Search
Results for 'careers'
Clear-
Department Spotlight: NICU Transport
Bringing in new life is an exciting and beautiful occasion. The possibilities for the newest members of our world are endless – what will the child grow up to become? What will they achieve in their lifetime? Anyone will agree that a new life is precious and protecting that life by any means possible is a necessity. Sometimes, however, a baby’s journey into our world brings along obstacles. Prematurity, congenital defects and other complications can accompany a birth and the baby’s first few moments of life. But what happens when these complications happen outside of a fully-functioning Labor & Delivery unit, or if the complications need a special level of intervention with a health system capable of caring for their unique needs? Enter the NICU Transport team at Renown Health. As the only Neonatal Intensive Care Unit (NICU) Transport team in northern Nevada, these dedicated nurses, respiratory therapists and neonatal nurse practitioners – who have normal unit duties of their own at Renown Regional Medical Center – step up to the plate to take on this extra duty to support members of their community facing some of the scariest moments of their lives. To them, transporting babies in critical condition and giving them the best chance of life isn’t just a responsibility; it’s a calling. The NICU on Wheels When the Saint Mary’s maternity unit, which was Renown’s partner in NICU transport duties, made the decision to close, our dedicated NICU nurses and respiratory therapists diligently rose to the occasion to fill the demand. Dubbed the “NICU on Wheels,” Renown’s team went from taking on transport duties every other day to 365 days a year – and they are always ready to go at a moment’s notice, whether it’s by ambulance or by fixed-wing aircraft. “When we learned about the closure we knew it was our calling and knew we had to step up,” said Rachel D., Neonatal Transport RN at Renown. “We still have regular days on the floor, and we each switch off being on-call for transport. Once we get a distress call, we have 30 minutes to get to the hospital, grab our gear and go. We have to essentially put a whole room’s worth of portable equipment in one bag.” “I really enjoy being a part of the transport team and making a difference from northern Nevada to northern California,” added Sam V., Supervisor of Respiratory Care at Renown. “We are able to practice at the top of our skill level and use autonomy that not every practitioner gets to use.” Each NICU Transport unit works in teams of three when heading out into the field: one nurse (our bedside experts), one nurse practitioner (our education experts) and one respiratory therapist (our lung and breathing experts). With several years – and in many cases, decades – of experience in NICU nursing, NICU transport duties and respiratory therapy, this team is poised to provide state-of-the-art lifesaving care en route to the hospital. This diverse array of experiences among the team especially comes in handy as they continue to face the increased transport workload. “We are so thankful to have Saint Mary’s employees come over and work on our team after their maternity ward closed,” said Melyssa H., RN, NICU Transport Coordinator at Renown. “Helping the babies, as well as helping the scared families, will always be our top priority.” “I love the complexity that babies provide in the NICU,” added Jennifer J., Neonatal Transport RN at Renown. “Providing hands-on care right at the bedside along other members of the team is such a rewarding experience.” Education is also a crucial tool in NICU care, especially in the field. The nurse practitioners on this team make it their mission to outreach to the community, including our rural health partners, and help them build the tools and skills they need to care for our smallest and most critical patients. “I have been on a few transports where we went out and did not have to bring the baby over to the hospital, and we were able to provide lots of education instead,” said Shiela A., Respiratory Specialist at Renown. “For instance, I was called out to Fallon for a baby that was in respiratory distress. When we arrived, we saw the baby was awake and active although intubated. The tube came out, and we retaped it. While we stayed to observe the baby to make sure everything was okay, the nurse practitioner on the team provided educational tools to the family on what they can improve on regarding their baby’s tubing. Our nurses do such a great job with these teachings.” “When I started, I quickly noticed that more education was needed in the field,” added Jennifer J., RN. “Now I see the momentum we’ve had in these communities really take full force. Because of this education, and the confidence we instill in our patients’ families, each baby’s transition to our team has become so much easier. It has been awesome to watch this progress over the years.” With immense experience, education and a strong commitment to their community under their wing, the NICU on Wheels is only just getting started. Teamwork Makes the Dream Work Running a successful NICU Transport operation, especially as the sole health system participating, takes a village. With only three professionals out in the field, the team leans on their fellow nurses, physicians, surgeons and specialists to make the operation run as smoothly as possible. From REMSA and Care Flight helping load patients in and get them to the hospital safely, to Renown’s Clinical Engineering team who are first on the scene when machines need repairs and troubleshooting, everyone rises to the occasion to achieve the best-possible outcome for our youngest patients at some of the most challenging moments of the beginning of their lives – and they are fully trusted to move those mountains. “Being a part of the NICU Transport team has given us the opportunity to facilitate a deeper, meaningful relationship with providers and a patient’s entire care team,” said Rachel D., RN. “They entrust us with our assessment skills, opinions and skill levels. There is an equal layer of trust between us and them.” Despite the pressure they feel every day, the NICU Transport team never let it overtake them and instead let it empower them. “We are under a lot of pressure and stress regardless of the case, and yet, we all work so well together; the teamwork really is incredible,” said Lisa A., Respiratory Specialist at Renown. “I am very proud of how our team steps up and is very intricate, even down to organization. For example, team members like Shiela arrange all the respiratory bags and make sure they are laid out in a way that makes the procedure as simple as possible to ensure there are no complications.” The nurses and respiratory therapists also partner together on the NICU floor and are always ready to provide coverage when their transport colleagues get a call. Committed to collaboration and ready to jump into action, the NICU Transport team works together to elevate each other and the bottom line for each patient. “This is a full-time gig, and the group works together to make sure everyone is covered; we are all very collaborative,” said Sarah K., Respiratory Specialist at Renown. “We all think of our patients as extra special, and it’s nice to know that you can make a difference in the baby’s life and the lives of the family. We all have a sense of purpose in giving back to the community.” “I am just so thankful to be a part of this team,” added Marcia A., Neonatal Transport RN at Renown. “We really have developed a strong bond.” A Track Record of Success The life-saving measures that each member of the NICU Transport team take surpass hospital walls. The impact they have on each baby are remembered and celebrated for years, and they often develop lifelong relationships with patients and their families after their stay in the NICU. One prime example of this can be found in an impassioned letter from Tess, the mother of a young boy who was in the midst of respiratory distress and needed immediate intervention. Because of the valiant efforts of Renown’s NICU Transport team, her child, Warren, is a healthy and happy baby to this day. She recalls the experience: Warren had stopped breathing while getting routine blood work. He was resuscitated twice while at an area hospital. We made the decision to transfer him to Renown for him to be admitted into the NICU. Within an hour and a half of this decision, Renown had sent a team consisting of a respiratory therapist, nurse and nurse practitioner to come and get him. As soon as the team entered the room, we immediately felt safe and comforted. The team made sure we knew exactly what was going on and what was going to happen in the following hours, and they let us know they would do everything for Warren. He was resuscitated two more times by the respiratory therapist while getting ready for transport. At that time, the decision was made to intubate for a smoother ride to Renown. We knew you all had his best interest in mind, and of course, we trusted you with everything. The intubation went well, and he was packed up and ready to drive. Today, Warren is hitting all of his developmental milestones and is a normal, happy baby in everyone’s eyes. We can’t thank the NICU Transport team enough for taking such good care of Warren and helping him Fight the Good Fight. “This success wasn’t just due to our three-person unit – our manager, Jason, also jumped in and drove all the way to Carson City to stabilize the child,” said Shiela A. “This just goes to show that no matter our title, we are always here to help and make a huge difference in the lives of our patients.” Success stories of children like Warren describe the common mission of the NICU Transport team in detail, and while there are more of these stories to come, the team is always ready to make the necessary sacrifices for the greater good of their patients. “Sarah K. is like Warren’s guardian angel,” said Tess. “We call her ‘Auntie Sarah’ now. He wouldn’t be here if it weren’t for her and the entire NICU Transport team. It takes a special kind of person to work in the NICU. I can never repay this team for what they’ve done for Warren and our family.” “I am proud of this team, their flexibility and the sacrifices they have made to do transport 365 days a year,” added Melyssa H., RN.” The remarkable success of the NICU Transport team serves as proof of the unwavering and tireless commitment of each and every team member, bringing hope to families during their most difficult moments. “NICU Transport forces you to be confident in yourself and your abilities and to push yourself a step further,” said Rachel D., RN. “I am a better nurse because I joined the transport team.”
-
Department Spotlight: Surgical Preadmission
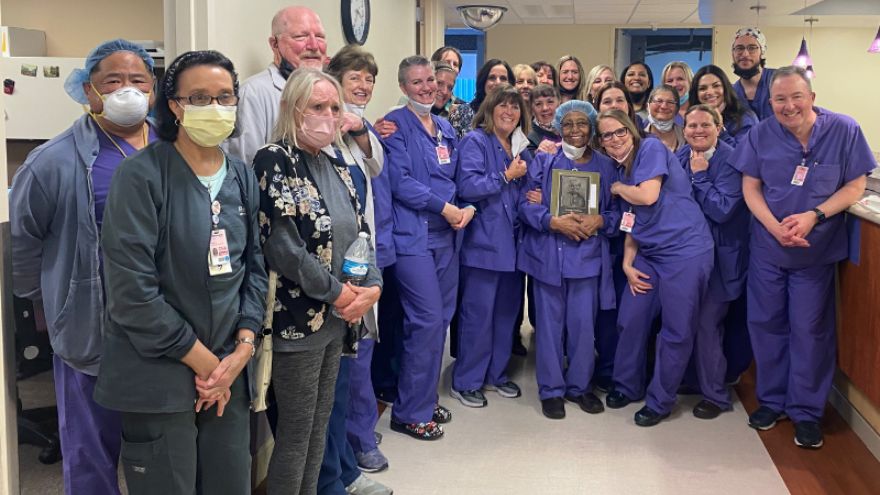
Heading into surgery of any kind can bring along feelings of intimidation. With a best-in-class surgery team at Renown Health, patients rest assured that they are in the most capable hands for their entire procedure from start to finish – and while the physical preparation is vital, mental and emotional preparation is equally as important to ensure each patient has a smooth and comfortable experience. The Surgical Preadmission department (a.k.a. “preadmit”) at Renown Regional Medical Center and Renown South Meadows Medical Center is a dynamic and compassionate group of nurses, case managers, chart managers and more who are dedicated to guiding each patient through the surgical process. With extensive knowledge and expertise under their belt, the teams are equipped to make a genuine difference in the health and well-being of all patients, for all surgeries, at all times of the year. Surgery Starting Ground The Surgical Preadmission teams are crucial aspects in the successful outcome of every surgical procedure. Comprised of skilled healthcare professionals, this department is dedicated to providing comprehensive support and care before heading into the pre-operating room. “Our job is to prepare every patient for surgery, make sure all their pre-surgery testing is done, ensure they understand their fasting and medication instructions, have had their questions answered, have a ride home and know what to expect during surgery and after so their recovery can go smoothly and without complications,” said Debra Bennett, RN, Supervisor of Surgical Preadmission at Renown Regional. “Each patient is unique, so each experience is different.” Our preadmit nurses are the masters of communication, directing thorough assessments – including medications, tests and clearances – and addressing any questions or concerns patients may have, never missing the opportunity to inform them of exactly what they will expect in surgery. “I do a complete history on every patient while giving them detailed pre-operating instructions and helping them answer any questions to the best of my ability,” said Nancy Hilts, Surgical Preadmission RN at Renown Regional. “I am proud to be able to help allay their fears and concerns using my 30 years of pre-op experience. I offer an avenue for them to feel comfortable opening up to me.” “We always tell patients that they have great surgeons and a fantastic team that will be watching over them and taking care of them every step of the way,” added Jon Capallupo, Surgical Preadmission RN at Renown South Meadows. “We also give them plenty of educational handouts and video content, in addition to verbal instruction, to ensure they are as prepared as possible.” The nurses then pass the reigns onto the chart managers, who prepare the charts for surgery and ensure all documentation is up-to-date before sending them to the pre-operative team. The expert surgical case managers also step in to prepare a thorough discharge plan, along with reviewing pre-operation orders for status, consent, codes and more. The team does several of these initial visits virtually, and they are looking forward to soon phasing all preadmit case manager preliminary visits into a virtual model. From assisting the pre-op and post-anesthesia care unit (PACU) teams with discharge planning concerns to helping on the outpatient side with anything from oxygen equipment and catheters to transportation issues and those experiencing homelessness, our pre-admit case managers are always up to the challenge. "We are true patient advocates, alleviating concerns and fears along the way,” said Mary Carl, RN, Case Manager at Renown Regional. “Just to name a few things we do on a daily basis, we see our total joint and non-weight bearing patients during their preadmission appointment, so they are aware of the medical equipment they need and if it is covered by insurance; provide education for Aspira catheters and gastrostomy tubes; advocate to ensure tube feeding and dressing changes are set up for hospice and home health patients; and escalate concerns of patient safety to ensure a safe discharge.” In the midst of it all, there is never a dull moment in the preadmit teams. At Renown Regional alone, the preadmit professionals see more than 1,600 patients a month – and each one has a hyper-personalized experience with their very own preadmit team. “Many times, we are the first impression a patient has on our organization; after all, we touch more than 97 percent of patients that are scheduled for surgery, cardiac catheterization lab procedures or interventional radiology,” said Amy Schler, Surgical Preadmission RN at Renown Regional. “We also collaborate with many other departments in the hospital as well, from surgeons and anesthesiologists to case managers and nurse navigators. Our work in preadmit impacts the entire surgical process.” Holding a diverse array of experiences, our preadmit department plays an integral role in our commitment to providing the highest quality of care to every patient. Knowledge is Power Heading into surgery feeling fearful and worried is normal for any patient. However, how would you feel knowing that each individual member on your preadmit team has, on average, 23-25 years of experience in the field? This is the reality for our Surgical Preadmission department – and they put that vast knowledge to great use to bring a sense of calm to patients. “Our team members have worked in various departments within our organization, and they bring a wealth of knowledge that we share with each other, and most importantly, with our patients,” said Amy Schler, RN. “If you have hundreds of years of nursing experience, you can speak not only as a nurse but also as a patient. It allows you to give a more personal perspective on what patients can expect in their recovery. Being able to assess their emotions and provide feedback to our pre-op and PACU teams help the patient have a better experience.” “Many of our nurses have close to 40 years of experience each, and they have an extremely large knowledge base since we see patients from newborn to geriatric and from easy procedures to complex surgeries,” added Debra Bennett, RN. “Another great aspect of our team is the varied nursing backgrounds we all hold – surgery, pre- and post-op, labor and delivery, pediatric intensive care, cardiology, gastroenterology, urology, cardiac cath lab, home health and everything in between. Communication between departments is so important!” All members in this department, regardless of which clinical area they came from, surgical or non-surgical, can easily translate their skills into the work they do in preadmit – and they only continue to grow. “As a surgical preadmission nurse, I have used my years of experience as a nurse in surgical services,” said Terri Delatorre, Surgical Preadmission RN at Renown Regional. “I started as a floor nurse with orthopedics for 12 years, and then I worked with the PACU for 11 years. This has helped me give great understanding and care to our surgical patients.” “Because we have staff with such a vast knowledge base, we can rely on our years of working within our organization to help alleviate fears that the patient may have,” added Amy Schler, RN. We can prepare them for what to expect in pre-op and PACU and educate them on what to expect post-op, including any barriers they may face. For example, mastectomy patients may not realize they will not be able to raise their arms for 7-10 days post-op, and total knee patients have to navigate stairs and housing access. Helping patients think about barriers at home that they may not have thought about helps them prepare prior to surgery, enhances their healing and provides a better surgical experience.” The preadmit team works closely with our best-in-class surgeons and anesthesiologists, continuing to grow their expertise along the way while learning alongside our talented providers. For instance, when it comes to our Renown South Meadows preadmit department, anesthesiologist Nariman Rahimzadeh, MD provides excellent guidance for the entire team on state-of-the-art anesthesiology practices. “I am very proud of the work we do with Dr. Rahimzadeh,” said Lisa Closson, Surgical Preadmission RN at Renown South Meadows. “Together, we ensure patients are safe for both surgery and anesthesia.” Despite the challenges that come their way – whether it be changes to process and workflow to navigating support for patients after they leave the surgery floor – the preadmit team cleverly uses their collective wealth of knowledge to bring hope and comfort to all patients. “Our nurses are such warm, caring and compassionate humans that do their best to ease any fears and anxieties patients may have,” said Debra Bennett, RN. The Pride of Preadmission The pride of our preadmit team lies in their ability to make a positive impact on all patients they serve. To them, their work is not just a job – it's a calling. And they do it all while working together to elevate their team and performance. “Our team is most proud of the quality of care we provide to our patients and our abilities to troubleshoot difficult situations to ensure they have a great surgical experience here at Renown,” said Mary Carl, RN. The entire department supports each other by working collaboratively and relying on each other’s expertise to provide the best possible care for patients. They understand that their success as a team depends on their abilities to support and help each other. “Our team is awesome here at South Meadows,” said Jon Capallupo, RN. “We can turn to each other for support, and we all work very well with each other. I am glad to be a part of this team.” “I am proud of how well all of us in preadmit works with each other every day,” added Lisa Closson, RN. “We try to make patients feel comfortable from the moment they arrive to the time they leave the department.” The pride that our preadmit team expends goes beyond their departmental limits – these team members are also trusted teachers. They work closely with cancer nurse navigators to teach weekly classes for patients who have been newly diagnosed with breast cancer, coupled with lymphedema prevention and education classes. The team also encourages participation in Renown’s free smoking cessation programs to help their patients learn the risks and benefits of quitting smoking. When not serving patients or teaching classes, you can find many of these team members taking charge of multidisciplinary committees within our health system, including breast leadership, gastroenterology leadership, shared governance, infection control and recruitment and retention. On top of it all, this team certainly knows how to celebrate, with several of their members being a part of their own department-wide Celebration Committee, where they gather for retirement parties, baby showers and team get-togethers. Always active and never passing up a challenge, our preadmit department are shining examples of Renown’s Culture Commitments, especially Caring and Collaboration, and the pride in the vital work they do every day is limitless. “I am so happy my position in preadmit opened up for me at a time when I was really feeling challenged in my career,” said Nancy Hilts, RN. “The team that we have here is amazing. I am so grateful and thankful every day for the opportunity. It is an amazing place to work!”
-
Department Spotlight: Wound Care
For the average person, wounds aren’t an everyday worry. However, for at least eight million Americans, chronic wounds can pose a serious threat to health and well-being. From a person with diabetes experiencing painful neuropathy to a patient healing from a significant burn, caring for advanced wounds is a major part of their healthcare journey. Who do they go to get the care and guidance they need? The answer: Renown Wound Care. Serving patients in both the inpatient and outpatient settings, this department provides comprehensive, best-in-class treatments for severe and chronic wound healing and ostomy care. Our Wound Care team members have mastered the art of harnessing cutting-edge technologies and a patient-centric approach to redefine the standards of healing. Advanced Care for the Best Repair At Renown Health, we are fortunate to have a team full of nurses, physicians and more caring for patients with wounds caused by a wide variety of conditions. Those include: Burns Trauma Vascular diseases Radiation therapy Pressure ulcers Diabetes and diabetic neuropathy Adding to the expert-level continuum of care, Renown is the only health system offering complete ostomy services in the entire region. The Wound Care team helps ostomy patients with the fitting of their medical bags, treatment of any skin conditions that may arise after ostomy bag placement, care coordination and much more. With a multidisciplinary network of experts tailoring personalized treatment plans, there is never a dull moment on the floor. On the outpatient side, the team expects 50-60 patients in one day alone. “As a clinician, wound care is a lot of ‘arts and crafts,’ so we get to use our creative and critical thinking skills to provide the best possible care,” said Samantha Moore, Advanced Wound Care Specialist RN for Outpatient Wound Care. “Each patient has an individualized plan of care – we greet them as they come into the clinic, escort them back to their treatment rooms and get their latest health updates and life situations before providing wound or ostomy care. We prepare each morning doing chart reviews to determine patient needs, wound progression and referral needs.” “We are a highly specialized, dedicated group of professionals with a passion to treat and heal our patients’ wounds,” added Lori Conner, Advanced Wound Care Specialist RN for Outpatient Wound Care. “When a patient comes to our clinic for evaluation, they are given a dedicated appointment to thoroughly go over their medical and surgical history, medications and nature of the wound.” Switching over to the inpatient care team, they operate like a well-oiled assembly line, navigating different daily assignments with precision and flexibility. “On the inpatient side, our day starts in our office with triaging our consult list; after the triage process is completed, we get our assignments, which can consist of wound vacuum-assisted closure (VAC) patients, follow-up patients, ostomy education patients and new wound consults,” said Megan Uy, Advanced Wound Care Specialist RN for Inpatient Wound Care. “In the case of patients requiring wound VAC changes, we consider what kind of pre-medication for pain that they need. Although some patients may be seen on a time schedule, the day ends up flexible as patients are being seen by other specialties. This flexibility also benefits the patients, making them feel more empowered with their care.” “Each day in the inpatient setting, we get to our office and sort through all the new consults that came in overnight, and the charge nurse makes the assignment for the day,” added Madison Arlin, Advanced Wound Care Specialist RN for Inpatient Wound Care. “After the assignment is completed, each nurse is responsible for researching their patients and organizing their day, typically by priority – wound VACs and ostomies usually take top priority.” Now, how do these treatments actually work? This specialized field handles advanced methods of treating each condition, including: Biological skin substitutes Surgical debridement Advanced wound dressings Negative pressure therapy Pre-ostomy markings and education Offloading techniques, such as padding or dressing “Before starting treatments, we communicate with our nurses and providers to make sure that the patient is comfortable prior to wound care,” said Dianna Seo, Advanced Wound Care Specialist RN for Inpatient Wound Care. “After we see the patient, if there is a need for escalated care, we contact the provider for additional testing or consults. We continue to follow-up on patients that have severe wounds, wound VACs and ostomies.” In the hands of the Wound Care team, patients exit our hospital walls not only restored but also empowered, set on a trajectory for long-term healing. Your Expert Care Guides No matter the case or the severity of the wound or condition, patient care, comfort and communication always come first – before, during and after treatment. “Many of our patients have chronic needs, so we end up seeing them for several months, if not years in some cases; we stay up to date with their specific psychosocial needs and help remove barriers that would prevent their wounds from healing,” said Samantha Moore. “I enjoy knowing that my positive attitude can improve our patients’ days,” added Maddie Pauley, Patient Access Representative for Outpatient Wound Care. “When they’re routinely coming to appointments they might not enjoy, hearing them praise our team and give their thanks is one of the most rewarding feelings.” As a wound care patient, there can be a lot of unknowns when beginning their care journey. However, these team members carefully walk each patient through every step from beginning to end. “When we go to see a wound care patient, our team is very consistent about explaining to the patients what our role is and what we plan to do with their wound, and then we continue to actively communicate throughout wound care each step that we are doing as we are doing it,” said Madison Arlin. “We also encourage some of our patients to listen to music that they enjoy during the wound care, or we will cover their eyes with a cloth if they request so that they don't have to see their wound. Sometimes, we will ask the family to stay at the bedside to hold their family member's hand.” Education is crucial to ensuring each patient knows what to expect in order to care for their wound and understanding the stages of healing. Fortunately, this team is well-versed in the world of wound wisdom. “A lot of education is provided on the type of dressing we are applying, and if the patient is going to be performing their own dressing changes, we will go over the entire change with them and provide supplies for discharge,” said Megan Uy. “Additionally, there will be written instructions in their discharge paperwork. In the cases of wound VAC dressing changes, each step is explained to the patient before doing it, and we also go over discharge options and expectations.” “As a clinician who sees a lot of patients prior to having their ostomy placed (pre-surgical marking), one of the most important things we do is first sit with the patient and/or caregivers and talk about their fears, concerns, questions and goals,” said Samantha Moore. “We provide a lot of emotional support and education, helping identify community resources. For our wound patients, we spend a lot of time educating our patients/caregivers about how and why their wounds occurred. We try to connect with them on a personal level and help them identify ways to help their wounds heal.” To see a patient’s care journey from the second they enter through our doors to the moment they return home is one of the most rewarding feelings for the Wound Care teams. In fact, they’ve had the pleasure of treating patients for years and seeing their wounds almost completely heal. The team collectively values the successful healing journeys of their patients as their proudest achievement. “One of our team's greatest accomplishments was being able to see one of our long-term patients discharged with nearly resolved wounds,” said Megan Uy. “This patient had been in our care on-and-off for the past year with many hospitalizations and had complicated high-output enterocutaneous fistulas within his wound bed. These were incredibly hard to keep a dressing on successfully, and he often had issues with the dressing leaking. Eventually, we got a dressing that could remain intact until his next scheduled dressing change, and he was able to get surgery that fixed his fistulas. Being able to see him recover and heal his wounds was a very large accomplishment for us.” The admiration and compassion this team has for their patients also extends to each other. The cohesive way they work together only further benefits their patients, offering the best-possible collaborative care. “We have extremely skilled clinicians in our group that are not only incredible in the work that they do and the patient care that they provide but are also enjoyable to work with as well,” said Geane Weaver, Advanced Wound Care Specialist RN for Inpatient Wound Care. “There is something to be admired in each and every one of my coworkers.” “Our team is very close and supportive of each other at all times,” added Madison Arlin. “I feel very lucky to work with such an amazing group of people. Our team is very proud of the work we do.” Fervently Fighting the Good Fight So, with the highly specialized nature of advanced wound care, how did these team members get inspired to join the Wound Care team in the first place? Well, for many of these devoted employees, their first exposure to caring for wounds took place on different units – sparking their interest in making wound care their full-time career. “Renown was the most welcoming towards me as a student nurse, and I liked that it was a teaching hospital,” said Madison Arlin. “I started in the General Surgical Unit (GSU) immediately after graduating nursing school and worked there for two years before transferring to wound care. I decided to apply to the wound team after watching the wound nurses do wound VACs and ostomy changes on the floor. I would ask them if I could watch, and I was always very fascinated by the wound healing process.” “Prior to joining the inpatient wound team, like Madison, I was also a bedside nurse in GSU,” added Geane Weaver. “Working on that floor, I was already exposed to a lot of patients that were requiring some kind of advanced wound care in one way or another. Working in the GSU, I also cared for a lot of patients that had wound VACs and ostomies. These patients make up a huge group of the individuals that our team sees on a regular basis, and they've always been intriguing for me, so naturally, wound care has always been on my radar.” For other team members, wound care has always been a point of curiosity throughout their education and career. From their very first exposure to this care area, they were hooked. “I was always curious about wound care even through my nursing school experience,” said Dianna Seo. “When I was working on the floor, I would trade to do wound care for patients. When I had time, I would follow wound care and help when I could. I joined the skin team which drove me to be increasingly involved with wound care. As soon as there was a job opening, I applied for the position. I worked in outpatient wound care for approximately four years and now inpatient for another four years. I have enjoyed all aspects of wound care and patient care.” “I had great clinical experience at Renown when I was in nursing school; I also was very interested in caring for trauma patients, and Renown being a Level II trauma center aligned with my interests,” added Megan Uy. “I began my nursing career in the GSU, but my dream job was always Wound Care. During my nursing school clinicals, I had the opportunity to watch some members of the wound team do wound VAC changes and thought it was incredibly intriguing and a great combination of utilizing the knowledge of anatomy and physiology while being creative with handicraft. A position opened on the team around the time I met the prerequisites to be eligible for the position, and luckily, I got it.” Our Wound Care team has achieved significant employee and departmental milestones over the past year, reflecting their dedication to enhancing patient care and overall process improvement. “We have had many accomplishments within the last year and are currently working on more to improve the hospital,” said Dianna Seo. “Madison Arlin won the DAISY Award for her great work with our patients. Megan Uy won Top Talent of the Quarter for helping a stranger. Ande Ferriera has worked tirelessly to improve our process improvement. Allie Saunders, as our leader, has worked to improve patient skin by getting new beds for Renown Regional. All our patients that have healed or are on their way to healing under our care is our greatest achievement that we as wound team is most proud of.” “We are constantly updating protocols, notes and orders for bedside nursing so that it is a more straightforward and seamless charting process,” added Madison Arlin. “We have representatives of different supply companies come and present new products that we think may benefit our patients better. Our wonderful tech has even updated our department site on Inside Renown so that the nurses always have references available.” Renown’s strong influence in the region – and the opportunity to give back to their community – was, and continues to be, a major draw for this team. “Since I can remember, Renown has always been the most prevalent healthcare name for my family and has always taken the most amazing, thorough care of my loved ones,” said Maddie Pauley. “I have always wanted to work somewhere I could help people, and starting at Renown has really opened my eyes into how much of a difference each one of us can make.” Our Wound Care department’s success stories and proactive approach not only reflect their passion for healing but also inspire a ripple effect of positive change throughout our health system. They proudly exemplify a shared commitment to enhancing the well-being of all patients under their care. “Being part of Renown and part of this team has been my blessing; I get to do a job I love with people that love it too,” closed Dianna Seo.
-
Department Spotlight: Labor & Delivery
Parents welcoming their new bundles of joy into the world might be overcome with emotions. They're exhausted yet excited to meet their new baby and hold them in their arms. That’s where Renown Health’s Labor & Delivery (L&D) department comes in. When patients arrive at the L&D unit in Renown Regional Medical Center, they are embraced with caring, compassionate nurses, surgical technicians and physicians ready to serve their family. As they get ready for the big moment in their private L&D room or family suite, you can be certain that you, they can be certain that they will receive the excellent care they deserve. Unpredictable, but Never Unprepared Ushering in new life can bring a lot of surprises for parents, but the L&D department is prepared for any challenge. Whether the unit is helping with a routine or high-risk delivery, every patient and newborn are treated with personalized care that is uniquely tailored to their own individual needs and birth preferences, from labor evaluation and birth to post-birth lactation consultation and navigating the nursery. “Our floor is never predictable,” said Bri Goode, Renown L&D nurse. “Our nurses and our staff work as a team to ensure the best care for our patients. I commonly say that we are all 'nurses’ for each patient!” The state-of-the-art technology at their fingertips – including advanced 3D ultrasound machines – coupled with the love and passion the team has for their patients allows them to create an optimal environment for every mother and baby. The unit is also equipped with a Labor Assessment Area, where expectant mothers are evaluated to determine what stage of labor they are in, removing the guesswork and allowing providers to treat the patient and unborn child more efficiently and meet them exactly where they are at in the labor process. Nothing can replace the careful guidance and words of encouragement a patient needs in the delivery room. The L&D department are true patient advocates and firmly believe in the power of listening and the power of staying calm and collected. “To help our patients and ease their fears and anxieties, we always ensure them that our biggest goal is to have a healthy mom and healthy baby,” said Lindsay Strowmatt, Renown L&D nurse. “We constantly reinforce that they are strong and capable. Empowerment goes a long way!” “We always take the time to actually sit down and listen to the patient, no matter how busy we are,” added Krystie Mortensen, Renown L&D nurse and DAISY Award winner. “It’s important for us to understand where their nerves are stemming from and address any changes in plan of care along the way.” While the L&D unit is seen as a “happy place,” as described repeatedly by the members of the team, a seemingly low-risk patient can also turn into an emergency in a matter of seconds. "Our line of work can involve high-stakes emergency care,” said April Tucker, Renown L&D nurse. “We view change as a necessary part of growth, and we save lives.” These steps result in high patient outcome scores, which can be attributed directly to the unit. “We have continually great outcomes from hard work and consistency in care,” said Roya Galata, Renown L&D nurse and Nursing Organizations Alliance (NOA) Lifetime Achievement awardee. “I have tremendous love for my patients and the type of work I do.” Awards Without End With patient safety and experience always top of mind, and with the team continually going above and beyond for all parents and their newborns, it’s no wonder why the L&D department has achieved a long and growing list of both local and national awards and accolades. This year, U.S. News & World Report ranked the L&D unit at Renown Regional as "High Performing in Maternity Care – Uncomplicated Pregnancy.” This award is only the latest in this department’s “Best Of” accolades list, as the unit also achieved a win as the Best Place to Have a Baby in the 2022 Best of Reno Awards. Not only is the department continually recognized, but individual team members also receive coveted awards within their professional associations. As previously mentioned, Krystie Mortensen is a DAISY Award winner, which means that she has been recognized for the “super-human work” she has done throughout her career. Additionally, three team members, including Roya Galata, have received NOA awards, celebrating their contributions to the nursing profession as a whole. Many nurses in this department also choose to pursue lifelong learning by taking advantage of the educational benefits that Renown offers. Several team members have completed their continuing education in midwifery and advanced practice, reaffirming their dedication to delivering healthy babies and helping parents manage their first few days with their newborns. “The teamwork on this unit is phenomenal, and the energy and commitment that the staff comes in with every single day amazes me,” said Lora Carlson, Renown L&D Manager of Nursing. Internally, the L&D department loves to show their spirit at Renown. In December, they received the Best Holiday Decoration award during the 2021 holiday season. The team also enjoys participating (and scoring well) in Renown-sponsored Halloween costume contests. In 2023, the L&D department will only pursue greater heights to continue producing patient outcomes. A Work Family “I stay here because this is my family. My work family.” These strong words were proudly stated by Jeanne Bufkin, Renown L&D Surgical Technician, and echoed by virtually every L&D employee. Having each other’s backs during both times of need and times of celebration is a must in this department, and they do so proudly. “Our staff constantly back each other up,” added Lora Carlson. “They display a lot of adaptability and flexibility. That’s why our unit functions as well as it does.” Several team members in this department experienced the care of the L&D unit at Renown before they became fully-fledged employees. “I had two of my babies here and had wonderful experiences both times,” said Judy McBride, Unit Clerk. “I love being a part of the reason why the next woman can say the same!” Bri Goode also delivered her child at Renown and loved her experience so much that she was also inspired to join the team. “I chose to work at Renown because when I had such a positive experience during my delivery while I was in nursing school, I knew it was a team I wanted to be a part of.” Coming to Renown was clearly an easy decision for this team; staying at Renown is even easier. “I stay here because I love what I do and who I do it with,” said Judy McBride. “I truly feel like I am treated as an asset to this department, and it makes me want to come to work every day and make a difference in these mothers’ lives.” The closeness of this department and the top-of-the-line collaboration displayed by every provider can be felt by the patients during their entire stay at Renown. “We have an amazing collaborative team of physicians, nurses, scrub techs, unit clerks, patient access representatives and environmental services personnel that strive to provide our patients with the best possible care,” said April Tucker. The labor and delivery process is a team effort – and those interested in jumping in on this team effort are welcome to join. Delivering healthy babies and supporting new mothers are cornerstone acts in meeting Renown’s mission of making a genuine difference in the communities we serve. Our L&D department does precisely this and more, never giving up in Fighting the Good Fight.
-
Department Spotlight: Surgery & Procedure Scheduling
When it comes to intimidating procedures such as surgery, cardiac catheterization (Cath) or interventional radiology (IR), there can be a lot of unknowns. What can I expect on the big day? What will happen after I’m all done? Will I have to worry about my orders not being in the system? Who can I call if I have any last-minute questions? It’s easy for your thoughts to race as you approach your procedure date, but luckily, there is a team who puts your mind at ease. With Renown Health’s Surgery & Procedure Scheduling department, patients can breathe a sigh of relief knowing that all the nitty-gritty is taken care of before they step foot in the procedure room. This team operates in the mindset of a complex Tetris board – fitting in all the pieces to make sure every patient is set on the path for surgery success. Consistent Contact Our Surgery & Procedure Scheduling team has a unique history. Initially operating as two separate teams, over the last year, our leaders skillfully combined the two teams together under one umbrella. That allows the now singular team to have line of sight across every surgery and Cath or IR procedure plan and be better stewards of the resources they have at their fingertips to provide streamlined, more-connected care for patients. As one might imagine, with the merger of the two teams, the day-in-the-life of each team member is full of a variety of crucial checklist items to cross off – all supporting constant communication from patients to providers. On the surgery scheduling front, these team members are resource rockstars. From working with referring providers to get patients scheduled appropriately to ensuring rooms and equipment are available for every patient, this team makes sure everything and everyone is in place when the time comes to help create a successful procedure and the best possible patient experience. “In surgery scheduling, we handle inbound calls for the outside offices to get time scheduled for each patient in the operating room (OR),” said Lydia Sharkey, Senior Scheduler. “We make sure there are plenty of anesthesia resources and equipment for every surgery, including any important information that we need to schedule patients appropriately and adding all documents to the OR board. If we need to swap rooms or move patients around, we handle that process too.” Over on the IR/Cath scheduling side of things, this team is on the frontlines of patient communication. They are experts in helping patients navigate their procedure from start (seeing their provider and obtaining the proper referrals) to finish (the day of the procedure and post-procedure process). “My day is a little different than the hospital schedulers; our part of the team handles the outpatient aspect,” said Adrienne White, Senior Scheduler. “We are in constant contact with patients and the IR and Cath departments. We help them navigate their procedure, including what to expect during and after the procedure. We get them through the process as easily as possible and ease their minds, so they know what is going to happen every step of the way. It’s all about communication, communication, communication!” This department has a significant overarching role: make sure all documents and ancillary information is set up for all our clinical teams that help with surgeries and procedures. This critical work means that every process is followed, and no important details are left out. “No one wakes up and says, ‘I want to have surgery;” our team goes above and beyond to make sure every single detail is taken care of so that when patients arrive, everything is in place,” said Trisha White. “Our team works hard to ensure everything runs as efficiently as possible because we want to use our resources in the best way possible to serve our patients without delays. We make sure we receive all the orders, codes and insurance and that the teams that follow after us – including our pre-admit team and nurses – have all the information they need to do their job seamlessly." With all the work they accomplish daily – not to mention how they wholeheartedly support each other through it all – it’s no question that the entire team has a lot to be proud of. Besides helping make patient care possible, the team puts their departmental merger and the move to fully remote work at the top of the list. “We’re most proud of merging the surgery scheduling and procedure scheduling teams together and therefore more cohesive,” said Mary Gray, Senior Scheduler. “The merger has made our team blossom and be able to connect with and rely on one another even more. We aren’t afraid to speak up and say something. At the end of the day, we’re here to take care of the patient, but we also help each other out. Our morale has gone up, and everybody is happier. Even though we all work remotely, we are more connected and have a great work-life balance.” “Along with transitioning the two teams into one big team, the move to being fully remote was huge," added Patricia Cruz-Hernandez, Surgical RN Scheduling Coordinator. “We worked through all the glitches, and it was a seamless transition to move into a remote setting. What’s great is that it did not affect patients at all; everything still gets done exactly as it should.” No matter how busy the days may get, Renown’s surgery and procedure schedulers always remember one thing: they are incredibly grateful for their fellow team members. “We have a very efficient and hard-working team of women,” said Pam Chapa Valencia, Senior Scheduler. “I could not have handpicked better people for our team,” added Trisha White. “I feel so lucky to have the team that we have.” A Renown “Why” Our Surgery and Procedure Scheduling team members all have diverse stories to tell about their road to Renown and why they’ve stayed in the department for as long as they have. Whether they’ve been with us for two years or two decades, they all share the same strong calling to care for their community. “I always wanted to help people, and my grandma was a nurse,” said Pam Chapa Valencia, Senior Scheduler. “I loved hearing her stories, and it made me want to be involved in patient care.” “I have a caring nature, and a hospital nature seemed like the right fit – I've been here for 25 years,” added Mary Gray. Several of our schedulers recognized the influence Renown has within our community and the ability to grow professionally and personally, both of which were a driving factor in their decision to make our health system their long-term career. “I’m originally from southern California, and I moved here about eight years ago; my husband always talked so positively about Renown, especially with how big it is and how it has the only level II trauma center in northern Nevada, so my goal was always to get a job here,” said Lydia Sharkey. “It’s been a great environment to be a part of.” “I’ve been with Renown for 17 years, and I chose to come here because of the reputation of the services Renown provided and care they gave,” added Trisha White. “I also knew what opportunities there were for me professionally, and in doing so, we are taking care of our community. I’ve had the chance to grow within my own professional skills and leadership skillset.” A profound feeling of ‘home’ is a common theme among this department. These team members appreciate the sense of community Renown has, the strides we’ve made in expanding our reach and how our health system gives healthcare professionals who are new to the field a chance to succeed. “At the time, Renown was the only hospital that would train nurses, and as a brand-new nurse, I had no experience – Renown took a chance on me,” said Patricia Cruz-Hernandez. “I feel like this is home. Our health system is so community-based and people-first minded, keeping ‘mission over margin.’ We’re growing, we’re expanding, we’re everywhere!” “I was a part of a transition as the cardiology private practice I worked with became a Renown practice, and it was great,” added Adrienne White. “This transition enabled us to provide more services and better care to patients. I stay here because I see the leaps and bounds we’ve been able to make in terms of procedures, accessibility and patient experience.” As true advocates for both patients and each other, the team is proud to have found their niche – and the ultimate beneficiaries? Everyone undergoing a surgery or procedure at Renown. A Culture of Kindness and Gratitude When you meet the Surgery & Procedure Scheduling team, you are greeted with warm smiles and an enthusiastic “Nice to meet you!” You can’t help but smile back and feel the infectious kindness they exude. Renown operates with a People-First mindset, a vision that this department especially takes to heart. They emulate the exact definition of our “Collaboration” cultural commitment. “We’ve built very good relationships and rapport with the OR managers and board runners,” said Lydia Sharkey. “The communication that we have at all three locations is very solid.” “The OR leadership is always so willing to help out whenever they can, and the resources they’ve provided have been huge for us,” added Adrienne White. “All the teams that see the patients after us – especially the surgical pre-admit team and the case managers, are fantastic about collaborating with us and reaching out to solve any issues they may have,” added Trisha White. “We all work so well together, especially since we all impact patient care.” In any organization, strong and compassionate leadership is key to a thriving team. Luckily for our surgery and procedure schedulers, they have Trisha White on their side. They attribute a lot of their success to having a supportive leader who “gets it.” “Trisha has been a scheduler like us, so she completely understands when we’re having an issue, because she’s struggled with the same thing and knows where we are coming from,” said Mary Gray. “It makes us feel like we are not alone – I can always reach out to her, or any of my other coworkers, to ask questions and figure out a solution together.” Despite being a remote-only team that meets in-person only one or two times a month, this group never misses an opportunity to reconnect both online and offline. They frequently shout out their Culture Ambassadors, schedulers Pam Chapa Valencia and Roxanne Abundis, for their team’s high morale. “Even though we all primarily work remotely, our in-person days are some of my favorite days of the month,” said Trisha White. “We feel so uplifted, we laugh and we have fun. We love being with each other. Pam and Roxanne are our Culture Ambassadors, and they both have been amazing at planning fun things for our teams. They go above and beyond to make our team feel cohesive and included.” “Pam and Roxanne have been leaders in creating a fun environment and supportive culture for us,” added Lydia Sharkey. “Whether it’s creating care packages or making sure we all have a good time when we see each other in person, they deserve a lot of credit.” As this team excels in their roles and foster a culture rooted in kindness and gratitude, we can trust that Renown’s surgeries and procedures will continue to thrive, and patients will continue to benefit from their diligent efforts and commitment to efficiency. “We make the magic happen!” closes Mary Gray.
Read More About Department Spotlight: Surgery & Procedure Scheduling
-
CEO Blog: Improving Health Through Genetics and Big Data
Renown Health President and CEO Tony Slonim, MD, DrPH, discusses efforts nationwide to develop a more effective and efficient way to deliver care. explains the benefits of Renown Health’s population health study with the Desert Research Institute and 23andMe.
Read More About CEO Blog: Improving Health Through Genetics and Big Data
-
Research Shows Genetic Approaches to Breast Cancer Screenings Yield More Accurate Results
Clinical researchers with the Healthy Nevada Project co-author research paper with findings that emphasize the need for a comprehensive approach to breast cancer risk assessment – including a focus on genetic medicine – to help ensure that individuals at high risk are identified and supported proactively rather than reactively. Breast cancer is a leading cause of cancer death among women in the United States. According to the American Cancer Society, about 1 in 8 women will develop breast cancer and about 1 in 39 women will die from breast cancer. Breast cancer is associated with increased age, hereditary factors, obesity, and alcohol use. Since 1990, breast cancer death rates have declined progressively due to advancements in treatment and detection. In Nevada there are an estimated 2,310 new breast cancer cases a year, and genetic mutations such as in the genes BRCA1 or BRCA2 remain a top risk factor for this prevalent disease. Recognizing the urgency for progress in breast cancer research, a collaborative effort between physicians, advanced practice providers and scientists from the Healthy Nevada Project® (HNP) and Helix have unveiled groundbreaking research. This study explores how genetic screenings are a necessary supplement to traditional testing methods, together offering more accurate insights into a patient's likelihood of developing breast cancer in the future. HNP is operated by Renown Genomic Medicine and the Institute for Health Innovation and is one of the largest community-based population health studies in the country. Their team works in collaboration with Helix, a leader in precision health that delivers comprehensive genomic solutions. Together, this dynamic partnership aims to understand breast cancer risk factors and pave the way for more effective preventative measures. The combined research team studied 25,591 female HNP participants to evaluate the performance of different genetic screening approaches to identify women at high risk of breast cancer. The results of this research suggest that a combined monogenic, or single-gene, and polygenic, or multi-gene, approach to breast cancer screenings helped produce more accurate results and more closely identify study participants who have a high genetic risk of developing the disease. "Based on this research, we are advocating a shift in approach which would improve breast cancer risk assessment through a combination of effective family history ascertainment and genetic screening,” said Joseph Grzymski, PhD, principal investigator of the Healthy Nevada Project, research professor at the University of Nevada, Reno School of Medicine and co-author of the breast cancer research paper. “This tailored approach, founded on the assessment of individual genetic risk, not only intends to elevate patient well-being but also will improve efficiency and equity in healthcare." Complementing the team’s research on leveraging genetics to identify women at low genetic risk of breast cancer that could safely defer mammogram screenings by five to 10 years that was released in late 2023 in JAMA Oncology, the study suggests that incorporating genetic information can assist in personalizing breast cancer screenings and optimizing the use of screening resources. "Existing disparities persist across various facets of breast cancer screening and treatment; however, genetic screening is clearly a powerful tool to help facilitate early intervention for those at higher risk,” said Jamie Schnell Blitstein, APRN, a primary care nurse practitioner at Renown Health and co-author of the breast cancer research paper. “By placing a heightened focus on risk, we underscore the pivotal role of preventative breast cancer screening.” Despite the availability of effective methods for early screening, co-authors of this research found that 78 percent of women with a family history of breast cancer had their risk ascertained only after a breast cancer diagnosis. The findings emphasize the need for a comprehensive approach to breast cancer risk assessment – including a focus on genetic medicine – to help ensure that individuals at high risk are identified and supported proactively rather than reactively. “These findings that can profoundly impact how healthcare is delivered were only made possible by all the participants who were willing to consent to research,” said Alex Bolze, PhD from Helix and co-author of the publication. “Broad-scale collaboration projects like these between Renown Health and UNR that engage large populations where participants share both their genetic information as well as electronic health records drive advancements in preventative medicine, as well as fundamental biological research.” The research paper was officially accepted on Jan. 29, 2024, and will be published by Elsevier, Inc. on behalf of the American College of Medical Genetics and Genomics. The contents of the paper will appear in the international journal Genetics in Medicine Open. Read the full article by visiting sciencedirect.com. The Healthy Nevada Project is currently recruiting new study participants. Free to all Nevadans with a saliva sample or blood draw, participants and their referring providers receive access to whole-exome sequencing and clinical grade results that help provide insight into their unique genetic risks tied to heart disease and certain cancers. If you are interested in enrolling in the study, schedule a Virtual Consent Appointment through MyChart or contact the Renown Institute for Health Innovation at RenownIHI@renown.org or (775) 982-6914 to be connected to a Genomic Representative. About Renown Health Renown Health is the region’s largest, not-for-profit integrated healthcare network serving Nevada, Lake Tahoe and northeast California. With a diverse workforce of more than 7,000 employees, Renown has fostered a longstanding culture of excellence, determination and innovation. The organization comprises a trauma center, two acute care hospitals, a children’s hospital, a rehabilitation hospital, a medical group and urgent care network, and the region’s largest, locally owned not-for-profit insurance company, Hometown Health. Renown is currently enrolling participants in the largest community-based genetic population health study, the Healthy Nevada Project®. To join the Renown Health team, visit renown.org/careers. About Helix Helix is the leading population genomics and viral surveillance company operating at the intersection of clinical care, research, and data analytics. Helix enables health systems, life sciences companies, payers, and government partners to accelerate the integration of genomic data into patient care and public health decision-making. Learn more at helix.com.


.png?rev=5ac90884d83d45468d7e3a5389920ff1)