Search
-
How to Protect Your Kids from Heatstroke
Summer is around the corner, bringing heightened risks of heatstroke, especially for children who cannot regulate their body temperature as efficiently as adults. Infants are particularly vulnerable and may not express discomfort, so never leave a child unattended in a vehicle. Top Tips for Preventing Heatstroke Reduce the number of deaths from heatstroke by remembering to ACT. Avoid heatstroke-related injury and death by never leaving a child alone in a car, not even for a minute. And make sure to keep your car locked when you’re not inside so kids don’t get in on their own. Create reminders. Keep a stuffed animal or other memento in your child’s car seat when it’s empty, and move it to the front seat as a visual reminder when your child is in the back seat. Or place and secure your phone, briefcase or purse in the backseat when traveling with your child. Take action. If you see a child alone in a car, call 911. Emergency personnel want you to call. They are trained to respond to these situations Keeping Your Baby Cool in the Back Seat In hot weather, it is crucial to keep your baby cool and hydrated by using a car seat cover or towel over them to reflect the sun's rays. Dress your baby in lightweight clothing that covers their arms and legs. Keep an eye on your baby's skin color. Move them to a cooler place if they look too red or flushed. Keep the temperature at a comfortable temperature for you, not for your child. Keep the windows cracked open for ventilation and ensure nothing is blocking the airflow from entering or exiting the vehicle. Dress your infant appropriately for their environment, including appropriate head and neck coverings, to keep them cool and protected from sunburns. Ensure you have enough fluids to last an hour before getting out of the car or use bottled water if possible. Never leave your child unattended in a car. Steps to Follow if You Suspect Heatstroke Call 911 immediately. Cool the victim – Get the person to a shady area, remove restrictive clothing and cover skin with sheets soaked in ice-water, and place ice packs in the arm pits and groin. Have the victim drink cool fluids, preferably an electrolyte-containing sports drink. Monitor body temperature with a thermometer but stop cooling efforts after temperature has dropped to 102 Fahrenheit. Baby Safe Classes These classes help prepare parents for emergencies that may occur in baby’s first year. Safe Kids Worldwide Did you know heatstroke is the leading cause of non-crash related fatalities in children? “On average, every 10 days a child dies from heatstroke in a vehicle. In more than half of these deaths, the caregiver forgot the child was in the car.”
-
When Care Can’t Wait: True Stories of Renown ER
Renown Health is home to three 24/7 Emergency Rooms (ERs) providing comprehensive emergency and trauma care, access to specialists and inpatient services backed by the area's most extensive health system. In 2023, Renown Health cared for 132,340 patients across three ER locations. Renown is also home to the region’s only level II trauma centers for both adult and pediatric patients. We spoke to three patients who sought immediate medical attention for various ailments and conditions to learn more about their emergency care experience and why they chose Renown ERs. Kamrin’s Story: From Worrisome to Critical In the spring of 2021, Danielle and her 13-year-old son Kamrin visited his primary care doctor for unexplained vomiting and were promptly referred to Renown Children's ER via ambulance for further evaluation and seen by board-certified emergency physician, Dr. Lisa Nelson. What initially began as an unassuming doctor's visit quickly turned into something much more severe after several tests confirmed a devastating abdominal tumor and a stage-four cancer diagnosis, unbeknownst to the family. Kamrin was immediately admitted to the Pediatric Intensive Care Unit (PICU) and referred to a Pediatric Oncologist at Renown Children’s Hospital to begin his plan of care with expert pediatric hematology and oncology specialists. Regarding the board-certified physician, who delivered the results to the family, Danielle said, “She was so calming to us, even as the diagnosis haunted us. She led us by guiding our family through the unknowns. She felt like a family member to us in that moment, letting all the unknowns be well known.” “The love, empathy, support and guidance these employees gave us carried us. The care team quickly and easily became a source of relief, knowing we were their priority and in the best hands. We are forever grateful for the team at Renown Children's Hospital and Renown Children’s ER; they truly saved our son's life and continue to be our guiding light whenever it's needed in our son’s health journey,” Danielle said. Today, Kamrin is in remission and navigating the aftereffects of chemotherapy, including an immune system deficiency. However, his family chooses to navigate each day by embracing the positive side of things, such as the life-saving impact of his treatment. Did you know? Renown Children's Pediatric Hematology and Oncology is located within Renown Regional Medical Center and offers expert pediatric specialists dedicated to providing comprehensive treatment for pediatric hematology and oncology, including chemotherapy, radiation therapy and infusion services. Taylor’s Story: From Crisis to Recovery Promptly after cosmetic surgery performed by a medical professional not associated with Renown, Taylor Salas (Chacon) began to lose consciousness and notice her post-surgery drainage systems, also known as Jackson-Pratt drains, fill with blood. She was transported to Renown Regional ER via ambulance and immediately seen by ER staff and board-certified emergency physician Thea Berning, MD, for medical assessment. Taylor drifted in and out of consciousness as the ER team began blood transfusions and a CT scan to determine her plan of care. Dr. Berning began facilitating communication with a community plastic surgeon with privileges at Renown Health and emergency surgery was performed to stop Taylor’s internal bleeding. Taylor was placed on a ventilator due to respiratory distress and trauma from the event, then transferred to Renown’s Intensive Care Unit (ICU) to continue her care. Thankfully, Taylor listened to her gut when something didn’t feel right after her surgery and sought immediate medical attention. The ER team's quick response, communication and collaboration with a plastic surgeon saved Taylor from severe internal bleeding. “I was informed every step of the way about what was happening and why. I felt comfort in this,” she said. Did you know? Because of Renown Regional Medical Center’s Level II Trauma Center distinction, you have immediate access to an extensive list of specialists and physicians trained in a wide array of specialties, in the event of a traumatic injury or accident. This is one of the many benefits of Renown Regional’s Level II Trauma status. Ted’s Story: The Unsuspected Threat Bothered by symptoms of heartburn, fatigue, neck pressure and arm discomfort, Ted was in the middle of a busy workweek in June 2023 when he began to suspect something was wrong. Knowing the importance of addressing early heart attack symptoms immediately, Ted and his wife headed to Renown Regional ER because of proximity and some familiarity with Renown’s leading cardiology care and technological expertise. After prompt assessment by the Renown ER team, including blood work, imaging tests and the administration of medication, Ted was admitted to the hospital to treat the blockage and narrowing of his coronary artery. On June 8, Ted was admitted for treatment, where he successfully underwent a single bypass surgery and recovered in the Cardiac Intensive Care Unit (CICU), before being discharged and following up with the Intensive Cardiac Rehab (ICR) program at Renown. The ICR program at Renown played a pivotal role in Ted's 55-pound weight loss and overall health improvement, empowering him to embrace a healthier lifestyle and find ways to use his newfound energy and strength today. “Overall, I believe I had the best care possible because of the collective group of people at Renown caring for this community, who we could see in the grocery store, at the ball game and in the shopping malls. This community feeling is something you might not get in a big city hospital,” Ted said. Did you know? Intensive Cardiac Rehab at Renown Health is a medically supervised program designed to improve cardiovascular health after a significant heart condition or procedure. Since its inception in 2016, this program has been a pioneer in the region for cardiac rehabilitation focusing on three key pillars including exercise, nutrition and stress management.
Read More About When Care Can’t Wait: True Stories of Renown ER
-
Preventing Skin Cancer A Doctors Tips
Want to protect yourself from skin damage from the sun’s harmful rays? Dr. Angela Walker, dermatologist with Renown Medical Group, shares what you can do to prevent skin cancer. What can people do to prevent skin cancer while enjoying the outdoors? There are several steps you can take to protect your skin from the sun. “I caution all of my patients to avoid the sun during the hours of 10 a.m. until 2 p.m. when UV rays are strongest. I also encourage people to wear sleeves on cooler days. And don’t forget that we still need to wear sunscreen on cloudy days! UV rays can still cause sun damage on cloudy days. Preventing skin cancer also entails wearing sunscreen of at least SPF 30 everyday. Are hats also a good idea for skin protection? Yes, of course! Choose a wide-brim hat that shades the face as well as the back of the neck for extra protection against UV rays. When it comes to identifying skin cancer, what should people watch for? We use easy-to-remember letters when checking for spots on the skin; it’s called the ABCDEs: A - Asymmetry: One half of the mole or lesion doesn't match the other half. B - Border irregularity: The edges of the mole are irregular, blurred, or notched. C - Color variation: The mole has different shades of color or uneven color distribution. D - Diameter: The diameter of the mole is larger than the size of a pencil eraser (about 6 millimeters) or is increasing in size. E - Evolution: Any changes in the mole over time, such as size, shape, color, itching, bleeding, or crusting. These guidelines can help in identifying potentially suspicious skin lesions, but it's important to consult a dermatologist for proper evaluation and diagnosis. Early detection is crucial for successful treatment of skin cancer.
-
The Expanded Role of OBGYNs in Women's Healthcare
Obstetrician-gynecologists (OBGYNs) see patients from menses (the monthly menstrual cycle that occurs as a part of the female reproductive system), pregnancy and childbirth through menopause and play a pivotal role in managing reproductive health and overall wellness. Dr. James Alexander with Renown Women's Health explains. "As experts in women's health, we are uniquely positioned to recognize subtle changes or symptoms that might indicate broader health issues. This comprehensive approach allows us to serve as a valuable first touchpoint for various health concerns." Preventive Screenings: A Proactive Approach One key aspect is an OBGYN's ability to recommend preventive screenings based on your symptoms, age, lifestyle and medical history. For instance, lipid screenings are critical for monitoring cholesterol levels, which can be a significant factor in women’s heart disease. An OBGYN keeps up with the current guidelines for routine screening as well as in women with risk factors such as high blood pressure, diabetes, or a family history of heart disease during your visit. By identifying risks and abnormal screening early, they can collaborate with you to implement lifestyle changes or treatments to reduce your risk of heart conditions. Schedule Your Screening Appointment Make an Appointment by Phone: 775-982-5000
Read More About The Expanded Role of OBGYNs in Women's Healthcare
-
Celebrating Resilience: Raquel's Remarkable Journey Through Breast Cancer Treatment
Raquel was 33 when she was diagnosed with breast cancer. It was April 2023, when she found a lump in her breast and was referred to the William N. Pennington Cancer Institute. After comprehensive imaging, she was diagnosed with invasive lobular carcinoma, which is a type of breast cancer that begins in the milk-producing glands of the breast. Between June 2023 and January 2024, she received a total mastectomy, chemotherapy and radiation at Renown Health. “Breast cancer is uncommon in women under 40, but any woman with a mass or lump in her breast should have an exam by a physician and imaging at any age,” said Dr. Lee Schwartzberg. In fact, according to the Centers for Disease Control and Prevention (CDC), only 9% of all new cases of breast cancer in the U.S. are found in women younger than 45. “It was a pretty scary diagnosis, but I’ve been led by great people through the process,” she said. “They were so helpful and there for me throughout the chemo and radiation.” Raquel's journey through breast cancer treatment at the William N. Pennington Cancer Institute was marked by the exceptional care provided by the Renown Health team, including nurses, nurse navigators, therapists, support teams and providers. Among the dedicated professionals, Dr. Michelle Chu and Dr. Lee Schwartzberg played pivotal roles in Raquel's diagnosis and subsequent treatment plan. Their expertise, compassion and commitment to patient care left an indelible impact on Raquel's experience. Their thorough examination and comprehensive approach ensured that Racquel received the best possible care for her invasive lobular carcinoma. In addition to the care provided at Renown, Raquel greatly benefitted from being connected with a mentor by Dr. Chu. This mentor, Kayla, had undergone a similar diagnosis and treatment plan, and at the same age Raquel. They texted and called each other throughout Raquel’s treatment, providing additional support through a challenging time. As of January 2024, Raquel is done with her treatment and continues to see her care team for follow-up appointments. “I’m through the worst and ready to rebuild my life,” Raquel said. To help celebrate this milestone, Nevada Athletics invited Raquel to receive the game ball at a Nevada Men’s Basketball game. She was joined on the basketball court for this special recognition by her husband, Raul; mother, Arlene; and two daughters, Ryleigh and Rhiannon. Racquel's journey is not only a testament to her resilience but also a tribute to the invaluable contributions of Dr. Chu and Dr. Schwartzberg in guiding her towards triumph over breast cancer.
Read More About Celebrating Resilience: Raquel's Remarkable Journey Through Breast Cancer Treatment
-
A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
Embarking on the path to bariatric surgery is a unique and deeply personal journey. Individuals like Mary Escobar choose this life-changing route for reasons ranging from improved cardiovascular health to managing diabetes or finding relief from various health complications. In Mary's case, her two-decade-long healthcare journey not only underscores the challenges she faced but also highlights the support and expertise that ultimately led to her successful transformation through bariatric surgery. Mary's Resilience: December 2002 through February 2003 More than two decades ago, Mary experienced unforeseen health complications just days after giving birth via c-section. Septic shock, hemolytic uremic syndrome, thrombocytopenia, renal failure and a blood clot in her lung plunged her into a critical state. Intensive care, plasma exchange and a long recovery followed. After being discharged with compromised kidney function, Mary faced complete renal failure two years later, leading to dialysis and a spot on the donor list. Mary's brother, a perfect match, selflessly donated his kidney on Dec. 14, 2007, marking a turning point in Mary's health. However, the post-transplant period brought new challenges, including diabetes, high blood pressure and a significant weight gain, reaching 230 pounds. Determined to regain control, Mary explored various diets without success until she consulted with a bariatric doctor. Journey to Bariatric Surgery: November 2009 - April 2021 In November 2009, Mary opted for a gastric band, shedding 40 pounds within a year. Despite initial success, issues with the gastric band arose, prompting a consultation with Dr. John Ganser at Renown Health in April 2021. Together, they decided to transition to a gastric sleeve, with comprehensive education provided to ensure long-term success.
Read More About A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
-
Understanding the Reasons Behind Heavy Menstrual Cycles
While menstrual cycles can be an annoying inconvenience for many women, heavy bleeding (menorrhagia) is not normal and can disrupt your life. A few days of heavy flow at the start of your period is usually nothing to worry about. However, if you’re frequently experiencing very heavy periods, you should discuss it with your gynecologist or primary care provider. Dr. Megan Fish, an OB-GYN with Renown Women’s Health, discusses various reasons, evaluation and treatment methods when it comes to heavy menstrual cycles. What is classified as heavy menstrual bleeding? The American College of Obstetricians and Gynecologists considers heavy bleeding to be any of the following signs: Bleeding that lasts more than 7 days. Bleeding that soaks through one or more tampons or pads every hour for several hours in a row. Needing to wear more than one pad at a time to control menstrual flow. Needing to change pads or tampons during the night. Menstrual flow with blood clots that are as big as a quarter or larger. What are the most common reasons for heavier periods? A variety of reasons why someone might have heavy periods. Fortunately, most of these problems are treatable. Because each woman's period is unique, only a doctor can definitively determine the cause of your heavy periods. Some of the most common issues that cause heavy periods include: Hormone imbalances such as anovulation, thyroid disease and Polycystic Ovary Syndrome (PCOS). Structural abnormalities in your uterus such as polyps or fibroids. Precancer and cancer such as uterine, cervical, vaginal, ovarian or endometrial hyperplasia. Infections such as chlamydia, gonorrhea, endometritis or vaginitis. Other medical conditions such as liver disease, kidney disease or Pelvic Inflammatory Disease. Medications such as blood thinners and aspirin, hormone replacement therapy, Intrauterine devices (IUDs), birth control pills and injectables. Pregnancy-related problems such as a miscarriage or ectopic pregnancy.
Read More About Understanding the Reasons Behind Heavy Menstrual Cycles
-
6 Healthcare Action Items for the LGBTQIA+ Community
© Niyazz via Canva.com Every patient, regardless of how they may identify, greatly benefits from preventive healthcare and early detection. Members of the LGBTQIA+ community face unique considerations when it comes to their health, and a proactive approach to preventive screenings and vaccines is important in order to address their individual health needs. Dr. Karen Thiele, Family Medicine Physician with University Health and Assistant Professor of Family and Community Medicine at the University of Nevada, Reno School of Medicine, breaks down key steps that LGBTQIA+ patients should take to safeguard their health. PrEP and PEP Pre-exposure prophylaxis (PrEP) is a strategy to prevent human immunodeficiency virus (HIV) infection. It is an important measure for those who are HIV-negative but may be at risk of contracting it. The highest risk sexual practice is receptive anal intercourse, due to the relative fragility of rectal tissue. This medication can stop HIV from spreading in the body and help patients maintain their HIV-negative status. PrEP is available in both pill form, which is taken every day, and injection form, of which the first two injections are initiated one month after another while all other injections are initiated every two months. Post-exposure prophylaxis (PEP) is an antiretroviral drug regimen taken after potential HIV exposure to prevent an HIV-negative individual from converting to HIV-positive status. PEP is only for emergency situations and must be started within 72 hours of exposure – sooner is always better than later – and must be taken for 28 days. PrEP and PEP are available in many ways, including visiting your primary care provider (PCP) or an urgent care location. HPV Immunization All genders and identities can protect themselves against human papillomavirus (HPV), a sexually transmitted infection (STI) that can lead to the risk of cervical, mouth, head, neck, throat, anal, vaginal, penile and vulvar cancers. HPV is so common that nearly all sexually active people, regardless of sexual orientation and practices, will be exposed at some point in their lifetime. The HPV vaccine (common brands include Gardasil and Cervarix) is a safe and effective method to prevent HPV, according to the Centers for Disease Control and Prevention (CDC). This vaccine protects against infections that can lead to HPV-related cancers and precancers, as well as genital warts. While patients should start receiving the vaccine at 9 years old years old, unvaccinated adults up to the age of 45 can also receive the vaccine through their PCP – better late than never! STI Testing Sexually-transmitted infections form from bacteria, viruses or parasites that can be transmitted by person-to-person sexual contact through semen, vaginal, blood and other bodily fluids. According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new STI cases across the nation each year. Luckily, most STIs are preventable. Annual STI testing for HIV, gonorrhea, chlamydia and syphilis is important to stay on top of your sexual health. Because these STIs may sometimes have no symptoms, screening is recommended regularly and with any change in sexual partners. Depending on the specific condition, tests for these infections include urine, swab and blood tests. Speak with your primary care provider on a screening schedule that works best for you. Prostate Exams Prostate exams look for early signs of prostate cancer in patients who still have a prostate. The CDC recommends those who are at least 55 years old get regular prostate screenings; however, for patients with a family history of prostate cancer, screenings may be recommended as early as 45 years old. These exams are done via two common methods – a prostate specific antigen (PSA) blood test and a digital rectal examination (DRE). Your provider can help you determine your risk and when you should start getting screened. Pap Tests and Pelvic Exams Patients of all genders who have a cervix, uterus, vagina and/or ovaries will benefit from regular pelvic exams and Pap screenings. A pelvic exam consists of a provider looking inside the vagina and at the cervix for anything unusual. A Pap test, also known as a Pap smear, involves your provider using a small, soft swab to collect cervical cells to check for early signs of cancer. Generally speaking, people with these organs should have a Pap test every three years starting at age 21 through the age of 30. After age 30, patients should receive a Pap test with HPV co-testing every five years until age 65. These recommendations are changing based on new research, so it is important to have a conversation with your PCP about the current guidelines so you can make an informed choice about what schedule you should follow. A gynecologist or your primary care provider can counsel you and perform these screenings. Mammograms and Breast Exams People with breast tissue, especially dense breast tissue, are at risk for breast cancer, and regular breast screenings are your best line of defense. At-home breast self-exams are the first step – you will want to check your breasts for any lumps, changes, fluid leaks, irregular tissue thickening or anything else that feels unusual. The Breast Cancer Risk Assessment tool, provided by the National Cancer Institute, is a good place to start to identify your risk. Talk with your primary care provider about the risks and benefits of starting screening at age 40 so you can make an informed decision about when to start. If you have any family history of breast or ovarian cancer, your PCP will offer you genetic testing for BRCA 1 and 2 mutations. Nevadans over the age of 18 can also get BRCA genetic test for free by enrolling in the Healthy Nevada Project. Mammograms are important screening tools, but for a significant portion of people with breast tissue, density of the breast tissue may make mammograms less helpful in detecting cancer. Your primary care provider can help you decide what additional imaging (such as breast ultrasound) might be best for you.
Read More About 6 Healthcare Action Items for the LGBTQIA+ Community
-
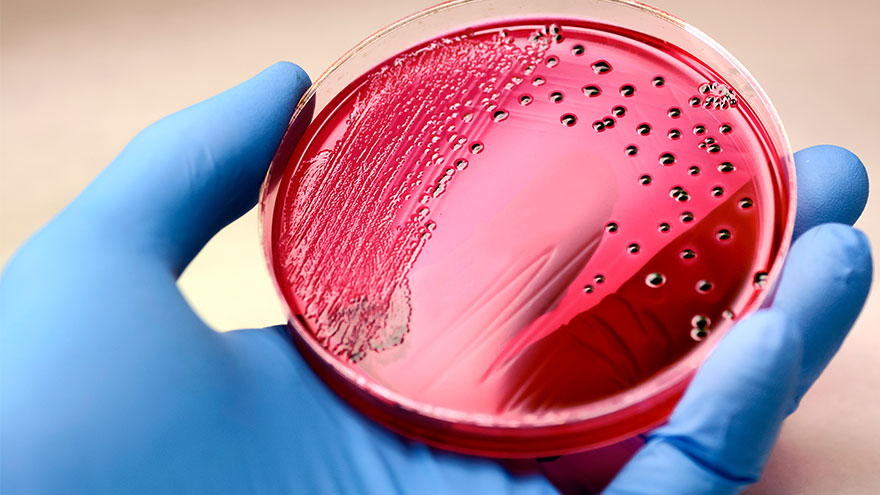
Sepsis: Causes & Symptoms
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.
-
Department Spotlight: Respiratory Care
This Department Spotlight is dedicated to Jason Simpson, Manager of Respiratory Services at Renown Children’s Hospital. Take a moment to breathe deeply. Inhale in, exhale out. We rely on our lungs to provide us with the air we need to live a healthy life – and this essential bodily function is something that many of us don’t think twice about since it comes easily for us. Now, imagine yourself as someone who is living with severe asthma, chronic obstructive pulmonary disease (COPD) or someone who was recently diagnosed with a frightening respiratory condition like COVID-19 or pneumonia. The simple act of breathing can prove to be an intimidating venture requiring the care of a professional. Who are the people that take on the challenge? Meet Renown Health’s Respiratory Care Services department. Serving patients across 13 service lines, three acute facilities, outpatient locations and telehealth, our respiratory specialists – including respiratory therapists, respiratory care aides, inpatient COPD respiratory therapy navigators and educators and more – use their expertise to help restore the vitality of all their patients with every inhale and exhale, shaping a healthier livelihood one lung at a time. The Guardians of Respiratory Wellness Whether they are managing lifelong respiratory conditions or offering crucial support in emergencies, the Respiratory Care team strives to enhance the quality of life for every patient. As an indispensable member of the clinical team at Renown, our respiratory therapists work collaboratively with doctors and nurses to tackle a wide range of tasks, tailoring care for each patient’s unique needs. “Respiratory care is involved with all stages of life, from beginning to end,” said Sarah Kurtz, Respiratory Therapist. “We work closely with nurses and doctors and perform arterial punctures, breathing treatments, weaning maneuvers for patients on life support, intubations and much more. We assess patients constantly to see if their care needs to be upgraded or if they can be weaned to get them back home with their families.” “You start your morning researching your assigned patients,” added Tim Start, Respiratory Specialist. “We go over lab values and chest radiographs and decide the best plan of care for each patient. Our objective is to improve their respiratory status by giving them medications and doing breathing exercises. We participate in other forms of care with nurses, such as activities of daily living (ADLs) and mobilization. We work as a team, and that enables us to provide great patient care.” For patients living with COPD, enjoying all that life has to offer comes with a separate set of obstacles. According to the Centers for Disease Control and Prevention (CDC), over 200,000 people across the Silver State are living with this chronic condition. Luckily for them, Renown has a specialized team to help these patients optimize their life and manage their condition with individualized treatment and education. “We run a report every morning to identify all the patients currently admitted who have a history of COPD, take respiratory medications or smoke,” said Amber Beck, Inpatient COPD RT Navigator. “After looking through their charts, we visit with the patient (and possibly their family) at the bedside to help them better understand how to manage their breathing issues.” As a vital part of the Respiratory Care team, Renown’s respiratory care aides help ensure the seamless operation of our respiratory care services. These dedicated professionals provide essential support to respiratory therapists not only during intricate procedures but also outside of face-to-face patient care by transporting equipment, restocking supplies, assisting in the mobilization of patients and more. “We are responsible for the maintenance of unit supplies and making decisions regarding levels of stock to be maintained,” said Dia Ramos, Respiratory Care Aide. “We also transport equipment, refill the oxygen tanks on the floors and intensive care units (ICUs), order and stock respiratory care supplies, mobilize patients and assist the respiratory therapists during bronchoscopies in the ICUs. In addition, we clean respiratory equipment like mechanical ventilators, continuous positive airway pressure (CPAP) and bilateral positive airway pressure (BiPAP) machines, high flows and aerosol poles.” Once the COVID-19 pandemic hit, a special spotlight shined upon respiratory care teams across the country for the heroic care they provided patients in respiratory distress. While their roles in health systems have gained a better understanding nationwide, this team understands it is vital for them to educate the community about the important jobs they hold for our patients. “Respiratory care can be under the radar,” said Pam Umek, Respiratory Specialist. “Once, when I told someone that I am a Respiratory Therapist, they said, ‘Oh, like a yoga breathing instructor?’ I then explained all the things we do: intubation, extubation, bronchoscopies, transports, traumas, codes, rapid responses, pediatrics/NICU, breathing medications/therapies, open heart rapid ventilator weaning … needless to say, that individual walked away with a better understanding of not just Respiratory Care Services but also the enormous effort it takes to care for our community.” The accolades and achievements continue to pour in, from national awards and certifications to implementing different jobs in care units to optimize the patient care experience. “We have earned and continue to maintain the Joint Commission Disease-Specific Certification for COPD,” said Amber Beck. “We are well below national averages for 30-day readmissions, lengths of stay and mortality due to COPD. Sandy, one of our COPD Coordinators, was a recipient of a patient advocacy award from the American Association of Respiratory Care and FACES Foundation.” “We have started implementing Respiratory Care Aides in the critical units, starting with the Cardiac ICU,” added Dia Ramos. “We work as one team and are always helping each other with their tasks.” Education and mentorship are at the core of Renown’s mission to make a genuine difference in the health and well-being of every patient. Nurturing the next generation of medical professionals – including respiratory care professionals – is a task that the Respiratory Care team takes seriously. “It has been great being able to help educate students in different disciplines,” added Pam Umek. “We have been able to offer shadow shifts to students in emergency medical services (EMS), nursing and medical school. These opportunities help students entering the medical field have a better understanding of the many ways we can help care for our respiratory patients.” From the moment of birth to the final stages of life, Renown is fortunate to have a Respiratory Care team that tirelessly ensures every breath counts, safeguarding their role as a trusted partner within our health system. A Tribute to Jason Simpson, Healthcare Hero
-
3 Unexpected Perks of Choosing a Hometown Health Plan
© AndreyPopov via Canva.com Becoming a Hometown Health plan member opens you up to the largest provider network in our region. As northern Nevada’s only not-for-profit health insurance company, the hometown advantage goes beyond your health coverage – and you may not be using all the perks available to you. Here are three benefits that Hometown Health is proud to offer all members to enhance wellbeing and connect the dots between healthcare and technology. MyChart MyChart is Renown Health's and Hometown Health’s secure online member portal that gives you direct access to your health and benefit information. From 24/7 access to your benefits and important documents to scheduling an appointment with your provider, this free tool is a great way to keep track of your family’s health. If you have a Renown primary care provider, you can use MyChart to: Securely email your healthcare provider. Get your test results faster and view your After Visit Summaries. Request prescription refills. Schedule and check-in for appointments. Pay your bill. Request your medical records and review immunization records. Manage designated health care agents and upload end-of-life documents, such as advance directives and a living will. View or download your documents: Member ID Card, Summary of Care, Explanation of Benefits, Referrals and Authorizations. Get in touch with our Customer Engagement Center. Telehealth Virtual visits have never been easier thanks to Renown Telehealth and Teladoc. These two tools are convenient options that allow members to be seen by a qualified doctor via phone or video chat who can diagnose, recommend treatment and prescribe medication for many non-emergent medical conditions – no matter where you are. Some of the health issues your virtual provider can treat include: Cold and flu Allergies Sore throat Sinus infection Respiratory infection Stomach bug Ear infection Urinary tract infection Both Renown Telehealth and Teladoc are also staffed with specialists in behavioral health, where you can speak with a therapist or psychiatrist on a wide variety of issues, including: Stress and anxiety Depression Trauma Grief Burnout Medication management Renown is also proud to offer access to top-level specialty care to address your ongoing condition and help guide you through illness maintenance and education. Through Renown Telehealth, Hometown Health members have access to a variety of specialties, including (but not limited to): Adolescent Medicine Cardiology Hematology, Oncology and Pediatric Oncology Nephrology Pediatric Endocrinology Pediatric Neurology Pulmonary and Pediatric Pulmonary Sleep Medicine New in recent years, Teladoc is now proud to offer both dermatology and nutrition visits. Teladoc dermatologists can treat conditions like acne, rosacea and rashes, while their registered dieticians can help you manage your nutrition and weight goals. Booking an appointment with Renown Telehealth is easy by heading over to MyChart and selecting “Schedule an Appointment.” To book an appointment with a Teladoc provider, visit teladoc.com or download the Teladoc app. Renown Telehealth is available within the state of Nevada, and Teladoc is available in all 50 states. Your copay can be as low as $0 for each visit; check your plan documents for more information. Doctoroo The house call has returned – avoid long urgent care waits with Doctoroo. Through Doctoroo, Hometown Health members have access to in-home urgent care services at the same price as your regular urgent care copay. A call to Doctoroo will dispatch a fully equipped medical team consisting of an EMT and either a nurse practitioner or physician assistant to your home within a few hours. Whether you need treatment or testing, each team is ready to provide care in the comfort of your own home with their over 60 medications and antibiotics, EKGs, wound dressings, IVs, catheters and more. Doctoroo care teams can address and treat many non-emergent care areas and conditions, including (but not limited to): Respiratory Ear, Nose, Throat Eye Wound Care Cardiac Care Musculoskeletal Gastroenterology Doctoroo is open year-round from 7 a.m. to midnight. Book a house call in minutes in the Doctoroo app or by calling (888) 888-9930.
Read More About 3 Unexpected Perks of Choosing a Hometown Health Plan
-
Importance of Safe Sleep
In today's fast-paced society, it is understandable for parents to want to take shortcuts in caring for their little ones. A s a result, It is tempting to leave a sleeping infant in a car seat or swing after a long day of errands or when you need a moment to catch your breath. But, as convenient as these devices may be, they pose a serious risk to your child's safety. Why Car Seats and Swings Pose Risks for Infant Sleep Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The American Academy of Pediatrics (AAP) states that “infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical.” If a parent must use a car seat or other sitting device, they should only do so for a short period of time and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The American Academy of Pediatrics (AAP) warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. This is because infants can easily slump over or become entangled in the straps, blocking their airway, and causing suffocation. Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The AAP states: Infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical. If a parent must use a car seat or other sitting device, they should only do so for a short period and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The AAP warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. In addition, infants can easily slump over or become entangled in the straps, blocking their airways and causing suffocation.