Search
-
Life after Lymphedema Diagnosis: What to Expect
Managing lymphedema effectively is essential for enhancing the quality of life for individuals affected by this condition. Katherine Bunker, a Physical Therapist and Certified Lymphedema Therapist (PT, DPT, CLT) at Renown, has expertise in this area and her insights offer valuable strategies for managing lymphedema. Lymphedema is a chronic condition characterized by swelling in one or more limbs due to a blockage in the lymphatic system. This condition can result from cancer treatments, surgery, infection, or can sometimes be congenital. While it can be challenging to live with lymphedema, understanding the condition and adopting specific lifestyle changes and strategies can significantly improve the quality of life. Understanding Lymphedema Educating yourself about lymphedema is crucial. Understanding the causes, symptoms, and potential complications can provide you with the tools to manage the condition proactively. Lymphedema can lead to discomfort, decreased mobility, and in severe cases, infections such as cellulitis. Therefore, recognizing the early signs and knowing when to seek medical advice is essential. Medical Management Consulting with healthcare professionals who specialize in lymphedema is critical. A physiotherapist or occupational therapist trained in lymphedema management can tailor a treatment plan for you that can include the following: Compression Therapy - Wearing prescribed compression garments can help move the lymph fluid and reduce swelling. It’s essential to get fitted by a professional and understand how to use these garments correctly. Manual Lymphatic Drainage (MLD) a gentle massage technique that encourages the movement of lymph fluid out of the affected limb. It’s typically performed by a trained therapist but ask about self-massage techniques you can do at home.
Read More About Life after Lymphedema Diagnosis: What to Expect
-
Department Spotlight: Special Procedures
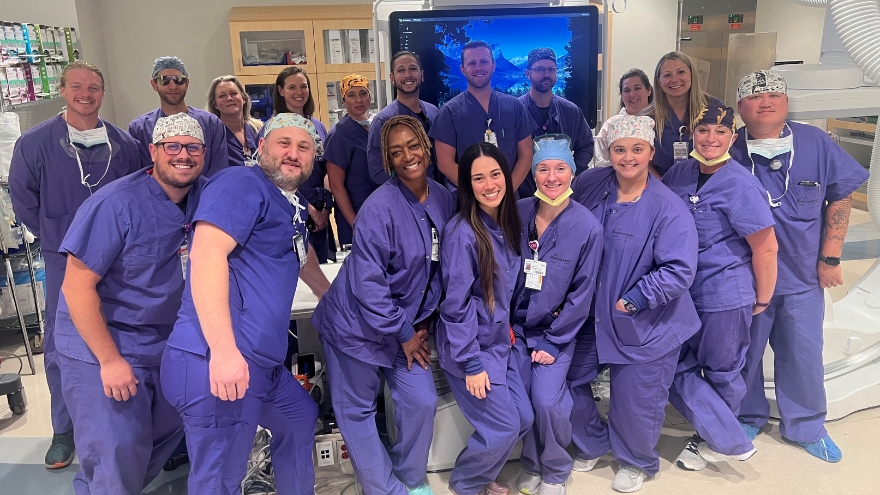
Chronic pain can be one of the most distressing feelings someone may encounter – and more likely than not, you know someone who is managing their pain as a part of their healthcare journey. In fact, according to the Centers for Disease Control and Prevention, about 1 in 5 U.S. adults have experienced chronic pain in recent years. One of the most common methods of treating pain is through prescription pain medications; however, with the rise of the opioid epidemic across the country, leveraging other interventions to help patients manage their chronic pain has become increasingly more important. What if there was a way to treat pain directly without the automatic need for pain medication? Luckily for patients in northern Nevada, our Special Procedures department at Renown Rehabilitation Hospital specializes in exactly that: interventional pain mitigation sans painkillers. With nearly 95% of their patients who come in with pain-related mobility issues being able to physically walk out of the hospital after their treatment, much-needed relief is clearly in store. Tight-knit and forever-caring, the Special Procedures team knows how to transform the purpose of pain management. A Penchant for Pain Alleviation Renown's Special Procedures team offers a wide variety of pain management solutions that are uniquely tailored to each individual patient’s needs. With the help of a team of 14 attentive nurses, interventional radiology technologists and a surgical technician – plus a dedicated patient access representative ensuring everything goes smoothly behind-the-scenes – these lifechanging interventions include: Epidurals (including steroid epidurals) Nerve blocks Ablations Tenotomies Spinal cord stimulator trials Peripheral nerve stimulator trials The nurses on this specialized team guide patients before, during and after their procedures, making sure they are at ease throughout the entire process. Each nurse emulates both expertise and empathy to help light the path towards healing. “Before each procedure, we get the patient’s vitals, health history and work with the doctor to answer any questions they may have about what is going to happen in the procedure room,” said Michon Edgington, RN. “After they’re all done, they come back to me, and I make sure they are ready to go home by educating them on their discharge. Our goal is to get them back to their families very quickly.” “In the actual procedure room, we perform safety checks, do charting, prepare the sterile tray for the doctor and give medication for conscious sedations, all while consistently monitoring the patient and helping the doctor out along the way to help the procedure go well,” added Shannon Boelow, RN. This team’s dedicated imaging professionals harness expertise that goes beyond capturing images. Their skillful utilization of X-ray technology serves as a guide for doctors administering treatments for pain – and according to our own physicians, our imaging technologists are some of the best in the business. “Our X-ray skills here are specialized,” said Julie Smith, Imaging Lead. “Visually, the doctor needs to see what’s going on inside the body so they can accurately place needles and steroids. We all work together collectively and work with each doctor to accommodate their preferences, helping the treatments go much faster and minimizing the patient’s exposure to radiation.” Serving as the ideal representation of both precision and support, the surgical technician on this team is an important collaborator in the procedure room, helping to ensure the success of every interventional procedure with a meticulous eye for detail. “As the Special Procedures surgical technician, I get the room ready with all the necessary instruments, including making sure everything is sterile,” said Carrie Crow, Surgical Technician. “I enjoy keeping the team organized.” Overseeing it all are the physicians, who are eternally grateful for the team for the life-changing interventions they offer every day. “Our physicians are so phenomenal,” said Brittney Summerfield, Manager of Nursing. “They are very supportive and collaborative, and they always do the right thing. They have total confidence in us.” Seeing patients walk out of the hospital happy and healthy is a driving motivator for this team. Whether they had significant experience in pain management or were ready for a completely new challenge, each team member comes to work every day inspired to move mountains. “I had worked in pain management in other facilities, and I was extremely excited to come here and solely focus on pain,” said Jodi Eldridge, Supervisor of Special Procedures. “I enjoy seeing the patients so happy when they leave no longer in pain. I feel immediate gratification, because you truly feel like you’re doing something big for the patient. It’s very rewarding.” “I decided to come work here because I worked in the inpatient setting for a long time, and I was ready to see a different side of healthcare and provide a different type of care to our community; plus, my coworkers are the best,” added Lisa Dunnivant, RN. There’s no question that the realm of pain management is a delicate one – and there is no team better suited to take on that challenge than Special Procedures, working harmoniously to bring relief and a renewed sense of livelihood for every patient they serve. “Some people believe pain management is just all about pills, and that is simply not true,” said Carrie Crow. “Our procedures are yet another way to help them manage their pain and find relief.”
-
Department Spotlight: Interventional Radiology
National Radiologic Technology Week is from Nov. 5-11, 2023. Join us in celebrating Renown's Interventional Radiology department!Try to put yourself in the shoes of someone who is told that they have a massive blood clot in their lung, someone who needs a biopsy to determine the next steps of their care, someone facing a stroke or brain aneurysm or someone who needs a catheter to receive treatment such as chemotherapy. You may immediately think that an intense and intimidating surgery is on the horizon. What if, instead of surgery, your care teams were able to use the necessary tools to treat your blockage or administer your medicine with an image-guided procedure? That’s precisely what the Interventional Radiology (IR) team at Renown Health does. Behind the doors of this department is where you’ll find a team of highly skilled individuals who operate like a well-oiled machine, ensuring that each procedure is executed with precision and care. Their commitment to excellence knows no bounds as they provide essential interventions to patients of all ages, from the tiniest newborns to the elderly. Their mission extends beyond diagnostic and therapeutic procedures; they are experts in understanding and serving the ever-evolving needs of their patients. Minimally Invasive, Maximally Impactful With their advanced expertise, our IR teams at both Renown Regional Medical Center and Renown South Meadows Medical Center harness the power of X-ray, CT and ultrasound technologies to navigate their way through life-saving minimally invasive procedures, such as thrombectomies, angioplasties, stent placements, embolizations, catheter and drain insertions and needle biopsies. In the world of medicine, Interventional Radiology often offers an alternative to traditional surgical methods, reducing the risk of hospitalization and helping patients embrace recovery more quickly. Our IR teams have a diverse and busy daily work life in order to make these complex and life-saving interventions happen – and they all have each other’s backs to ensure that every patient gets the care they deserve. “Every day is different, and no two days are alike,” said Ryan Nunes, Specialty Procedure IR Technologist at Renown Regional. “The day can start off first thing in the morning with several emergent cases, such as ruptured brain aneurysms to brain blockages. We all work really well together; we help each other out and come together to do things as a team.” Like every other team at Renown, patient well-being is always a number one priority. The IR department takes this commitment seriously, upholding the highest standards of ethics and safety. “We start the day by preparing rooms and making sure they are well-stocked, checking that all devices are working, performing safety checks and making sure the entire team is well-prepared for whatever cases come through the door,” said Aubrey Goldsmith, Supervisor of Clinical Nursing in IR at Renown Regional. “We have routine cases like drain placements, biopsies, line placements and more, and we also have life-threatening cases that come at a moment’s notice. Our nurses are responsible for monitoring patients throughout the procedure to make sure they are doing well the entire time and are there to respond if the patient has a decline.” "After completing the prior assessment of each patient, we look for any medical problems the patient may have before confirming it is safe for the patient to have procedure done,” said Brandon Hartwig, Interventional Radiology RN at Renown South Meadows. “We work closely with the physicians on all our cases while assessing each patient, going through labs and vitals and personalizing the procedure for each patient.” Even though the procedures they oversee are minimally invasive, the IR team understands that any procedure, regardless of the severity, can be incredibly frightening for any patient. Their best tool for handling patient anxieties? Communication. "The best thing we can do to reduce anxieties and fears in patients is to have communication with them to ensure they know what is going on and what to expect,” said Megan Rios, IR Technologist at Renown Regional. "We set clear expectations for the patients and give reassurance throughout the entire procedure.” "All of our team members are very attentive to our patients when it comes to potential fears and anxieties that they may have,” added Jazmynn Kimsey, IR Technologist at Renown Regional. “We always take the extra time to listen to our patients and break things down, explaining every step before, during and after the procedure.” Knowledge sharing is also a crucial part of the IR process. No patient will ever have to wonder, “what exactly is going on here?” “We provide each patient with education and advocacy throughout the process,” said Blaire Henderson, Interventional Radiology RN at Renown Regional. “We ensure every patient is as comfortable as possible at all times.” “When it comes to procedures, patients tend to be scared and nervous,” added Ryan Nunes. “The silver lining to what we do is that it is all done through very small openings of the skin, and we all explain this to patients. Most procedures we do are done under moderate sedation which helps put the patient more at ease.” In a world where advanced medical care meets the human touch, the IR team exemplifies Renown’s commitment to making a genuine difference in the health and well-being of everyone they serve.
Read More About Department Spotlight: Interventional Radiology
-
A Therapist's Tips to Prevent and Manage Osteoporosis
Want to know more about osteoporosis and osteopenia? We'll dive into these conditions and give you some handy tips on preventing future problems and taking care of your bones. What is Osteopenia? Osteopenia (low bone density) is the initial stage of bone mineral density loss, which can eventually progress to osteoporosis if steps are not taken to prevent it. What is Osteoporosis? Osteoporosis is a condition that weakens our bones. While it literally means “porous bone," it doesn’t mean that our bones are doomed to succumb to the changes that can happen to us silently over time. Our bones are living tissues that are constantly breaking down and remodeling themselves. Osteoporosis and osteopenia are typically diagnosed by testing bone mineral density using scans that your primary care provider can easily order. This is important testing because it dictates your risk of breaking a bone in common areas like your hip, wrist or spine. It also helps set the stage for talking with your healthcare team to develop a treatment plan. Most people will reach their peak bone mass in their mid to late twenties. There are several factors that increase our risk of osteoporosis or osteopenia as we age, such as menopause, genetics and other lifestyle factors. However, there are several things you can do to mitigate this breakdown and assist your body in the constant remodeling it does to our bones. 3 Controllable Factors to Build Strong Bones 1. Talk to your primary care provider They can go over a plan and prescribe things such as vitamin D, calcium and medications that can help if you are at risk or have osteoporosis or osteopenia. 2. Maintain a healthy diet Talk to a dietician if you need further help as they can be an invaluable resource to develop a plan. Eat foods rich in calcium, vitamin D and vitamin C. These assist with the rebuilding of bone. Examples include but aren’t limited to leafy greens, legumes, salmon and healthy dairy products. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per week. Alcohol interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. 3. Exercise Talk to your primary care provider to get a referral to physical therapy if you need help with exercise. Our bones adapt to the stresses we put them through. Therefore, exercise should be tailored to putting the right stress on our bones. There is good quality research that most exercise is safe when dealing with less bone mineral density. The exercises should be progressively challenging and increase the load for resistance and weight training at least two to three days a week. Examples include squats, step-ups, chest presses and rows. Exercises higher in velocity will lead to more power and bone adaptation. Examples include quicker push-ups, marching and quicker walks. Exercises that are weight-bearing will lead bones to adapt to the stress placed on them. Movements such as mini stomps, step-ups, jumping, jogging and so forth may be used depending on how your body tolerates these things to really stimulate bone adaptation. There are aspects of aging and bone health we can’t control, but we can take steps to minimize the chances of bone loss and osteoporosis. Talk to your healthcare team to determine your risk and don’t forget to show your bones a little TLC – you’re going to need them.
Read More About A Therapist's Tips to Prevent and Manage Osteoporosis
-
Department Spotlight: Imaging
The imaging department is where scientific precision and patient connection come together in harmony to help diagnose a multitude of conditions. When a mystery needs to be unraveled, experts in X-ray, CT, MRI, ultrasound, echocardiography, mammography and nuclear medicine step in to provide a deeper lens into each patient’s inner workings. At Renown Health, our imaging specialists exemplify this and more. With the inpatient teams at Renown Regional Medical Center and Renown South Meadows Medical Center and many outpatient locations across Reno and Sparks, our dedicated and compassionate imaging and radiology technologists make this symphony of healing a melodious reality. Through the lens of their expertise and the state-of-the-art equipment at their fingertips, the invisible becomes visible, pain transforms into answers and the path to recovery. A Picture Tells a Thousand Words Every patient image tells a story, and Renown’s Imaging department is full of master storytellers. From X-rays that capture the intricate architecture of bones to MRIs that unveil the complex structure of organs, these team members use sophisticated techniques to make sure every patient receives the highest standard of care. Within the imaging landscape, no day looks the same – and each team can expect a different set of challenges to overcome, all while helping providers gain better diagnostic clarity. “Every day in imaging is a little bit different, and I love that,” said Savannah Terrana, Outpatient CT Scan Technologist at Renown X-Ray and Imaging – Vista. “We start like everyone else: getting our rooms stocked and ready for patients and protocoling the day's exams. We have a lot of different types of scans, like x-ray, CT and bone density, and a variety of conditions that we are evaluating for the ordering providers, like fractures, cancer, bleeds and more. “When we get into work, we get a daily assignment that decides whether we are in one of our outpatient or inpatient rooms,” added Ireland Bennett, Echo Technologist at Renown Regional. “Then when we are on inpatients, we get our assignments for whether we are assigned to transesophageal echocardiograms, the cath lab or pediatrics. When we are on outpatients, we get a set schedule for the day with patients every hour from 7:15 a.m. until 4:15 p.m. We do our best to be efficient as possible to not delay any patient care or discharges.” “X-rays aren’t just for bones; we do chest X-rays to look for pneumonia and intestinal issues, and we also do fluoroscopy, which is a live video X-rays while patients drink contrast or while surgeons fix fractures with screws and other hardware in the operating room,” said Amethyst Winters, Inpatient Diagnostics Imaging Lead at Renown South Meadows. “There is a lot of variety, and we provide imaging for patients in the entire hospital.” Equipped with advanced technologies and the unique skills they acquired in a trade program, at the university-level or in the military, the Imaging department can deliver precise and comprehensive information to help providers make accurate diagnoses. And their role transcends beyond the image scanner. “A typical day for an MRI Technologist depends greatly on outpatient or inpatient settings,” said Sean Fryer, Supervisor of Imaging for Renown X-Ray and Imaging – Pringle. “There is a lot of screen time and usually in dark areas, but this is where our technologist skill set comes into play – manipulating parameters to either increase quality by signal/resolution or decrease them a little to gain time." “A day in the life as an ultrasound tech would of course be performing ultrasounds on our patient community, but there is much more to it,” added Mary Rushton, Ultrasound Specialist at the Renown Breast Center. “This includes keeping rooms clean and stocked with supplies, protocoling exams and studying patient history so you can give the best patient care possible, continuing education and training to keep up with new technologies and being an aide to your radiologist. Working with many different personalities, you recognize that you cannot complete every step of the patient care process all by yourself – it requires collaboration from your team to give the ultimate patient care experience." Mary brings up an excellent point about the wide variety of people her team meets every day, on both the patient and employee side, with the common goal of solving diagnostic mysteries. This aspect of their work has become one of the highlights of their career. “Working in imaging allows us to meet many members of our community,” Teresa Shutts, Breast Health Coordinator at Renown X-Ray and Imaging – Pringle. “We are responsible for providing imaging exams, managing patient needs and creating a comfortable and caring environment for people who are possibly going through the worst times of their lives.” Along with every day being different, our Imaging team members thrive in their dynamic and fast-paced work environment, where efficiency and urgency are vital, especially among a constant stream of patients in need of timely diagnoses. “Our days in CT are very fast paced,” said Shelly Lavin, Imaging Lead for Inpatient Diagnostics at Renown Regional. “Our modality is the first choice for assessing stroke and trauma patients. We are fortunate to have very competent tech aides who help work up CT orders by checking orders, IV status and labs. We generally have inpatients scheduled every half hour, and we work these around a very full ER list. When we get extremely busy, we have to strategize how we schedule our patients in the various scanners to expedite exams and not delay patient care.” “We provide patient care for those who come in for emergencies, trauma, inpatient care, surgery and fluoroscopy studies,” added Sean Elliott, Inpatient Radiology Technologist at Renown Regional. “I was always told in school that our main purpose was to help doctors better diagnose patients, and imaging provides many modalities to appropriately diagnose.” Behind-the-scenes, our Imaging surgery schedulers are the keys to ensuring each appointment runs smoothly, communicating directly with patients to get their exams off to a good start. “Every day it is my task to make sure we have everything we need to do the exam that is ordered for a patient,” said Isela Gonzalez, Surgery Scheduler for Renown X-Ray and Imaging – Double R. “This includes the order, authorization approval, completing the protocol, confirming the appointment, re-stating the address and directions, going over any prep for the exam and giving them their estimate cost for the exam. I always do my best to give the patient the best experience possible.” Whether they are in the weeds of radiology or in the depths of patient coordination, Renown’s Imaging department is unmatched – and the direct beneficiaries are their patients.
-
Learn How to Manage Lymphedema
Katherine Bunker, Physical Therapist and Certified Lymphedema Therapist (PT, DPT, CLT) at Renown, discusses how patients can manage lymphedema with changes to daily routines along with diet and exercise. Lymphedema is a condition that affects millions of people around the world. It is a chronic and progressive disorder that results in swelling of the arms, legs, or other parts of the body due to an accumulation of lymph fluid. Lymphedema can occur because of cancer treatments, surgery, or other medical conditions. Managing Lymphedema Treatments to help reduce symptoms such as pain, swelling and discomfort associated with lymphedema can include compression garments, exercise, skin care, manual lymphatic drainage and pneumatic compression. The goal is to avoid triggering the onset of lymphedema. Lymphedema can present itself immediately after surgery or radiation. It can appear months later or even years later. There are many factors that influence the development of lymphedema which is why prevention is so important. If you have had injury or disruption to your lymphatic system, then: Avoid injuries to the skin near the affected area. For example: wearing gloves during gardening, using bug spray to ward off mosquitos, covering your limbs while playing with pets, keeping nails clean and avoiding cutting too close to cuticle, utilizing electric razors at the armpit (instead of a traditional razor)., Avoid blood pressure readings to the affected limb or request blood pressure to be taken manually, not by a machine. Avoid heat like saunas, hot tubs, sunburns, hot packs, and even massages. Avoid tight jewelry like rings or bracelets, which can be too tight.
-
Department Spotlight: Acute Care Rehab Therapy
Being admitted to the hospital is never easy. Being admitted for a traumatic injury can be even harder. Whether it's learning how to walk again or powering through a new speech therapy routine, recovering from an injury that may affect the course of your life can be daunting. But it doesn’t have to be, thanks to the Acute Care Rehab Therapy team at Renown Health. The smiling faces of the Acute Care Rehab Therapy team at both Renown Regional Medical Center and Renown South Meadows Medical Center will make you see that there is a light at the end of the tunnel. Your dedicated physical therapists, occupational therapists and speech language pathologists are here to serve you and place you back on the right path to recovery and function. The Role of Acute Inpatient Therapy The Acute Care Rehab Therapy team comes in at a critical juncture in a patient’s care process after hospital admission. As one of the primary rehabilitation partners on a care team, these dedicated therapists are here to maximize every patient’s safe and independent living before they set off back home – all while reducing the risk of hospital readmission. “As physical therapists, we address musculoskeletal deficits and assess a patient’s current function after acute injury or illness from their baseline and develop a plan for functional recovery,” said Kristie Eide-Hughes, Physical Therapist at Renown Regional. “We also use our clinical expertise to assist with the discharge process and make sure each patient has the best durable medical equipment the first time around, removing the guesswork.” “On the occupational therapy side, we work with patients to facilitate their independence with basic life skills, such as dressing, bathing and using the restroom,” added Jeanne Clinesmith, Occupational Therapist at Renown Regional. “In the pediatric setting, we help babies and kids get back to what they were doing before they came into the hospital,” continued Rhonda Yeager, Pediatric Occupational Therapist at Renown Regional. “In the NICU specifically, we support the development of babies, trying to prevent problems from worsening. It’s nice to be a source of positivity in an otherwise intimidating situation.” The role of therapy in this setting reaches all ages, from babies in the neonatal intensive care unit (NICU) to adults approaching end-of-life care. Every therapeutic approach is tailored specifically to each patient. “Therapy is more of a habilitative approach for infants in the NICU, while it is more of a rehabilitative approach for kids and adults following injury or illness,” said Sara Carolla, Physical Therapist at Renown Regional. Each team member in the Acute Care Rehab Therapy department is dedicated to each patient, helping them make progress from start to finish and giving them the tools to succeed along the way. “I enjoy the variety of the patients we get to see and the ability to see them make gains from the wonderful treatment they get in the hospital from my team,” said Kelly Schwarz, Occupational Therapist at Renown South Meadows. “We provide education as each patient’s acute issues evolve,” added Nicole Leeton, Speech Language Pathologist at Renown Regional. “One of my favorite parts of my work is the patient and family education aspect, and that includes other healthcare provider education as well. It’s a moving picture.” Moreover, every team member gives each patient tools to learn how to be themselves again and empowers them to continue striving for the best possible result of their therapy “We get the opportunity to make a person’s bad experience in life better even by spending one session with them, giving them the keys to unlock something that they didn’t think they had the ability to do,” said Dana Robinson, Occupational Therapist at Renown Regional. On the Road to Independence Our dedicated therapists in the Acute Care Rehab Therapy team set the stage for a patient’s recovery process after trauma, showing them their potential for independence. With a multitude of patients coming into the hospital with many degrees of medical complexity, each day is different while the end goal is always the same: to optimize function as early as possible while overcoming any barriers and paving the way for a comfortable and effective quality of life. “Early intervention is a big piece,” said Nicole Leeton. “Us seeing patients early can get them recovered and independent more quickly and help prevent future illness and injuries. For example, in speech therapy, getting in early and facilitating communication skills for patients with impaired speech can make a huge difference.” Acute Care Rehab therapists dig deeply to see the whole picture of each patient’s situation to foster their independence – their history, social skills, support system and more. “Sometimes, we are the difference between independence and dependence,” said Dana Robinson. “We are the eyes and ears because we have so much time with the patients. Our team is extremely collaborative and develops a great rapport with patients, so they feel comfortable telling us everything going on with them.” “For kids, we teach parents ways they can help their kids by setting up their homes and the equipment they need to succeed,” added Rhonda Yeager. According to the team, one of the biggest keys to independence is repetition. A continual flow of getting up and trying again is crucial for recovery. “Repetition helps people regain their quality of life back sooner and control their recovery process,” said Megan Hough, Physical Therapist at Renown Health. “Helping people continue to get stronger and more independent makes my job so rewarding,” added Sam Brown, Physical Therapist at Renown Regional. Knowing that they have made a difference and help shape a patient’s overall development inspires each therapist to never give up, regardless of how difficult an injury presents. There is no set schedule for recovery, and the therapists are always in the patient’s corner. “This team has the most passionate, caring and dedicated individuals that I know,” said Kendra Webber, Manager of Acute Inpatient Rehab Therapy Services at Renown Regional. They give 110 percent to every patient every time to ensure they have what they need to regain function and independence.” “By tailoring therapy to the individual, the bounds are virtually limitless for what we can accomplish,” added Dana Robinson. It Takes a Village Since acute inpatient therapy is never a one-size-fits-all approach, it truly takes a village for this team to move the mountains they do for patients every day. These teams are fact-finding masters, gathering all the necessary information from the patient, their family and their care team to figure out their precise needs. “We are a consistent presence for our patients, identifying a lot of different needs and meeting those needs to help patients grow in their treatment process,” said Kelly Schwarz. “By collaborating with each patient’s diverse care team, we are able to employ the clinical judgment to help patients overcome physical, emotional and environmental struggles and set them up with the proper resources once they leave our setting.” “Our team has steady communication with physicians, nurses, acute care technicians, respiratory staff, physician assistants, case managers and more to ensure the best possible care,” added Jet Manzi, Physical Therapist at Renown Regional. Constant communication and collaboration are also necessary beyond the acute treatment process. These skills are vital in order to facilitate discharge planning, and the Acute Care Rehab therapists are an essential resource in the discharge process alongside our Hospital Care Management team. “Often times, a patient’s family needs a lot of guidance in helping their loved ones determine the next level, and we help them navigate those steps and the resources available to them,” said Mark Stumpf, Occupational Therapist at Renown Regional. “And it’s all a team effort.” “Our therapists are the most committed, generous, hardworking people,” added Courtney Phillips-Shoda, Supervisor of Rehab Therapy Services at Renown Regional. “Despite being short-staffed, we come to work every single day and give everything to our patients. They are the priority.” If you take away one thing, know this for certain: Renown’s Acute Care Rehab occupational, speech and physical therapists will always be there to help patients continue on a positive trajectory to physical, mental and emotional recovery. “Whether you are a patient or a provider, if there is a problem, never hesitate to reach out to us,” said Nicole Leeton. “We are always receptive to anyone seeking our help.” With the Acute Care Inpatient Therapy team on their side, a patient’s journey to recovery is only just beginning.
Read More About Department Spotlight: Acute Care Rehab Therapy
-
Recognizing World Lymphedema Day
To recognize World Lymphedema Day, Katherine Bunker, Physical Therapist and Certified Lymphedema Therapist (PT, DPT, CLT) at Renown, shares her experience helping those with lymphedema and lymphatic disease thrive in their daily lives. Each year, World Lymphedema Day continues to be an advocate-driven celebration and global education opportunity on what it means to live with lymphedema and lymphatic disease. We explore why this cause deserves global recognition each year on March 6 below. Types of Lymphedema Lymphedema is an abnormal collection of protein-rich fluid that causes swelling just beneath the skin. The fluid, which is filtered through the lymph nodes, makes up a network of tissues that help the body get rid of toxins, waste and other unwanted substances. According to Katherine Bunker, PT, DPT, CLT at Renown Health, this collection of fluid causes swelling, usually in the arms or legs, but can happen in other areas too. It can also cause discomfort, restricted movement and may increase the risk of infections.
-
The Road to Recovery Close to Home
Meet Connor Smith Life was hectic for Connor Smith. He had just finished at the top of his class at both the fire academy and paramedic school and was looking forward to starting work in northern Nevada. It was winter 2019, and he was ready to have some fun. The plan was to ride ATVs at Sand Mountain with his brother Cody, dad Lance and some friends, but a jump would change everything. Connor’s ATV took off but landed awkwardly, and he remembers immediately knowing he was paralyzed. Connor’s mom, Dana Shugar, was at home when she received the upsetting call from Cody, who told her he had an accident. Connor was flown to Renown Regional Medical Center, the area’s only Level II Trauma Center. After a seven-hour emergency surgery, Dana learned that Connor would live but only had a slight chance of walking again due to a spinal fracture. “The surgeon saved his life. It’s amazing how your life can change in a matter of seconds,” she said. Once his condition stabilized, Connor moved to the Renown Rehabilitation Hospital and began physical rehabilitation. “Thank God for the people at rehab,” Dana said. “Dr. Pence, the therapists, nurses and all the employees were a wonderful support system, explaining everything and answering all our questions. The kindness they showed got me through.” Connor agrees, calling the Renown rehab team nothing short of amazing.
-
Low Back Pain – How to Stop the Ache
Low back pain is not only a problem most people have at some point in life, but also the leading cause of disability in the U.S. Whether it is a sharp spasm from lifting something heavy or a daily constant ache, there are various treatments available to relieve your pain. Jessica Ryder PT, DPT, cert VRS, with Renown Health Outpatient Therapy, explains some common causes of this pain, how to treat it and ways to prevent pain flare-ups. It’s important to realize most cases of low back pain are short term. Frequently lasting only a few days or weeks. In general these cases leave no long-term damage to the spine, muscles, discs or nerves. “However, it can become episodic or chronic (lasting longer than 12 weeks) if it is not properly understood or managed by the individual, ” cautions Ryder. Causes of Pain Specifically back discomfort can be related to: Wear and tear on the spine due to age or poor movement patterns Injury to spinal discs Sprains (overstretching or tearing of ligaments) and strains (tears in tendons or muscles) Trauma Irregularities of the spine present at birth (example: scoliosis)Notably the above issues may result in a “pinched nerve” or sciatica, causing pain to extend down the leg. Risk Factors for Pain In particular, your chance of developing low back pain increases with the risk factors below: Age Being overweight Low fitness level or occasional physical activity (“weekend warrior”) Family history Pregnancy Poor posture Jobs requiring heavy physical work (landscaping, plumbers, construction, etc.)
-
Perseverance and Physical Therapy Help UNR Student Walk Again
University of Nevada, Reno student Khoa Le was paralyzed in 2010 after a longboarding accident. Through physical therapy, a positive attitude and sheer will, Le is walking again. This weekend, Le will walk across the commencement stage to accept his college diploma. “Walking around on my own power is just the greatest feeling,” says Khoa Le, a senior at the University of Nevada, Reno. Just after finishing summer school at the university in July 2010, his whole life changed within seconds after stepping on a longboard skateboard for the first time. He lost control of the board and hit the curb, causing paralysis on the left side of his body. His journey to recovery began at Renown Health Physical Therapy & Rehab. His physical therapist, Dina Barry, says he never complained once in four years. “I started seeing Khoa in April 2011, and we worked for four years together,” says Barry, a lead physical therapist at Renown. “Everything I’ve ever asked him to do, he does. Le is a hard worker, is continuously optimistic and smiling, and I think that is why he’s accomplished what he has.” Le plans to pursue a career as an information systems manager.
Read More About Perseverance and Physical Therapy Help UNR Student Walk Again