Search
-
The Expanded Role of OBGYNs in Women's Healthcare
Obstetrician-gynecologists (OBGYNs) see patients from menses (the monthly menstrual cycle that occurs as a part of the female reproductive system), pregnancy and childbirth through menopause and play a pivotal role in managing reproductive health and overall wellness. Dr. James Alexander with Renown Women's Health explains. "As experts in women's health, we are uniquely positioned to recognize subtle changes or symptoms that might indicate broader health issues. This comprehensive approach allows us to serve as a valuable first touchpoint for various health concerns." Preventive Screenings: A Proactive Approach One key aspect is an OBGYN's ability to recommend preventive screenings based on your symptoms, age, lifestyle and medical history. For instance, lipid screenings are critical for monitoring cholesterol levels, which can be a significant factor in women’s heart disease. An OBGYN keeps up with the current guidelines for routine screening as well as in women with risk factors such as high blood pressure, diabetes, or a family history of heart disease during your visit. By identifying risks and abnormal screening early, they can collaborate with you to implement lifestyle changes or treatments to reduce your risk of heart conditions. Schedule Your Screening Appointment Make an Appointment by Phone: 775-982-5000
Read More About The Expanded Role of OBGYNs in Women's Healthcare
-
Understanding the Reasons Behind Heavy Menstrual Cycles
While menstrual cycles can be an annoying inconvenience for many women, heavy bleeding (menorrhagia) is not normal and can disrupt your life. A few days of heavy flow at the start of your period is usually nothing to worry about. However, if you’re frequently experiencing very heavy periods, you should discuss it with your gynecologist or primary care provider. Dr. Megan Fish, an OB-GYN with Renown Women’s Health, discusses various reasons, evaluation and treatment methods when it comes to heavy menstrual cycles. What is classified as heavy menstrual bleeding? The American College of Obstetricians and Gynecologists considers heavy bleeding to be any of the following signs: Bleeding that lasts more than 7 days. Bleeding that soaks through one or more tampons or pads every hour for several hours in a row. Needing to wear more than one pad at a time to control menstrual flow. Needing to change pads or tampons during the night. Menstrual flow with blood clots that are as big as a quarter or larger. What are the most common reasons for heavier periods? A variety of reasons why someone might have heavy periods. Fortunately, most of these problems are treatable. Because each woman's period is unique, only a doctor can definitively determine the cause of your heavy periods. Some of the most common issues that cause heavy periods include: Hormone imbalances such as anovulation, thyroid disease and Polycystic Ovary Syndrome (PCOS). Structural abnormalities in your uterus such as polyps or fibroids. Precancer and cancer such as uterine, cervical, vaginal, ovarian or endometrial hyperplasia. Infections such as chlamydia, gonorrhea, endometritis or vaginitis. Other medical conditions such as liver disease, kidney disease or Pelvic Inflammatory Disease. Medications such as blood thinners and aspirin, hormone replacement therapy, Intrauterine devices (IUDs), birth control pills and injectables. Pregnancy-related problems such as a miscarriage or ectopic pregnancy.
Read More About Understanding the Reasons Behind Heavy Menstrual Cycles
-
6 Healthcare Action Items for the LGBTQIA+ Community
Every patient, regardless of how they may identify, greatly benefits from preventive healthcare and early detection. Members of the LGBTQIA+ community face unique considerations when it comes to their health, and a proactive approach to preventive screenings and vaccines is important in order to address their individual health needs. Dr. Karen Thiele, Family Medicine Physician with University Health and Assistant Professor of Family and Community Medicine at the University of Nevada, Reno School of Medicine, breaks down key steps that LGBTQIA+ patients should take to safeguard their health. PrEP and PEP Pre-exposure prophylaxis (PrEP) is a strategy to prevent human immunodeficiency virus (HIV) infection. It is an important measure for those who are HIV-negative but may be at risk of contracting it. The highest risk sexual practice is receptive anal intercourse, due to the relative fragility of rectal tissue. This medication can stop HIV from spreading in the body and help patients maintain their HIV-negative status. PrEP is available in both pill form, which is taken every day, and injection form, of which the first two injections are initiated one month after another while all other injections are initiated every two months. Post-exposure prophylaxis (PEP) is an antiretroviral drug regimen taken after potential HIV exposure to prevent an HIV-negative individual from converting to HIV-positive status. PEP is only for emergency situations and must be started within 72 hours of exposure – sooner is always better than later – and must be taken for 28 days. PrEP and PEP are available in many ways, including visiting your primary care provider (PCP) or an urgent care location. HPV Immunization All genders and identities can protect themselves against human papillomavirus (HPV), a sexually transmitted infection (STI) that can lead to the risk of cervical, mouth, head, neck, throat, anal, vaginal, penile and vulvar cancers. HPV is so common that nearly all sexually active people, regardless of sexual orientation and practices, will be exposed at some point in their lifetime. The HPV vaccine (common brands include Gardasil and Cervarix) is a safe and effective method to prevent HPV, according to the Centers for Disease Control and Prevention (CDC). This vaccine protects against infections that can lead to HPV-related cancers and precancers, as well as genital warts. While patients should start receiving the vaccine at 9 years old years old, unvaccinated adults up to the age of 45 can also receive the vaccine through their PCP – better late than never! STI Testing Sexually-transmitted infections form from bacteria, viruses or parasites that can be transmitted by person-to-person sexual contact through semen, vaginal, blood and other bodily fluids. According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new STI cases across the nation each year. Luckily, most STIs are preventable. Annual STI testing for HIV, gonorrhea, chlamydia and syphilis is important to stay on top of your sexual health. Because these STIs may sometimes have no symptoms, screening is recommended regularly and with any change in sexual partners. Depending on the specific condition, tests for these infections include urine, swab and blood tests. Speak with your primary care provider on a screening schedule that works best for you. Prostate Exams Prostate exams look for early signs of prostate cancer in patients who still have a prostate. The CDC recommends those who are at least 55 years old get regular prostate screenings; however, for patients with a family history of prostate cancer, screenings may be recommended as early as 45 years old. These exams are done via two common methods – a prostate specific antigen (PSA) blood test and a digital rectal examination (DRE). Your provider can help you determine your risk and when you should start getting screened. Pap Tests and Pelvic Exams Patients of all genders who have a cervix, uterus, vagina and/or ovaries will benefit from regular pelvic exams and Pap screenings. A pelvic exam consists of a provider looking inside the vagina and at the cervix for anything unusual. A Pap test, also known as a Pap smear, involves your provider using a small, soft swab to collect cervical cells to check for early signs of cancer. Generally speaking, people with these organs should have a Pap test every three years starting at age 21 through the age of 30. After age 30, patients should receive a Pap test with HPV co-testing every five years until age 65. These recommendations are changing based on new research, so it is important to have a conversation with your PCP about the current guidelines so you can make an informed choice about what schedule you should follow. A gynecologist or your primary care provider can counsel you and perform these screenings. Mammograms and Breast Exams People with breast tissue, especially dense breast tissue, are at risk for breast cancer, and regular breast screenings are your best line of defense. At-home breast self-exams are the first step – you will want to check your breasts for any lumps, changes, fluid leaks, irregular tissue thickening or anything else that feels unusual. The Breast Cancer Risk Assessment tool, provided by the National Cancer Institute, is a good place to start to identify your risk. Talk with your primary care provider about the risks and benefits of starting screening at age 40 so you can make an informed decision about when to start. If you have any family history of breast or ovarian cancer, your PCP will offer you genetic testing for BRCA 1 and 2 mutations. Nevadans over the age of 18 can also get BRCA genetic test for free by enrolling in the Healthy Nevada Project. Mammograms are important screening tools, but for a significant portion of people with breast tissue, density of the breast tissue may make mammograms less helpful in detecting cancer. Your primary care provider can help you decide what additional imaging (such as breast ultrasound) might be best for you.
Read More About 6 Healthcare Action Items for the LGBTQIA+ Community
-
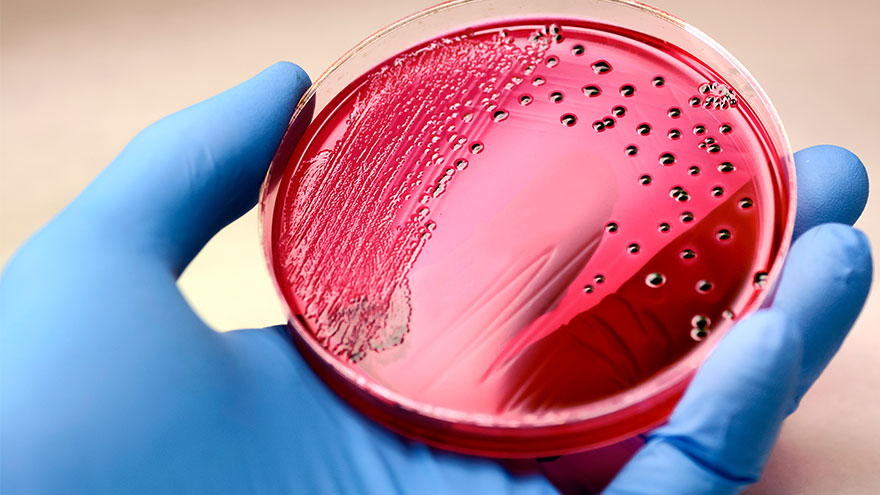
Sepsis: Causes & Symptoms
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.
-
Preventing Spinal Cord Injuries: What to Know
If you're not taking safety precautions during mountain sports, you could be at risk for a spinal cord injury. Dr. Benjamin Pence of Renown Rehabilitation Hospital explains the best way to prevent this serious injury. Mountain sports are a big part of the winter season here in our area, but if you’re not practicing all the proper safety techniques, you could end up with a serious spinal cord injury. Benjamin Pence, MD, Renown Rehabilitation Hospital, is here to offer tips to prevent this serious injury while you’re out enjoying what the Truckee Meadows has to offer. What is the spinal cord? The spine stretches from the base of your skull to the coccyx (commonly referred to as the tailbone). Your spine is made up of 24 vertebrae—seven cervical, which are in your neck, 12 thoracic, which are in your chest, and five lumbar, which are in your lower back. There are ligaments and muscles attached to each vertebra. These facilitate back movement and protect the bones from damage. There is cartilage between each vertebra which acts as a shock absorber for your spine. Finally, the spinal cord is a long, thin, tubular bundle of the nervous tissue and support cells that is enclosed in the spinal canal and send signals from the brain to everything from your arm and leg muscles to bowel and bladder function. The brain and spinal cord together make up the central nervous system.
Read More About Preventing Spinal Cord Injuries: What to Know
-
Your Ultimate Cold and Flu Survival Guide
While viruses can attack year-round, colds, flus and other respiratory illnesses are typically more prevalent during fall and winter. People spend more time indoors, which allows viruses to pass more easily from one person to another. The cold, dry air can also affect the respiratory system, making it more susceptible to germs. According to the CDC, flu activity in the U.S. often begins to increase in October and peaks between December and February. “Flu season” can last as late as May. When it comes to the cold and flu, prevention and preparation are key. Getting the flu shot and a COVID-19 vaccine is the first and most crucial step in protecting against these two respiratory illnesses. Preventative actions, such as washing your hands, covering your mouth and nose when coughing or sneezing and getting enough sleep can also help you avoid getting sick. However, despite your best prevention efforts, the time may come this winter when you start to feel a little scratch in your throat or a fever coming on. By taking steps ahead of time to assemble a cold and flu survival kit, you’ll be more prepared for whenever illness strikes, allowing you to stay home, rest and avoid spreading germs. Tips for Managing Symptoms Keep these tips in mind to ease your cold or flu symptoms: Stay home and rest Drink plenty of fluids Treat aches and fever with over-the-counter medication such as ibuprofen or acetaminophen Manage a cough with over-the-counter expectorants or suppressants Run a humidifier or sit in a steamy bathroom to ease congestion What to Stock in Your Flu Survival Kit Be ready when a cold or the flu strikes by having a flu survival kit filled with these get-well essentials stocked in your pantry, fridge and medicine cabinet: Over-the-Counter Medications: Take advantage of over-the-counter medications to make yourself feel better and ease most common flu symptoms of fever, headache, cough, muscle aches, sore throat, and runny or stuffy nose Pain relievers - Ibuprofen (Motrin and Advil) or Acetaminophen (Tylenol): for fever and aches Decongestants: for sniffles and congestion Cough expectorant (guaifenesin): for a “wet” cough to help clear secretions from the lungs Cough suppressant (dextromethorphan/DM): for a severe “dry” cough to block the cough reflex Cough syrups and drops Drinks: Water Herbal tea Low-sugar sports drinks Pedialyte Foods: Chicken soup Broth Vitamin C-containing fruits and vegetables Oatmeal Toast (add some avocado, honey or egg) Miscellaneous items: Tissues Lozenges Protective mask Thermometer Humidifier When to Seek Care and Where to Go Most healthy adults who have a cold, the flu, or other mild respiratory illnesses don’t need to see a care provider and will recover at home with self-care measures. Because these are viral illnesses, antibiotics won’t work against treating them. Your care provider may be able to prescribe an antiviral medication that can relieve your symptoms and shorten the duration and severity of your illness; however, this needs to be started within 48 hours of symptom onset and is often only prescribed to individuals at high risk for developing complications from the flu or those experience severe symptoms. Primary Care or Urgent Care Contact your primary care provider or visit an Urgent Care if you are at an increased risk, including those who: Are 65 years of age or older Have chronic medical conditions Are pregnant or recently gave birth Have a weakened immune system Find a primary care provider If you are otherwise healthy and not at increased risk of complications, seek medical advice if your flu symptoms are unusually severe, such as mild difficulty breathing, a severe sore throat, coughing that produces a lot of green or yellow mucus, or feeling faint. Emergency Care Go to the Emergency Department if you are experiencing emergency warning signs such as severe pain (chest, abdomen), concern for heart attack or stroke (slurred speech, new localized weakness), severe dehydration (needing IV fluids) or severe shortness of breath.
-
Department Spotlight: Customer Engagement Center
Do it for the patient. That’s the motto that each employee in the Customer Engagement Center (CEC) lives by every single day. This team spins all the existing stereotypical thoughts about call centers on their side by empowering and partnering with patients to achieve their best health. Being transferred around several times just isn’t in this team’s DNA – being a one-stop-shop for patient scheduling, referrals, insurance matters and more is how they proudly operate. Through elevating the customer engagement experience, the CEC closes care gaps to ensure patients get the right care at the right time. From employees who work from our home base in Reno, all the way to the southeastern corner of Florida, this primarily remote team stays firmly connected and collaborative to make patient care possible for all Renown Health patients and Hometown Health and Senior Care Plus members. The “Make It Happen” Department Back-to-back phone calls about a wide variety of patient needs? They make it happen. Referrals that need to go directly to the provider? They make it happen. Complex insurance questions that need to be resolved? They make it happen. The CEC is the keeper of all things customer service and all things patient satisfaction, leveraging technology to improve engagement and accessibility – and they wear that badge with pride. “Patient care is our first priority,” said Cindy Arevalo, Supervisor of Customer Engagement. “Even though we aren’t face-to-face with them, we are always there to help them over the phone with whatever their needs are.” The CEC has a lot of different sub-departments under its umbrella: scheduling, referrals, insurance, patient outreach, personal assistants, MyChart customer service and more. Each team handles calls for a different section of our health system, including the hospitals, imaging, primary care and specialty care. While their individual teams may be different, one aspect of their jobs remains the same: they care. Deeply. “We advocate for the patient, especially when they can’t advocate for themselves,” said Amanda Ishii, Referral Specialist. “We are the first people that patients speak to, and we all have empathy to listen to them, help them solve their problems and take as much time as they need to care for their needs,” added Susana Arroyo Garcia, Supervisor of Customer Engagement. Customer loyalty is key to the CEC. Every CEC team member builds strong relationships with patients and members. Whether they manage patient outreach or manage back-to-back inbound calls, each employee feels a special connection to the helpful work they do to solve a variety of patient concerns. “As Senior Care Plus Personal Assistants, for instance, we help guide our members through complex situations, and we eliminate the process of transferring them to different departments, becoming a ‘one-stop-shop' for them,” said Stephanie Perez Campbell, Senior Care Plus (SCP) Health Coordinator. “While every day is different, we are constantly learning new things and helping members navigate through the health system." With the 4.5 million calls the CEC handles per year, the nature of their jobs is undoubtedly fast paced. However, this does not intimidate the CEC team members; instead, it inspires them to continue reaching new milestones, helping thousands of patients and members every year by handling all the scheduling and referral work on the backend so that they can receive the care needed. “I never find myself sitting around asking, ‘what should I do next,’” said Gina Briles, Supervisor of Customer Engagement. “We always support each other to stay on top of it all in order to take care of our patients.” By wearing a lot of hats and managing many different work queues all while staying engaged with each patient, the CEC is full of natural problem-solvers, helping our healthcare network run smoothly. “The Engagement Center is the front door for the community; serving as the voice of the customer, we ensure patients do not fall through the cracks of the complex healthcare system and are able to easily access the right care at the right time through an exceptional experience,” said Candace Dietrich, Director of Customer Engagement. Consistently Connected With thousands of referrals to process and millions of calls to field, the ways the CEC stays connected to patients and members as well as each other can be related closely to magic. No concern goes unnoticed, and no problem is too complicated. “The sheer volume of patients we engage with is incredible,” said Rene Jacinto, Manager of Customer Engagement. “We processed nearly 200,000 referrals and authorizations last year.” “We expect a steady increase of calls year-over-year. My team processed 1,259 referrals in one day alone recently,” added Arielle Gomes, Referral Specialist. A superpower that every CEC team member holds is the ability to listen. According to this department, active listening is key when problem-solving with every patient and member, as that skill helps them anticipate patient needs and resolve their issues quickly and efficiently. “I’ll always listen,” said Alex Gomez, Customer Engagement Representative. “I want them to know that they are in good hands, especially when they are feeling scared or frustrated.” Team members like Alex help carefully guide customers through the Hometown Health and Senior Care Plus enrollment process, increasing membership and engaging patients to find the perfect plan for them. One of the largest challenges the CEC faces is the departures and arrivals of providers. The ebbs and flows of all hospital systems include provider departures and shifting provider availabilities. Despite this challenge, the CEC staff work hard to ensure communication with all patients regarding provider changes is consistent and that all patients are scheduled in a slot that works for both their schedule and the provider’s schedule. “It’s important for us to be flexible, because things can change at a moment’s notice,” said Gina Briles. “This is more than just a job – we are here for our patients. What we are doing impacts everyone.” Throughout all times of transition, the CEC builds robust relationships with both patients and providers within our organization and community, a skill that this team emphasizes as “fundamentally important.” For example, SCP Personal Assistants like Stephanie Perez Campbell will coordinate care with community resources and offices, giving members one less call to make and one less hurdle to cross in order to get the care they need. On top of it all, even though this team has the ability to work from all 50 states (and many of them work outside of Nevada!), every employee feels connected to their colleagues and their work. “This is the best group of people I’ve ever worked with,” said Riley Petro, Manager of Customer Engagement – Imaging. “I am super lucky for this job and am so thankful for these people.” Proud and Powerful The proof is in the pudding – or rather, the proof is in the numbers. Within the 4.5 million calls they successfully field every year, approximately 1.6 million of those calls route through the private branch exchange (PBX) team – the team that oversees the main operator lines – under the guidance of Jess Nater, Supervisor of Customer Engagement. The CEC is also on track to handle nearly 300,000 referrals this year alone. Additionally, the Hometown Health CEC team was recognized nationally this year with a five-star rating from Medicare. “We all have the initiative to grow, and because of this, we are always learning something new,” said Cindy Arevalo. “Our leaders also support our growth, especially if we want to skill-build or advance in our careers.” The CEC is frequently the first stop on the career ladder for many employees as they start their journey in healthcare, and CEC leadership is committed to the growth and development of their teams to reach their career goals at Renown. The secret formula for all this success can be in part attributed to the pride each CEC employee has for their team, their work and Renown. “We have a very supportive team,” said Holly Coffey, Supervisor of Customer Engagement. “I’ve seen our leaders support their teams tremendously.” “We rely on each other,” added Ashleigh Carty, Customer Engagement Representative. "I love the relationships we create with one another.” Employees in the CEC come from many walks of life, choosing to work at Renown and Hometown Health for a variety of different reasons, many related to the positive power our health system holds. Team members in this department hold a myriad of different career backgrounds, including pharmacy technicians, medical assistants, population health professionals, community health workers and more. Some team members, like Nikki Clifford, Customer Engagement Representative Lead, heard wonderful things about Renown from her mother, who also works for Renown. According to Nikki, “seeing how happy my mom has been in her career made me want to join too. I’ve loved it here ever since.” Katie Lunau, Supervisor of Customer Engagement, also grew up in a family involved in healthcare, and she wanted to follow in their footsteps. Choosing Renown as the place to follow her family path was a simple one, because “Renown stood out as the company that was actively involved in the community helping others.” For other team members, like Susana Arroyo Garcia, Ashleigh Carty and Stephanie Perez Campbell, Renown and Hometown Health’s impact on the local healthcare landscape was their primary driver for choosing a career here and in the CEC specifically. “Renown is very well-known in the area,” said Stephanie Perez Campbell. “I went to school in Reno for public health, so Renown came up all the time in my schooling. I knew Renown had a lot of different opportunities available for career growth, and with the friendly environment I always experienced here, it was an easy decision.” “Once I went through the interview process and joined the team, I immediately realized that there are outstanding managers, support systems and communication skills here. People genuinely care,” added Ashleigh Carty. Ashleigh is exactly right. As emphasized by every team member, employees in the CEC care. Their heightened levels of care and empathy set the bar high for all at Renown and Hometown Health, and their impact will be felt for years to come.
Read More About Department Spotlight: Customer Engagement Center
-
Prevention Against STIs Matters
According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new sexually transmitted infection (STI) cases in the United States each year, with rates continuing to increase. What you may not know is most STIs are preventable. We talked with Renown Adolescent Medicine Specialist, Caroline Barangan, MD to learn more about STIs. How Can You Get an STI? The CDC (Center for Disease Control) says that STIs are acquired through sexual contact. There are bacteria, viruses or parasites that can cause an STI which may pass from person to person in blood, semen, vaginal and other bodily fluids. How Do You Know if You Have an STI? STIs can have a range of signs and symptoms such as: Warts, bumps or sores on or near the penis, vagina, mouth or anus Swelling, redness or severe itching near the penis or vagina Discharge from the penis Vaginal bleeding that’s not your period Painful or uncomfortable sex Vaginal discharge that has an unpleasant odor, causes irritation or is a different color or amount than usual Weight loss, diarrhea or night sweats Aches, pains, fever and chills Jaundice (yellowing of the skin and whites of the eyes) Painful or frequent urination Sore throat if you engage in oral sex It’s important to know that the majority of people who have an STI commonly have no symptoms at all, which is why it’s important to get regularly tested once you have had any sexual activity. Young people less than 25 years of age should be screened on a yearly basis at minimum.
-
Type 2 Diabetes: What You Should Know
Type 2 diabetes, formerly known as adult-onset diabetes, is on the rise for adults and children in the United States. Although genetics play a role, you can take steps today to lower your risk of developing this life-altering condition. Michael Raymund Gonzales, MD with Renown Endocrinology answered our questions about Type 2 diabetes and gave us some useful tips for prevention. What effect does diabetes have on the body? And who’s most at risk? First, it’s important to know the difference between the two most common types of diabetes: Type 1 diabetes is the result of the body’s inability to make insulin, which is a hormone your body needs to be able to use sugar, or glucose, for energy. Type 1 is not preventable, and people who have it were either born with it or they developed it later in life due to an autoimmune process that attacked the pancreas that went unrecognized. Type 2 diabetes occurs when the body makes the insulin hormone, but it might not make enough or work well enough for the body to use sugar for energy. This is called insulin resistance. This condition usually develops later in life but is preventable with proper diet, exercise and weight loss. However, due to the obesity epidemic, type 2 diabetes is occurring more often in younger individuals. Diabetes hurts the body’s ability to break down glucose, so rather than it being used for energy, glucose stays in the bloodstream, which can cause problems. But with early detection and the help of your doctor, diabetes can be managed so that complications are avoided. Left unmanaged, however, diabetes can affect major organs and lead to heart and blood vessel disease, nerve damage, kidney damage, eye damage, skin conditions and more. Type 2 diabetes also results from risk factors that you can’t control, including your family history, race and age. However, there are a few risk factors that you can watch out for, such as being overweight, inactivity, diet choices, having high blood pressure and high cholesterol and triglycerides.
-
Meet Gabby, Renown Regional ER Nurse and Miss Rodeo Nevada
Renown Health is proud to embrace the Reno-Sparks culture that makes our community stand out, which is why we sponsor the Reno Rodeo, an early summer staple with roots in the community as deep as our own. One of our many ties with the Reno Rodeo includes Renown Regional’s own emergency room nurse and Miss Rodeo Nevada 2022, Gabby Szachara. A Reno native, Gabby developed a love for the Reno Rodeo at a very young age. “I loved watching the girls on the Reno Rodeo Flag Team when I was little and knew I wanted to be part of the Reno Rodeo someday,” said Gabby. “As I got older, I started to make connections and build relationships with some people in the rodeo scene, and they generously lent me their horses so I could participate in the Reno Rodeo Flag Team.” Gabby was on the flag team for three years before being crowned Miss Rodeo Nevada 2022 last year. Before joining the Reno Rodeo Flag Team, Gabby was a student at the University of Nevada, Reno, and a member of the women’s volleyball team. In December 2017, she graduated with a bachelor’s degree in public health. At first, Gabby was interested in a career in sports medicine – it made sense with her background in athletics. But, after working in the medical field as a certified nurse assistant and an emergency medical technician, she grew passionate about patient care and decided she wanted to become a nurse. “I’ve always loved teamwork and helping others,” said Gabby. “It’s important to me to be there for others, especially when it might be their worst day.” In December 2021, Gabby graduated from Truckee Meadows Community College with a nursing degree and joined Renown Health this February. “I love Renown for various reasons. Everyone here is so nice and welcoming, and there is a great team dynamic,” said Gabby. “And I love that Renown’s main color is purple because that is my favorite!” When Gabby isn’t in her scrubs and caring for patients, she is in western wear and carrying out her duties as Miss Rodeo Nevada. “I do a lot of traveling across the country to attend other rodeos,” said Gabby. “I enjoy meeting so many wonderful people and experiencing the culture of different states.” Gabby’s main goals as Miss Rodeo Nevada are to promote the western way of life, agriculture, rodeo and community benefit. In addition, she visits local schools to talk with kids about how they can get involved in these areas and inspires them to turn their dreams into reality. Gabby has a special place in her heart for the Reno Rodeo. “Reno is my home, and the Reno Rodeo is the heart and soul of summer in northern Nevada. Everyone comes together and dusts off their boots to have fun and also contribute money to important causes in our community,” said Gabby. “I love the comradery, the friendly and healthy competition and the great people.” If you’re going to the Reno Rodeo this weekend, watch for Gabby and her horse, “Torque.” And if you see Gabby in the halls at Renown Regional, give her a high-five for all her hard work as a nurse and Miss Rodeo Nevada!
Read More About Meet Gabby, Renown Regional ER Nurse and Miss Rodeo Nevada
-
Make Hydration a Priority for Your Health
As the temperatures skyrocket and we return to more outdoor activity, one thing is certain: you must hydrate to stay cool, healthy, and functional. But how much water do you need, and what are some easy ways to ensure you are getting enough? Aurosis Reddy, DO a family medicine provider with Renown Medical Group, shares what you need to know. How Much Water Is Enough? Experts agree that recommended daily water intake can vary depending on different factors such as your weight, metabolism, location, diet, physical activity, and health. As a rule of thumb, women should aim for a daily fluid intake of 91 ounces, and men should aim for 125 ounces. It is important to listen to your body and recognize when you might need to increase your water intake. For example, if you’re partaking in strenuous exercise, or spending time outside in the heat, you’ll want to give your body more water and electrolytes to function properly. How Can I Tell If I Am Dehydrated? Decreased coordination Fatigue Less urination Dizziness Dry, sticky lips and mouth Increased thirst Headache
-
Paola’s Story: Bringing Hope and Determination to Patient Care
You may recognize her from billboards around town or the cover of Renown's latest annual report, but what you might not know is the story behind the now-familiar face. Paola Espinoza-Patino is the oncology unit's associate nurse manager at Renown Regional, and she grounds her work in hope and determination daily. Meet Paola:
Read More About Paola’s Story: Bringing Hope and Determination to Patient Care