Search
-
Life after Lymphedema Diagnosis: What to Expect
Managing lymphedema effectively is essential for enhancing the quality of life for individuals affected by this condition. Katherine Bunker, a Physical Therapist and Certified Lymphedema Therapist (PT, DPT, CLT) at Renown, has expertise in this area and her insights offer valuable strategies for managing lymphedema. Lymphedema is a chronic condition characterized by swelling in one or more limbs due to a blockage in the lymphatic system. This condition can result from cancer treatments, surgery, infection, or can sometimes be congenital. While it can be challenging to live with lymphedema, understanding the condition and adopting specific lifestyle changes and strategies can significantly improve the quality of life. Understanding Lymphedema Educating yourself about lymphedema is crucial. Understanding the causes, symptoms, and potential complications can provide you with the tools to manage the condition proactively. Lymphedema can lead to discomfort, decreased mobility, and in severe cases, infections such as cellulitis. Therefore, recognizing the early signs and knowing when to seek medical advice is essential. Medical Management Consulting with healthcare professionals who specialize in lymphedema is critical. A physiotherapist or occupational therapist trained in lymphedema management can tailor a treatment plan for you that can include the following: Compression Therapy - Wearing prescribed compression garments can help move the lymph fluid and reduce swelling. It’s essential to get fitted by a professional and understand how to use these garments correctly. Manual Lymphatic Drainage (MLD) a gentle massage technique that encourages the movement of lymph fluid out of the affected limb. It’s typically performed by a trained therapist but ask about self-massage techniques you can do at home.
Read More About Life after Lymphedema Diagnosis: What to Expect
-
A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
Embarking on the path to bariatric surgery is a unique and deeply personal journey. Individuals like Mary Escobar choose this life-changing route for reasons ranging from improved cardiovascular health to managing diabetes or finding relief from various health complications. In Mary's case, her two-decade-long healthcare journey not only underscores the challenges she faced but also highlights the support and expertise that ultimately led to her successful transformation through bariatric surgery. Mary's Resilience: December 2002 through February 2003 More than two decades ago, Mary experienced unforeseen health complications just days after giving birth via c-section. Septic shock, hemolytic uremic syndrome, thrombocytopenia, renal failure and a blood clot in her lung plunged her into a critical state. Intensive care, plasma exchange and a long recovery followed. After being discharged with compromised kidney function, Mary faced complete renal failure two years later, leading to dialysis and a spot on the donor list. Mary's brother, a perfect match, selflessly donated his kidney on Dec. 14, 2007, marking a turning point in Mary's health. However, the post-transplant period brought new challenges, including diabetes, high blood pressure and a significant weight gain, reaching 230 pounds. Determined to regain control, Mary explored various diets without success until she consulted with a bariatric doctor. Journey to Bariatric Surgery: November 2009 - April 2021 In November 2009, Mary opted for a gastric band, shedding 40 pounds within a year. Despite initial success, issues with the gastric band arose, prompting a consultation with Dr. John Ganser at Renown Health in April 2021. Together, they decided to transition to a gastric sleeve, with comprehensive education provided to ensure long-term success.
Read More About A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
-
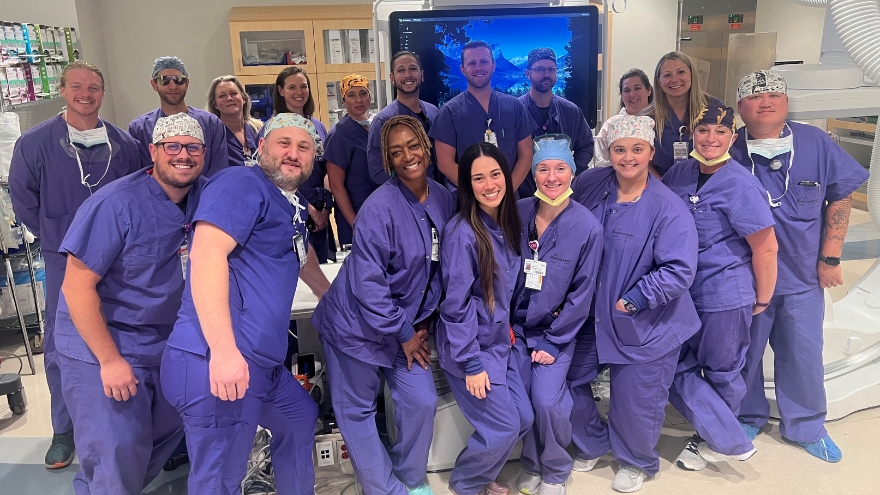
Department Spotlight: Special Procedures
Chronic pain can be one of the most distressing feelings someone may encounter – and more likely than not, you know someone who is managing their pain as a part of their healthcare journey. In fact, according to the Centers for Disease Control and Prevention, about 1 in 5 U.S. adults have experienced chronic pain in recent years. One of the most common methods of treating pain is through prescription pain medications; however, with the rise of the opioid epidemic across the country, leveraging other interventions to help patients manage their chronic pain has become increasingly more important. What if there was a way to treat pain directly without the automatic need for pain medication? Luckily for patients in northern Nevada, our Special Procedures department at Renown Rehabilitation Hospital specializes in exactly that: interventional pain mitigation sans painkillers. With nearly 95% of their patients who come in with pain-related mobility issues being able to physically walk out of the hospital after their treatment, much-needed relief is clearly in store. Tight-knit and forever-caring, the Special Procedures team knows how to transform the purpose of pain management. A Penchant for Pain Alleviation Renown's Special Procedures team offers a wide variety of pain management solutions that are uniquely tailored to each individual patient’s needs. With the help of a team of 14 attentive nurses, interventional radiology technologists and a surgical technician – plus a dedicated patient access representative ensuring everything goes smoothly behind-the-scenes – these lifechanging interventions include: Epidurals (including steroid epidurals) Nerve blocks Ablations Tenotomies Spinal cord stimulator trials Peripheral nerve stimulator trials The nurses on this specialized team guide patients before, during and after their procedures, making sure they are at ease throughout the entire process. Each nurse emulates both expertise and empathy to help light the path towards healing. “Before each procedure, we get the patient’s vitals, health history and work with the doctor to answer any questions they may have about what is going to happen in the procedure room,” said Michon Edgington, RN. “After they’re all done, they come back to me, and I make sure they are ready to go home by educating them on their discharge. Our goal is to get them back to their families very quickly.” “In the actual procedure room, we perform safety checks, do charting, prepare the sterile tray for the doctor and give medication for conscious sedations, all while consistently monitoring the patient and helping the doctor out along the way to help the procedure go well,” added Shannon Boelow, RN. This team’s dedicated imaging professionals harness expertise that goes beyond capturing images. Their skillful utilization of X-ray technology serves as a guide for doctors administering treatments for pain – and according to our own physicians, our imaging technologists are some of the best in the business. “Our X-ray skills here are specialized,” said Julie Smith, Imaging Lead. “Visually, the doctor needs to see what’s going on inside the body so they can accurately place needles and steroids. We all work together collectively and work with each doctor to accommodate their preferences, helping the treatments go much faster and minimizing the patient’s exposure to radiation.” Serving as the ideal representation of both precision and support, the surgical technician on this team is an important collaborator in the procedure room, helping to ensure the success of every interventional procedure with a meticulous eye for detail. “As the Special Procedures surgical technician, I get the room ready with all the necessary instruments, including making sure everything is sterile,” said Carrie Crow, Surgical Technician. “I enjoy keeping the team organized.” Overseeing it all are the physicians, who are eternally grateful for the team for the life-changing interventions they offer every day. “Our physicians are so phenomenal,” said Brittney Summerfield, Manager of Nursing. “They are very supportive and collaborative, and they always do the right thing. They have total confidence in us.” Seeing patients walk out of the hospital happy and healthy is a driving motivator for this team. Whether they had significant experience in pain management or were ready for a completely new challenge, each team member comes to work every day inspired to move mountains. “I had worked in pain management in other facilities, and I was extremely excited to come here and solely focus on pain,” said Jodi Eldridge, Supervisor of Special Procedures. “I enjoy seeing the patients so happy when they leave no longer in pain. I feel immediate gratification, because you truly feel like you’re doing something big for the patient. It’s very rewarding.” “I decided to come work here because I worked in the inpatient setting for a long time, and I was ready to see a different side of healthcare and provide a different type of care to our community; plus, my coworkers are the best,” added Lisa Dunnivant, RN. There’s no question that the realm of pain management is a delicate one – and there is no team better suited to take on that challenge than Special Procedures, working harmoniously to bring relief and a renewed sense of livelihood for every patient they serve. “Some people believe pain management is just all about pills, and that is simply not true,” said Carrie Crow. “Our procedures are yet another way to help them manage their pain and find relief.”
-
Department Spotlight: Interventional Radiology
National Radiologic Technology Week is from Nov. 5-11, 2023. Join us in celebrating Renown's Interventional Radiology department!Try to put yourself in the shoes of someone who is told that they have a massive blood clot in their lung, someone who needs a biopsy to determine the next steps of their care, someone facing a stroke or brain aneurysm or someone who needs a catheter to receive treatment such as chemotherapy. You may immediately think that an intense and intimidating surgery is on the horizon. What if, instead of surgery, your care teams were able to use the necessary tools to treat your blockage or administer your medicine with an image-guided procedure? That’s precisely what the Interventional Radiology (IR) team at Renown Health does. Behind the doors of this department is where you’ll find a team of highly skilled individuals who operate like a well-oiled machine, ensuring that each procedure is executed with precision and care. Their commitment to excellence knows no bounds as they provide essential interventions to patients of all ages, from the tiniest newborns to the elderly. Their mission extends beyond diagnostic and therapeutic procedures; they are experts in understanding and serving the ever-evolving needs of their patients. Minimally Invasive, Maximally Impactful With their advanced expertise, our IR teams at both Renown Regional Medical Center and Renown South Meadows Medical Center harness the power of X-ray, CT and ultrasound technologies to navigate their way through life-saving minimally invasive procedures, such as thrombectomies, angioplasties, stent placements, embolizations, catheter and drain insertions and needle biopsies. In the world of medicine, Interventional Radiology often offers an alternative to traditional surgical methods, reducing the risk of hospitalization and helping patients embrace recovery more quickly. Our IR teams have a diverse and busy daily work life in order to make these complex and life-saving interventions happen – and they all have each other’s backs to ensure that every patient gets the care they deserve. “Every day is different, and no two days are alike,” said Ryan Nunes, Specialty Procedure IR Technologist at Renown Regional. “The day can start off first thing in the morning with several emergent cases, such as ruptured brain aneurysms to brain blockages. We all work really well together; we help each other out and come together to do things as a team.” Like every other team at Renown, patient well-being is always a number one priority. The IR department takes this commitment seriously, upholding the highest standards of ethics and safety. “We start the day by preparing rooms and making sure they are well-stocked, checking that all devices are working, performing safety checks and making sure the entire team is well-prepared for whatever cases come through the door,” said Aubrey Goldsmith, Supervisor of Clinical Nursing in IR at Renown Regional. “We have routine cases like drain placements, biopsies, line placements and more, and we also have life-threatening cases that come at a moment’s notice. Our nurses are responsible for monitoring patients throughout the procedure to make sure they are doing well the entire time and are there to respond if the patient has a decline.” "After completing the prior assessment of each patient, we look for any medical problems the patient may have before confirming it is safe for the patient to have procedure done,” said Brandon Hartwig, Interventional Radiology RN at Renown South Meadows. “We work closely with the physicians on all our cases while assessing each patient, going through labs and vitals and personalizing the procedure for each patient.” Even though the procedures they oversee are minimally invasive, the IR team understands that any procedure, regardless of the severity, can be incredibly frightening for any patient. Their best tool for handling patient anxieties? Communication. "The best thing we can do to reduce anxieties and fears in patients is to have communication with them to ensure they know what is going on and what to expect,” said Megan Rios, IR Technologist at Renown Regional. "We set clear expectations for the patients and give reassurance throughout the entire procedure.” "All of our team members are very attentive to our patients when it comes to potential fears and anxieties that they may have,” added Jazmynn Kimsey, IR Technologist at Renown Regional. “We always take the extra time to listen to our patients and break things down, explaining every step before, during and after the procedure.” Knowledge sharing is also a crucial part of the IR process. No patient will ever have to wonder, “what exactly is going on here?” “We provide each patient with education and advocacy throughout the process,” said Blaire Henderson, Interventional Radiology RN at Renown Regional. “We ensure every patient is as comfortable as possible at all times.” “When it comes to procedures, patients tend to be scared and nervous,” added Ryan Nunes. “The silver lining to what we do is that it is all done through very small openings of the skin, and we all explain this to patients. Most procedures we do are done under moderate sedation which helps put the patient more at ease.” In a world where advanced medical care meets the human touch, the IR team exemplifies Renown’s commitment to making a genuine difference in the health and well-being of everyone they serve.
Read More About Department Spotlight: Interventional Radiology
-
A Journey of Transformation Through Robotic Surgery at Renown Health
Carrie Hintz is constantly on the move. “I don’t sit well,” she said when discussing her career as an Emergency Room nurse at Renown South Meadows Medical Center. She has also earned a PhD in nursing research, a Nurse Executive DNP and an MSN in nursing and healthcare leadership, all while managing the joyful chaos of raising two toddlers under the age of four. She's always been on the move, but her journey to transformation through bariatric surgery with the da Vinci Surgical System is a testament to her determination and the vital need for cutting-edge robotic surgical tools at Renown Health. Carrie's life is non-stop, but her struggle with weight loss was a persistent challenge, compounded by the complexities of medical conditions like PCOS and a pituitary tumor, both of which made losing weight an uphill battle. It was while reading the news one night, witnessing a mother's disappointment at Disney Land due to weight restrictions, that Carrie decided to take charge of her life. She knew she had to make a change. In 2016, Carrie embarked on her bariatric surgery journey, seeking consultation with a Renown surgeon. However, her dreams of starting a family prompted her and her supportive husband to postpone surgery since one cannot have a baby within 18 months of the procedure. After welcoming two beautiful children into their lives, Carrie returned to Renown in 2022 to discuss her surgical options. Finally, in February 2023, and after six months of mandatory weight loss preparation, Carrie was ready to undergo the life-changing surgery. Dr. Alexander Ayzengart, her dedicated surgeon, had a plan that involved utilizing the da Vinci Surgical System for her bariatric procedure, coupled with repairing a hernia that had developed during her weight loss journey. The stage was finally set for Carrie's transformation. To everyone's surprise, the hernia turned out to be larger than anticipated, but miraculously, Carrie experienced no post-operative pain and minimal scarring. She reminisces about her early post-surgery days, confidently attributing her excellent outcomes to the remarkable da Vinci Surgical System. “I was up and walking around the night after the surgery,” she said. The da Vinci is no ordinary surgical tool; it's a state-of-the-art, minimally invasive robotic system skillfully operated by trained surgeons. Renown's commitment to innovation in healthcare paved the way for Carrie's remarkable journey.
Read More About A Journey of Transformation Through Robotic Surgery at Renown Health
-
A Therapist's Tips to Prevent and Manage Osteoporosis
Want to know more about osteoporosis and osteopenia? We'll dive into these conditions and give you some handy tips on preventing future problems and taking care of your bones. What is Osteopenia? Osteopenia (low bone density) is the initial stage of bone mineral density loss, which can eventually progress to osteoporosis if steps are not taken to prevent it. What is Osteoporosis? Osteoporosis is a condition that weakens our bones. While it literally means “porous bone," it doesn’t mean that our bones are doomed to succumb to the changes that can happen to us silently over time. Our bones are living tissues that are constantly breaking down and remodeling themselves. Osteoporosis and osteopenia are typically diagnosed by testing bone mineral density using scans that your primary care provider can easily order. This is important testing because it dictates your risk of breaking a bone in common areas like your hip, wrist or spine. It also helps set the stage for talking with your healthcare team to develop a treatment plan. Most people will reach their peak bone mass in their mid to late twenties. There are several factors that increase our risk of osteoporosis or osteopenia as we age, such as menopause, genetics and other lifestyle factors. However, there are several things you can do to mitigate this breakdown and assist your body in the constant remodeling it does to our bones. 3 Controllable Factors to Build Strong Bones 1. Talk to your primary care provider They can go over a plan and prescribe things such as vitamin D, calcium and medications that can help if you are at risk or have osteoporosis or osteopenia. 2. Maintain a healthy diet Talk to a dietician if you need further help as they can be an invaluable resource to develop a plan. Eat foods rich in calcium, vitamin D and vitamin C. These assist with the rebuilding of bone. Examples include but aren’t limited to leafy greens, legumes, salmon and healthy dairy products. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per week. Alcohol interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. 3. Exercise Talk to your primary care provider to get a referral to physical therapy if you need help with exercise. Our bones adapt to the stresses we put them through. Therefore, exercise should be tailored to putting the right stress on our bones. There is good quality research that most exercise is safe when dealing with less bone mineral density. The exercises should be progressively challenging and increase the load for resistance and weight training at least two to three days a week. Examples include squats, step-ups, chest presses and rows. Exercises higher in velocity will lead to more power and bone adaptation. Examples include quicker push-ups, marching and quicker walks. Exercises that are weight-bearing will lead bones to adapt to the stress placed on them. Movements such as mini stomps, step-ups, jumping, jogging and so forth may be used depending on how your body tolerates these things to really stimulate bone adaptation. There are aspects of aging and bone health we can’t control, but we can take steps to minimize the chances of bone loss and osteoporosis. Talk to your healthcare team to determine your risk and don’t forget to show your bones a little TLC – you’re going to need them.
Read More About A Therapist's Tips to Prevent and Manage Osteoporosis
-
Department Spotlight: Imaging
The imaging department is where scientific precision and patient connection come together in harmony to help diagnose a multitude of conditions. When a mystery needs to be unraveled, experts in X-ray, CT, MRI, ultrasound, echocardiography, mammography and nuclear medicine step in to provide a deeper lens into each patient’s inner workings. At Renown Health, our imaging specialists exemplify this and more. With the inpatient teams at Renown Regional Medical Center and Renown South Meadows Medical Center and many outpatient locations across Reno and Sparks, our dedicated and compassionate imaging and radiology technologists make this symphony of healing a melodious reality. Through the lens of their expertise and the state-of-the-art equipment at their fingertips, the invisible becomes visible, pain transforms into answers and the path to recovery. A Picture Tells a Thousand Words Every patient image tells a story, and Renown’s Imaging department is full of master storytellers. From X-rays that capture the intricate architecture of bones to MRIs that unveil the complex structure of organs, these team members use sophisticated techniques to make sure every patient receives the highest standard of care. Within the imaging landscape, no day looks the same – and each team can expect a different set of challenges to overcome, all while helping providers gain better diagnostic clarity. “Every day in imaging is a little bit different, and I love that,” said Savannah Terrana, Outpatient CT Scan Technologist at Renown X-Ray and Imaging – Vista. “We start like everyone else: getting our rooms stocked and ready for patients and protocoling the day's exams. We have a lot of different types of scans, like x-ray, CT and bone density, and a variety of conditions that we are evaluating for the ordering providers, like fractures, cancer, bleeds and more. “When we get into work, we get a daily assignment that decides whether we are in one of our outpatient or inpatient rooms,” added Ireland Bennett, Echo Technologist at Renown Regional. “Then when we are on inpatients, we get our assignments for whether we are assigned to transesophageal echocardiograms, the cath lab or pediatrics. When we are on outpatients, we get a set schedule for the day with patients every hour from 7:15 a.m. until 4:15 p.m. We do our best to be efficient as possible to not delay any patient care or discharges.” “X-rays aren’t just for bones; we do chest X-rays to look for pneumonia and intestinal issues, and we also do fluoroscopy, which is a live video X-rays while patients drink contrast or while surgeons fix fractures with screws and other hardware in the operating room,” said Amethyst Winters, Inpatient Diagnostics Imaging Lead at Renown South Meadows. “There is a lot of variety, and we provide imaging for patients in the entire hospital.” Equipped with advanced technologies and the unique skills they acquired in a trade program, at the university-level or in the military, the Imaging department can deliver precise and comprehensive information to help providers make accurate diagnoses. And their role transcends beyond the image scanner. “A typical day for an MRI Technologist depends greatly on outpatient or inpatient settings,” said Sean Fryer, Supervisor of Imaging for Renown X-Ray and Imaging – Pringle. “There is a lot of screen time and usually in dark areas, but this is where our technologist skill set comes into play – manipulating parameters to either increase quality by signal/resolution or decrease them a little to gain time." “A day in the life as an ultrasound tech would of course be performing ultrasounds on our patient community, but there is much more to it,” added Mary Rushton, Ultrasound Specialist at the Renown Breast Center. “This includes keeping rooms clean and stocked with supplies, protocoling exams and studying patient history so you can give the best patient care possible, continuing education and training to keep up with new technologies and being an aide to your radiologist. Working with many different personalities, you recognize that you cannot complete every step of the patient care process all by yourself – it requires collaboration from your team to give the ultimate patient care experience." Mary brings up an excellent point about the wide variety of people her team meets every day, on both the patient and employee side, with the common goal of solving diagnostic mysteries. This aspect of their work has become one of the highlights of their career. “Working in imaging allows us to meet many members of our community,” Teresa Shutts, Breast Health Coordinator at Renown X-Ray and Imaging – Pringle. “We are responsible for providing imaging exams, managing patient needs and creating a comfortable and caring environment for people who are possibly going through the worst times of their lives.” Along with every day being different, our Imaging team members thrive in their dynamic and fast-paced work environment, where efficiency and urgency are vital, especially among a constant stream of patients in need of timely diagnoses. “Our days in CT are very fast paced,” said Shelly Lavin, Imaging Lead for Inpatient Diagnostics at Renown Regional. “Our modality is the first choice for assessing stroke and trauma patients. We are fortunate to have very competent tech aides who help work up CT orders by checking orders, IV status and labs. We generally have inpatients scheduled every half hour, and we work these around a very full ER list. When we get extremely busy, we have to strategize how we schedule our patients in the various scanners to expedite exams and not delay patient care.” “We provide patient care for those who come in for emergencies, trauma, inpatient care, surgery and fluoroscopy studies,” added Sean Elliott, Inpatient Radiology Technologist at Renown Regional. “I was always told in school that our main purpose was to help doctors better diagnose patients, and imaging provides many modalities to appropriately diagnose.” Behind-the-scenes, our Imaging surgery schedulers are the keys to ensuring each appointment runs smoothly, communicating directly with patients to get their exams off to a good start. “Every day it is my task to make sure we have everything we need to do the exam that is ordered for a patient,” said Isela Gonzalez, Surgery Scheduler for Renown X-Ray and Imaging – Double R. “This includes the order, authorization approval, completing the protocol, confirming the appointment, re-stating the address and directions, going over any prep for the exam and giving them their estimate cost for the exam. I always do my best to give the patient the best experience possible.” Whether they are in the weeds of radiology or in the depths of patient coordination, Renown’s Imaging department is unmatched – and the direct beneficiaries are their patients.
-
Department Spotlight: Medical-Surgical Nursing
The title of “largest nursing specialty in the country” belongs to medical-surgical nursing (commonly known as “med-surg”). Devoted to providing care for patients with a variety of health conditions and who are preparing for or recovering from surgery, this ever-popular nursing niche attracts impassioned, talented individuals who make a genuine difference in the health and well-being of every patient. Med-surg nurses at Renown Health emulate this dedication and more. From general surgery to oncology and orthopedics, the med-surg team at Renown Regional Medical Center and Renown South Meadows Medical Center play a critical role in our care delivery for patients facing challenging diagnoses or procedures. Their ability to seamlessly juggle multiple tasks while providing the highest quality of care makes them excellent patient advocates, guiding them through the path to healing. High-Paced with High Results Our med-surg team has the ability and willingness to provide high-caliber nursing for patients with virtually any medical condition – orthopedic injury, trauma surgery, infections, sepsis, pulmonary disease, you name it. No matter the diagnosis or procedure, med-surg has the experience and enthusiasm to handle the fast nature of the job well. Med-surg nurses are always on the go, handling a growing list of conditions together as a team. They work side by side to assess each patient’s condition and assist with both education and discharge planning for patients and families. “Med-surg is a high-paced and unpredictable environment with the largest variety of diagnoses and patient populations,” said Danyel Gish, Manager of Nursing at Renown Regional. “Every patient is everyone’s patient in med-surg. We help each other by answering each other’s call lights, communicate clear expectations and build strong trusting relationships with one another.” “You never know what kind of disease or conditions your patient may present with,” added Brittani Manatt, Registered Nurse in the Cancer Nursing Unit at Renown Regional. “We care for patients with almost any medical diagnosis.” Being admitted to the hospital, regardless of the reason, can be a scary and vulnerable time for anyone. However, patients can breathe a sigh of relief knowing that their competent and confident med-surg nurses are here by their side before and after they experience surgery or treatment. “We communicate with our patients at every step of their care journey to ensure they understand what is going on and help alleviate any fears or concerns,” said Jenni Gilligan, Associate Nurse Manager at Renown South Meadows. “Some of my tips include asking the patient how they are feeling and validating those feelings; getting them and their families and friends involved in the process; and ensuring them that we are here for them and will take the best possible care of them." “What we do as a team to reduce patients’ fears revolves around clear communication and support, whether it’s grabbing them a Starbucks drink, taking them outside for a walk or simply just listening to their concerns,” added Rose Simonian, Supervisor of Clinical Nursing at Renown Regional. “Connecting with our patients through kindness and laughter helps alleviate some of the anxiety that comes with being in the hospital.” Jenni and Rose are exactly right – that clear communication is the “secret sauce” to success within the med-surg team. Their patients are the direct beneficiaries of this crucial skill. “Everything we do throughout our shift focuses on teamwork and communication, making sure every piece of our plan comes together for optimal patient care,” said Cristina Vazquez, Registered Nurse at Renown Regional. “We collaborate a lot within each healthcare team,” added Reena Clark, Registered Nurse at Renown South Meadows. “We also make sure the patients participate and are involved in their plan of care. This is important to set a common goal and help each other achieve that goal for the patient. The nurses on the floor are the eyes, ears and hands of inpatient care." When faced with a daunting diagnosis or procedure, it’s important to have a strong support system within your personal care team, cheering you on every step of the way. Our med-surg team members are masters at this, finding new ways to connect with patients and help them feel empowered to Fight the Good Fight. “We always try to find something that the patient loves or is passionate about that helps shift their mindset,” said Paola Espinoza-Patino, Associate Nurse Manager in the Cancer Nursing Unit at Renown Regional. “It will help them focus their attention on something that brings them joy, even if it’s for a short period of time. This helps them let their guard down and trust the team. We are here to take the best care of them as possible.” "Med-surg provides a safe place to openly discuss any fears or anxieties a patient may be experiencing,” added Danyel Gish. “Our nurses are kind, compassionate and highly-trained professionals that work hand-in-hand with our patients to maintain their safety and wellness. We understand that being in the hospital can be a difficult experience, but we work hard to provide a calming presence and reassurance. We identify different ways to connect with our patients by holding their hands, listening, educating and providing individualized care and interventions.” Much like many other departments across Renown, for med-surg, their patients’ accomplishments are their accomplishments. Witnessing one of their patients reach a significant milestone in their healthcare journey inspires them to continue doing what they do best: provide care driven by equal parts determination and hope. “The biggest accomplishment for me is seeing a patient complete their last round of chemotherapy with us and getting to ring our ‘Chemo Bell,’” added Trevor Owens, Unit Clerk at the William N. Pennington Cancer Institute. “There is no greater joy than witnessing the happiness and relief of a patient completing a step in their healthcare journey." Working tirelessly to provide exceptional care to every patient – and celebrating all their wins along the way – alongside their dedication to Renown’s cultural commitments of Caring and Collaboration are what make our med-surg nurses prosper day-in, day-out.
Read More About Department Spotlight: Medical-Surgical Nursing
-
Love Endures: A Remarkable Recovery Leads to a New Future
It’s true that a road trip can change your life, and it did for Sergeant Brandon Ott, just not in the way he was expecting. For nine years, Brandon worked alongside his friend, Denton Tipler, at the police department in Florence, Oregon. To break the monotony of the COVID-19 lockdown, they planned a ‘guy’s trip’ - a pandemic safe, motorcycle adventure traveling through Idaho and Washington. On the morning of July 22, 2020, they set out on their journey. But by 8 p.m., they ran into rough weather - with wind, poor visibility and heavy rain as they rode into Nevada. Four miles from their destination, on a desolate stretch of Highway 140, a gust of wind hit Brandon. Denton watched in disbelief as his friend bounced, tumbled and ultimately came to a stop after sliding over 100 yards. He flagged down the next vehicle, a semi-truck, and the driver did traffic control while another passerby drove to get cell service and call 911. A Distressing Call About 10 p.m. the same night, Angie Brog, Brandon’s partner, picked up her phone at the Florence police station. A Nevada highway patrolman let her know Brandon was in a motorcycle accident and had been taken to a hospital in Winnemucca, NV. From there he took a life flight to Renown Regional Medical Center. Angie immediately called Brandon’s parents and told Addison, their 9-year-old daughter, the news. They quickly packed their bags and drove to Nevada. On the drive to Reno, an ER doctor called Angie to give her Brandon’s status, “I can’t thank him enough. I was so worried. He even gave me his personal cell phone number.” Upon arrival, she ran to see Brandon in the trauma ICU. “His face was shattered, he had a collapsed lung, a tube was down his throat and something was in his head to relieve pressure from his swelling brain,” she remembers. “He was not expected to live.” While Brandon was in a coma for three days, Angie was by his side, trying to come to grips with a new normal. “The doctors did not sugarcoat it,” she recalls. “They told me to prepare myself if he pulled through.” It was a rough week in the ICU with Brandon heavily sedated, so he could heal. From there he was transferred to the neurology floor, where he slowly improved. While there, his daughter Addison got to see him for the first time. Angie says, “When Addison saw her daddy for the very first time, she was relieved, happy she could hug him, and that he was alive.” Miraculously his legs were not broken and he was able to hold simple conversations and walk a few steps. As the days went on, Brandon’s dad returned to Oregon, and the Inn at Renown became the family’s new home. “It was such a blessing to be so close to Brandon,” Angie observes. “It allowed us to relax a little being in the same building and let us settle in.” The Comeback Brandon’s first memory after the accident was waking up in the Renown Rehabilitation Hospital, 16 days after his accident, not knowing where he was. (Brandon experienced amnesia due to his brain injury and doesn’t remember the days prior to his rehab stay.) He recalls looking around the hospital room and seeing the photos Angie posted of their family on the walls and wondering, “How did they get pictures of my family?” Immediately after learning that Brandon was awake, Angie raced back to the hospital, went outside his window and talked to Brandon on the phone, reassuring him that they were there for him and everything was going to be ok. The next morning, he saw Addison for the first time that he remembered since his accident. They each put their hands to the hospital window “touching” each other in an emotional reunion. During the pandemic, each rehab hospital room was designated with an animal, so family and friends could visit outside safely. Brandon was in the ‘moose’ room. “Whoever thought of that was a genius,” notes Brandon. A new phase of Brandon’s recovery began at the rehab hospital. "He worked so hard while he was there,” Angie shares. With a minimum of three hours of daily therapy sessions, including speech, occupational and physical therapy. Angie participated in every aspect of his therapy, “I learned so much from the therapists; they included me in everything,” she recalls. “The compassion and patience they have is amazing. It takes a special type of person to do this job. I cannot say enough good things about the Renown Rehabilitation Hospital staff. If he would have been anywhere else, I’m not sure he would be alive,” she says. It wasn’t easy. Brandon had a brain injury that required a bolt in his skull to relieve the pressure, and a broken left collar bone and left eye socket. His entire face had to be reconstructed. He remembers his face hurting and thinking he looked like Freddy Krueger. When he saw himself in the mirror for the first time, he was surprised to find he only looked thinner, with a gauze pad on his temple. Prior to the accident, Brandon weighed 300 pounds, but had just finished a year-long fitness journey losing 119 pounds, by doing CrossFit and overhauling his diet. During rehab his weight dropped to 160 pounds and he was known as “the double portion” guy, eating extra food to gain weight. Shaun Stewart, Therapeutic Recreational Therapist, recalls Brandon riding the recumbent cycle during his recovery. “I remember him saying he didn’t know if he was ever going to be able to ride a bike again and was appreciative when adaptive sports were discussed. He was very willing to participate and excited to be able to get on a bike again. He had a positive attitude and always was willing to get up and get back on the bike.” Better Together Although Angie and Brandon were in a committed relationship for almost 11 years, they were not legally married at the time of his accident. “In our minds, our lives were perfect,” Angie asserts. “We had lived together for so long and have a child together.” However, because of COVID-19 restrictions, Angie had to lie and tell the medical staff that they were married so she could be by his side. When Brandon woke up from a coma, she told him, “No matter what I’m your wife.” He asked, “What do you mean, you are my wife?” After hearing Angie’s explanation, Brandon said, “Then, let’s do it.” “We realized when faced with death that the benefits far outweighed the negatives in becoming husband and wife,” Angie discloses. “The rest is history.” On Tuesday, August 18, 2020, Brandon and Angie were married underneath the trees behind the rehab hospital. Their family, friends and several staff members attended the ceremony. “I think that’s a first for us,” declares Dr. Gavin Williams. “I cleared him for capacity to make decisions, and we had a COVID-friendly wedding on our back lawn before he went back home to Oregon.” The next day, Brandon officially left the hospital. “I felt good. Like ‘he’s gonna make it,’ but I was also scared,” mentions Angie. The family stayed in town for a couple of days to make sure everything was ok and then traveled home to Oregon.
Read More About Love Endures: A Remarkable Recovery Leads to a New Future
-
Zarah Path from Traveler to OR Nurse
As many nurses can attest, the journey they have taken to arrive at where they are today is full of twists and turns. For Zarah Jayco, an operating room nurse at Renown Regional Medical Center, her journey is nothing short of a fulfilling and exciting one. Zarah is no stranger to taking detours to find what truly makes her feel the bursts of passion she had been looking for her entire life. She found that passion in the operating room – and travel nursing led her to Renown Health. Today, she is a firm believer that she is exactly where she is supposed to be. “I Just Want to Help People” Throughout her life, Zarah knew she was destined for a meaningful career – but didn’t exactly know what. One day, she sat down with her mom, a nurse herself, where she asked the question that would ignite Zarah’s curiosity: What is important to you? “That’s when I told my mom: ‘honestly, I just want to help people.’” It was at that moment that she realized nursing could be a fit for her. Everything about venturing into the nursing field started to make sense. So, that’s precisely what she did. Zarah went to nursing school. When she stepped into the OR during her clinical rotation, she was immediately inspired. Zarah’s core values as a nurse were rooted from caring for her 90-year-old grandmother while she was in hospice. Her grandmother gave her some powerful lessons and words as she set off on her career: “You are in the right place.” Upon completion of her perioperative program, Zarah the OR Nurse we know and love started her journey. She began her trek as a travel nurse, going up and down California to do exactly what she was meant to do: care for surgical patients. “I Traded the Ocean Waves for the Mountains” As Zarah continued to travel and find different locations for new assignments, her husband received an opportunity for work to transfer to the Biggest Little City. The duo packed up their California lives and moved to northern Nevada, where Zarah signed up for a night shift OR nurse position at Renown Regional Medical Center. But the traveler’s mindset wouldn’t last long. Renown embraced Zarah with open arms, and she was immediately drawn into the community-feel that our health system offered. She felt welcomed and surrounded by “loving, hardworking people” across her department and all other teams she encountered. As Renown cares for patients across 100,000 square miles, Zarah was especially impressed with how rooted Renown is in northern Nevada, noting how it “truly feels like we are caring for the community” with our health system’s wide reach. She was inspired to live up to that mission and more. “Reno and Renown really reeled me in, and I fell in love with the city and everything it has to offer,” said Zarah. “I traded the ocean waves for the mountains, and the more we got to know Reno, the more we realized that this change of pace and lifestyle was definitely a good fit for us.” Zarah the OR Travel Nurse became Zarah the Renown OR Core Staff Charge Nurse. And she knew she made the right decision. Working in the OR, according to Zarah, is challenging in the best way possible. At night, all surgery cases at Renown are emergencies. The team springs into action to answer one vital question: How do we provide the best care for this patient? “It is essential for us to anticipate potential outcomes,” said Zarah. “When we book a surgical case, we look at everything to make sure we are absolutely prepared and ready.” Staying at Renown was an easy choice for Zarah. To her, there is nothing like being a part of a core team that inspires her every day and ‘has each others’ back,’” Zarah stated. “During the course of my assignment at Renown, the culture harnessed a kind of environment that felt like a hardworking family. This was the hook that reeled me into considering being part of core staff. I am incredibly grateful for the opportunity to build relationships that I hold in the highest esteem.”
-
Learn How to Manage Lymphedema
Katherine Bunker, Physical Therapist and Certified Lymphedema Therapist (PT, DPT, CLT) at Renown, discusses how patients can manage lymphedema with changes to daily routines along with diet and exercise. Lymphedema is a condition that affects millions of people around the world. It is a chronic and progressive disorder that results in swelling of the arms, legs, or other parts of the body due to an accumulation of lymph fluid. Lymphedema can occur because of cancer treatments, surgery, or other medical conditions. Managing Lymphedema Treatments to help reduce symptoms such as pain, swelling and discomfort associated with lymphedema can include compression garments, exercise, skin care, manual lymphatic drainage and pneumatic compression. The goal is to avoid triggering the onset of lymphedema. Lymphedema can present itself immediately after surgery or radiation. It can appear months later or even years later. There are many factors that influence the development of lymphedema which is why prevention is so important. If you have had injury or disruption to your lymphatic system, then: Avoid injuries to the skin near the affected area. For example: wearing gloves during gardening, using bug spray to ward off mosquitos, covering your limbs while playing with pets, keeping nails clean and avoiding cutting too close to cuticle, utilizing electric razors at the armpit (instead of a traditional razor)., Avoid blood pressure readings to the affected limb or request blood pressure to be taken manually, not by a machine. Avoid heat like saunas, hot tubs, sunburns, hot packs, and even massages. Avoid tight jewelry like rings or bracelets, which can be too tight.
-
Department Spotlight: Surgical Preadmission
Heading into surgery of any kind can bring along feelings of intimidation. With a best-in-class surgery team at Renown Health, patients rest assured that they are in the most capable hands for their entire procedure from start to finish – and while the physical preparation is vital, mental and emotional preparation is equally as important to ensure each patient has a smooth and comfortable experience. The Surgical Preadmission department (a.k.a. “preadmit”) at Renown Regional Medical Center and Renown South Meadows Medical Center is a dynamic and compassionate group of nurses, case managers, chart managers and more who are dedicated to guiding each patient through the surgical process. With extensive knowledge and expertise under their belt, the teams are equipped to make a genuine difference in the health and well-being of all patients, for all surgeries, at all times of the year. Surgery Starting Ground The Surgical Preadmission teams are crucial aspects in the successful outcome of every surgical procedure. Comprised of skilled healthcare professionals, this department is dedicated to providing comprehensive support and care before heading into the pre-operating room. “Our job is to prepare every patient for surgery, make sure all their pre-surgery testing is done, ensure they understand their fasting and medication instructions, have had their questions answered, have a ride home and know what to expect during surgery and after so their recovery can go smoothly and without complications,” said Debra Bennett, RN, Supervisor of Surgical Preadmission at Renown Regional. “Each patient is unique, so each experience is different.” Our preadmit nurses are the masters of communication, directing thorough assessments – including medications, tests and clearances – and addressing any questions or concerns patients may have, never missing the opportunity to inform them of exactly what they will expect in surgery. “I do a complete history on every patient while giving them detailed pre-operating instructions and helping them answer any questions to the best of my ability,” said Nancy Hilts, Surgical Preadmission RN at Renown Regional. “I am proud to be able to help allay their fears and concerns using my 30 years of pre-op experience. I offer an avenue for them to feel comfortable opening up to me.” “We always tell patients that they have great surgeons and a fantastic team that will be watching over them and taking care of them every step of the way,” added Jon Capallupo, Surgical Preadmission RN at Renown South Meadows. “We also give them plenty of educational handouts and video content, in addition to verbal instruction, to ensure they are as prepared as possible.” The nurses then pass the reigns onto the chart managers, who prepare the charts for surgery and ensure all documentation is up-to-date before sending them to the pre-operative team. The expert surgical case managers also step in to prepare a thorough discharge plan, along with reviewing pre-operation orders for status, consent, codes and more. The team does several of these initial visits virtually, and they are looking forward to soon phasing all preadmit case manager preliminary visits into a virtual model. From assisting the pre-op and post-anesthesia care unit (PACU) teams with discharge planning concerns to helping on the outpatient side with anything from oxygen equipment and catheters to transportation issues and those experiencing homelessness, our pre-admit case managers are always up to the challenge. "We are true patient advocates, alleviating concerns and fears along the way,” said Mary Carl, RN, Case Manager at Renown Regional. “Just to name a few things we do on a daily basis, we see our total joint and non-weight bearing patients during their preadmission appointment, so they are aware of the medical equipment they need and if it is covered by insurance; provide education for Aspira catheters and gastrostomy tubes; advocate to ensure tube feeding and dressing changes are set up for hospice and home health patients; and escalate concerns of patient safety to ensure a safe discharge.” In the midst of it all, there is never a dull moment in the preadmit teams. At Renown Regional alone, the preadmit professionals see more than 1,600 patients a month – and each one has a hyper-personalized experience with their very own preadmit team. “Many times, we are the first impression a patient has on our organization; after all, we touch more than 97 percent of patients that are scheduled for surgery, cardiac catheterization lab procedures or interventional radiology,” said Amy Schler, Surgical Preadmission RN at Renown Regional. “We also collaborate with many other departments in the hospital as well, from surgeons and anesthesiologists to case managers and nurse navigators. Our work in preadmit impacts the entire surgical process.” Holding a diverse array of experiences, our preadmit department plays an integral role in our commitment to providing the highest quality of care to every patient. Knowledge is Power Heading into surgery feeling fearful and worried is normal for any patient. However, how would you feel knowing that each individual member on your preadmit team has, on average, 23-25 years of experience in the field? This is the reality for our Surgical Preadmission department – and they put that vast knowledge to great use to bring a sense of calm to patients. “Our team members have worked in various departments within our organization, and they bring a wealth of knowledge that we share with each other, and most importantly, with our patients,” said Amy Schler, RN. “If you have hundreds of years of nursing experience, you can speak not only as a nurse but also as a patient. It allows you to give a more personal perspective on what patients can expect in their recovery. Being able to assess their emotions and provide feedback to our pre-op and PACU teams help the patient have a better experience.” “Many of our nurses have close to 40 years of experience each, and they have an extremely large knowledge base since we see patients from newborn to geriatric and from easy procedures to complex surgeries,” added Debra Bennett, RN. “Another great aspect of our team is the varied nursing backgrounds we all hold – surgery, pre- and post-op, labor and delivery, pediatric intensive care, cardiology, gastroenterology, urology, cardiac cath lab, home health and everything in between. Communication between departments is so important!” All members in this department, regardless of which clinical area they came from, surgical or non-surgical, can easily translate their skills into the work they do in preadmit – and they only continue to grow. “As a surgical preadmission nurse, I have used my years of experience as a nurse in surgical services,” said Terri Delatorre, Surgical Preadmission RN at Renown Regional. “I started as a floor nurse with orthopedics for 12 years, and then I worked with the PACU for 11 years. This has helped me give great understanding and care to our surgical patients.” “Because we have staff with such a vast knowledge base, we can rely on our years of working within our organization to help alleviate fears that the patient may have,” added Amy Schler, RN. We can prepare them for what to expect in pre-op and PACU and educate them on what to expect post-op, including any barriers they may face. For example, mastectomy patients may not realize they will not be able to raise their arms for 7-10 days post-op, and total knee patients have to navigate stairs and housing access. Helping patients think about barriers at home that they may not have thought about helps them prepare prior to surgery, enhances their healing and provides a better surgical experience.” The preadmit team works closely with our best-in-class surgeons and anesthesiologists, continuing to grow their expertise along the way while learning alongside our talented providers. For instance, when it comes to our Renown South Meadows preadmit department, anesthesiologist Nariman Rahimzadeh, MD provides excellent guidance for the entire team on state-of-the-art anesthesiology practices. “I am very proud of the work we do with Dr. Rahimzadeh,” said Lisa Closson, Surgical Preadmission RN at Renown South Meadows. “Together, we ensure patients are safe for both surgery and anesthesia.” Despite the challenges that come their way – whether it be changes to process and workflow to navigating support for patients after they leave the surgery floor – the preadmit team cleverly uses their collective wealth of knowledge to bring hope and comfort to all patients. “Our nurses are such warm, caring and compassionate humans that do their best to ease any fears and anxieties patients may have,” said Debra Bennett, RN. The Pride of Preadmission The pride of our preadmit team lies in their ability to make a positive impact on all patients they serve. To them, their work is not just a job – it's a calling. And they do it all while working together to elevate their team and performance. “Our team is most proud of the quality of care we provide to our patients and our abilities to troubleshoot difficult situations to ensure they have a great surgical experience here at Renown,” said Mary Carl, RN. The entire department supports each other by working collaboratively and relying on each other’s expertise to provide the best possible care for patients. They understand that their success as a team depends on their abilities to support and help each other. “Our team is awesome here at South Meadows,” said Jon Capallupo, RN. “We can turn to each other for support, and we all work very well with each other. I am glad to be a part of this team.” “I am proud of how well all of us in preadmit works with each other every day,” added Lisa Closson, RN. “We try to make patients feel comfortable from the moment they arrive to the time they leave the department.” The pride that our preadmit team expends goes beyond their departmental limits – these team members are also trusted teachers. They work closely with cancer nurse navigators to teach weekly classes for patients who have been newly diagnosed with breast cancer, coupled with lymphedema prevention and education classes. The team also encourages participation in Renown’s free smoking cessation programs to help their patients learn the risks and benefits of quitting smoking. When not serving patients or teaching classes, you can find many of these team members taking charge of multidisciplinary committees within our health system, including breast leadership, gastroenterology leadership, shared governance, infection control and recruitment and retention. On top of it all, this team certainly knows how to celebrate, with several of their members being a part of their own department-wide Celebration Committee, where they gather for retirement parties, baby showers and team get-togethers. Always active and never passing up a challenge, our preadmit department are shining examples of Renown’s Culture Commitments, especially Caring and Collaboration, and the pride in the vital work they do every day is limitless. “I am so happy my position in preadmit opened up for me at a time when I was really feeling challenged in my career,” said Nancy Hilts, RN. “The team that we have here is amazing. I am so grateful and thankful every day for the opportunity. It is an amazing place to work!”






.jpg?rev=35bd239de3a2430598e5556fd8dd90ab)



