Search
-
Department Spotlight: Radiation Oncology
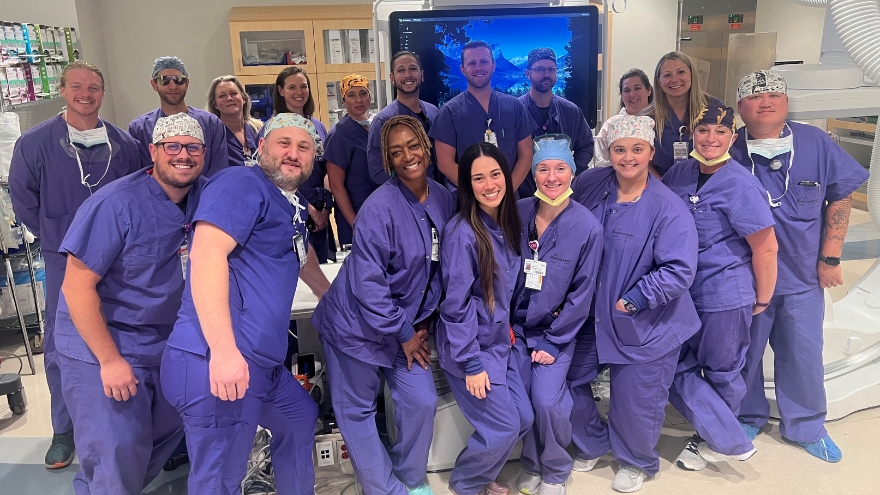
Up to half of all men and one-third of all women will face a cancer diagnosis in their lifetime, according to the Nevada Cancer Coalition. Chances are, you or someone you care about has been affected by cancer and has witnessed the ultimate fight for life. More than likely, your loved one’s cancer journey involved radiation therapy – and in fact, more than half of cancer diagnoses are treated in whole or in part with radiation. At first glance, this treatment plan can sound scary to any person. With a cancer care journey, it takes a village, and at Renown Health, we have top-notch leaders of the village roads that lead to radiation. Meet our Radiation Oncology team at the William N. Pennington Cancer Institute. From intake to inpatient, this department of passionate physicians, radiation therapists, registered nurses, medical assistants, intake coordinators, schedulers and more are here to help every patient dealing with the intimidating diagnosis of cancer. Any patient that needs radiation as a part of their treatment is in the best of hands with this team, who will stop at nothing to ensure each patient under their care knows that they have a village Fighting the Good Fight right alongside them. Teamwork in Tackling Tumors One of the most common forms of cancer treatment, radiation therapy uses high-energy X-rays to minimize cancerous cells. But with Renown’s Radiation Oncology department, the impressive cancer care doesn’t stop there – this team leverages advanced technology right at their fingertips. In fact, our cancer institute has the most state-of-the-art radiation therapy system of its kind – the ultra-precise Varian TrueBeam radiation therapy system – and is the very first program holding American College of Radiology accreditation in the entire region. Given the advanced nature of their jobs and the high standard of care their patients expect them to uphold, it’s no question that the days-in-the-life of each team member is complex and can continually change every day. “There are many moving parts in radiation oncology on any given day,” said Sandra Bailey, Manager of Radiation Oncology Services. “The radiation oncologists consult newly diagnosed patients, follow up with previously treated patients and oversee daily treatments for patients actively receiving treatments. Nurses and medical assistants move around the clinic to support the physicians with patients and provide education and other supportive care.” The physics and dosimetry teams work diligently alongside the physicians to design the most beneficial treatment plan for each patient. Once a patient begins their treatments, the radiation therapists administer the daily treatments with the utmost precision. Intake coordinators, schedulers and patient access representatives make surethe patients have their insurance authorization and are processed through the system appropriately. Like any well-oiled machine, each part is necessary for the other to function at peak performance to ensure our patients receive the quality care they deserve and expect. Like many other clinical departments at Renown, teamwork coupled with education is crucial to best serve radiation therapy patients. Our nurses on this team are experts at exactly that, serving as a reminder of the transformative power of care in the face of a daunting disease. “Radiation oncology is a unique world,” said Kristen Reed, Registered Nurse. “We have many different team members that play a role in how we function as a department. We all work together in some aspect to provide care for our patients. As a nurse, I provide patient education to all my patients before starting treatment to go over potential side effects and expectations on their treatment. Daily, we see new patients and follow-ups, plan simulations to start patients for radiation treatments and provide radiation treatments, among many other daily tasks.” The unique role of our radiation therapists, the team members who are on the frontlines of giving radiation treatments, helps this department stand out from the rest with their tireless dedication to fighting against cancer with compassion and expertise. Not only are they armed with technology, but they are also armed with hands that deliver healing rays of radiation. “As a radiation therapist, our daily tasks can vary pretty widely,” said Casey Johnson, Radiation Therapist. “We rotate between three radiation treatment machines called linear accelerators – one of which we use for stereotactic radiosurgery, a minimally invasive form of surgical intervention. We also staff the CT simulation room where we construct all the patients' treatment devices and perform their ‘mapping’ scan. We then coordinate with the dosimetrists and physicians to determine the specifics of the patients’ course of treatment. The most important parts of our job are patient care and education. Even though our job is very technical and requires tremendous attention to detail, the critical part is remembering that our average workday could be a monumental day for a new patient.” “Our day-in-the-life in Radiation Oncology is centered around patient care,” added Haley Longfield, Radiation Therapist. “Although we do not spend a ton of time with our patients, we see them every day. We are able to build a wonderful rapport with our patients that is top-notch. We set up the room with their treatment devices, get them set up appropriately and administer their radiation treatment. On average, our patients are here for about 15 minutes.” The bottom line: our Radiation Oncology team’s unified commitment to both excellence and innovation promises a brighter future for those battling cancer. No one is ever alone in their fight, and this team makes sure of that, no matter what. Radiating Excellence in Cancer Care The Pennington Cancer Institute boasts a stellar reputation in our community for offering best-in-class, evidence-based care and cutting-edge research, improving outcomes for patients battling cancer. This fact is what inspired many Radiation Oncology team members to take their talents to this department in the first place. “I chose to work at the Cancer Institute because I believe we offer the best patient care experience, along with the most advanced radiation treatments in the area,” said Casey Johnson. "I am a fifth generation Reno resident, and I am part of this community through and through,” added Haley Longfield. “I always knew that I wanted to work here.” The success of our cancer institute starts with our people – and many members of the Radiation Oncology team witnessed this firsthand upon their arrival in this department. “I was initially inspired to move across the country to work in the Cancer Institute by the vision of the senior leaders and the future growth plans for the entire institute; once I arrived, I quickly realized what a great team I am now leading,” said Sandra Bailey. “The compassion and care the Radiation Oncology team provides our patients is second to none. Medical errors are rare in our department, and this can be attributed to not only the processes in place to prevent them, but everyone working together to deliver radiation treatments safely. Each day I witness a patient relationship being nurtured and developed. I am truly honored to be part of this team.” Inspired by Renown's integral role in the northern Nevada community, several team members were drawn to this department because of the opportunity to make a meaningful impact on patients' lives in a quiet healing environment. “As a student nurse, I had clinical and practicum on the cancer nursing unit here at Renown; I noticed the quiet, healing environment and a patient population enduring some of life’s most challenging hurdles,” said Rachel Bales, Registered Nurse. “It is in these moments that you can really make a difference as a nurse. After pursuing critical care as a new grad and working in Interventional Radiology with cancer patients, I knew that I had to find my way back to oncology. I applied to Radiation Oncology, and I am working towards my third year in this department. I have always known that I enjoy helping others, and the fulfillment that comes from working with this patient population is unmatched.” “Renown is a huge part of the community in northern Nevada, and I knew while I was in nursing school that I wanted to have a career here,” added Kristen Reed. “I ended up joining the Cancer Institute about two years ago. My patients are a huge part of why I stay. We really get to know these patients and their families well, especially because they come in from Monday through Friday for up to six weeks for treatments. Building connections and being able to support these patients during a difficult time in their life makes my job fulfilling.” From the initial consultation to the administration of therapy, the staff's commitment to personalized care remains strong. Patients and their families develop profound connections with these team members as they navigate through the challenges of treatment. “We have knowledgeable and caring staff that help guide our patients through treatment,” said Kristen Reed. “This starts on the day of their consultation and continues even after completion of treatment. The patients and families get to know the staff through their treatment, and having a familiar face can be reassuring to them. We also take time every week to see how they are doing physically and mentally while undergoing treatment and we give them a chance to check in with their doctor. Taking this time helps reassure patients and allows them to ask questions, and in turn, reduce some anxiety and worry.”
-
The Expanded Role of OBGYNs in Women's Healthcare
Obstetrician-gynecologists (OBGYNs) see patients from menses (the monthly menstrual cycle that occurs as a part of the female reproductive system), pregnancy and childbirth through menopause and play a pivotal role in managing reproductive health and overall wellness. Dr. James Alexander with Renown Women's Health explains. "As experts in women's health, we are uniquely positioned to recognize subtle changes or symptoms that might indicate broader health issues. This comprehensive approach allows us to serve as a valuable first touchpoint for various health concerns." Preventive Screenings: A Proactive Approach One key aspect is an OBGYN's ability to recommend preventive screenings based on your symptoms, age, lifestyle and medical history. For instance, lipid screenings are critical for monitoring cholesterol levels, which can be a significant factor in women’s heart disease. An OBGYN keeps up with the current guidelines for routine screening as well as in women with risk factors such as high blood pressure, diabetes, or a family history of heart disease during your visit. By identifying risks and abnormal screening early, they can collaborate with you to implement lifestyle changes or treatments to reduce your risk of heart conditions. Schedule Your Screening Appointment Make an Appointment by Phone: 775-982-5000
Read More About The Expanded Role of OBGYNs in Women's Healthcare
-
Understanding the Reasons Behind Heavy Menstrual Cycles
While menstrual cycles can be an annoying inconvenience for many women, heavy bleeding (menorrhagia) is not normal and can disrupt your life. A few days of heavy flow at the start of your period is usually nothing to worry about. However, if you’re frequently experiencing very heavy periods, you should discuss it with your gynecologist or primary care provider. Dr. Megan Fish, an OB-GYN with Renown Women’s Health, discusses various reasons, evaluation and treatment methods when it comes to heavy menstrual cycles. What is classified as heavy menstrual bleeding? The American College of Obstetricians and Gynecologists considers heavy bleeding to be any of the following signs: Bleeding that lasts more than 7 days. Bleeding that soaks through one or more tampons or pads every hour for several hours in a row. Needing to wear more than one pad at a time to control menstrual flow. Needing to change pads or tampons during the night. Menstrual flow with blood clots that are as big as a quarter or larger. What are the most common reasons for heavier periods? A variety of reasons why someone might have heavy periods. Fortunately, most of these problems are treatable. Because each woman's period is unique, only a doctor can definitively determine the cause of your heavy periods. Some of the most common issues that cause heavy periods include: Hormone imbalances such as anovulation, thyroid disease and Polycystic Ovary Syndrome (PCOS). Structural abnormalities in your uterus such as polyps or fibroids. Precancer and cancer such as uterine, cervical, vaginal, ovarian or endometrial hyperplasia. Infections such as chlamydia, gonorrhea, endometritis or vaginitis. Other medical conditions such as liver disease, kidney disease or Pelvic Inflammatory Disease. Medications such as blood thinners and aspirin, hormone replacement therapy, Intrauterine devices (IUDs), birth control pills and injectables. Pregnancy-related problems such as a miscarriage or ectopic pregnancy.
Read More About Understanding the Reasons Behind Heavy Menstrual Cycles
-
Eight Lessons from an MD-PhD Candidate at UNR Med
Meet newly minted Dr. Majid Khan, PhD., a native of Reno, and current MD-PhD candidate and first-generation medical student at the University of Nevada, Reno School of Medicine, who is on his way to a career as a Neurosurgery. While most graduate students often choose between pursuing a medical degree (MD) or a doctorate in philosophy (PhD), Majid has boldly picked both. He is one of three medical students currently in the UNR Med MD-PhD Program run by Dr. Caroline Cobine, PhD and Dr. Violeta Mutafova-Yambolieva, MD, PhD. "Research is not merely an act of sitting at a computer and reading papers – it's about answering the thought-provoking questions about things we come across on a daily basis. By critically evaluating these ideas we can implement solutions to enhance various aspects of the medical field and patient care with an overall goal of improving patient outcomes," Majid said. Majid recognizes that modern research extends beyond academia and holds significant value for hospitals. “Research contributes to improving patient outcomes. By reviewing the data from peer-reviewed research studies, medical professionals can be better prepared to deliver effective care following the most up-to-date guidelines and data,” he said. Majid's journey to pursuing his MD-PhD with a goal of becoming a physician-scientist-surgeon began following a summer in the PathMaker Cancer Research Program at the Huntsman Cancer Institute at the University of Utah. "It was by fate that I stumbled into this field – ever since I saw my first brain surgery, I haven’t been able to look back," Majid said. Here are some of the valuable lessons that Majid has learned along the way. 1. Beyond the 9 to 5, Embrace both 5 to 9s To avoid burnout and nurture personal passions, make your time spent outside of work and school intentional. Harness any free time to reconnect with friends, pursue hobbies and engage with mentors and mentees. 2. Collaboration is Key Work collectively with colleagues locally, nationwide and even worldwide. Cultivate environments to share knowledge and innovation, as well as wisdom, which will evidently lead to more impactful outcomes. 3. Shine a Spotlight on Your Colleagues Acknowledge and celebrate your colleagues in group settings when you notice something outstanding that they’ve said or done – it could anything big or small. Shining the spotlight onto those who are making positive changes within the hospital can inspire a beautiful culture of academic healthcare, which ultimately improves patient outcomes. 4. Redefine Mentorship Mentorship does not need to be confined to traditional frameworks. Seek out guidance in unexpected and untraditional places; sometimes, the most enlightening lessons and opportunities emerge from the most unlikely sources. 5. Diversify Your Experiences Embracing a diverse range of experiences enriches one's medical acumen. You never know when a seemingly unrelated job or experience will help in a scenario in your career. 6. Live By the Mamba Mentality Follow the late Kobe Bryant’s approach to life and work, the Mamba Mentality. This includes planning long-term goals, placing meaning in everything, striving for constant personal growth, following your passions and focusing on the process rather than the end goal. 7. Make Time for Your Loved Ones Don’t forget who helped you get to where you are in your life, specifically your family, friends, teachers and mentors. By making time for the most important and loving people in your life, you will be surrounded by positivity which will help propel you to new heights. 8. Plan your Next Five Moves We all have the ability to come from nothing and become something. Take the time to plan out everything and execute your moves with careful precision. Majid has plans to return to the Biggest Little City after completing Neurological Surgery Residency Program. If you would like to get in touch with Majid, please reach out to him via email at majidk@med.unr.edu.
Read More About Eight Lessons from an MD-PhD Candidate at UNR Med
-
Clinical Research: Advancing Healthcare in Northern Nevada One Study at a Time
Did you know that the Renown Research Office has partnered with the University of Nevada, Reno School of Medicine Clinical Research Office to form the Integrated Clinical Research Office? This means we are able to provide more clinical research opportunities and expertise to our northern Nevada community than ever before. Over the past two years, we have significantly expanded our clinical trial offerings from 35 to 101 studies to meet the healthcare needs of our community members and keep care options local. Currently, we offer clinical research as a care opportunity in areas such as cardiology, pulmonology, endocrinology, oncology, pediatrics, neurology and immunizations. What is Clinical Research? Clinical research is simply medical research that involves human volunteers (participants). Research studies have to be reviewed and approved by ethics committees to ensure that the questions researchers want to answer are appropriate and that research participants are protected throughout the study. Often when we talk about clinical research, we are referring to a clinical trial. Clinical trials are a type of clinical research study that places research participants into groups to study the safety and effectiveness of new medications and devices on a specific health outcome. Clinical trials follow rigorous standards and must pass four phases of testing, where each phase works progressively to understand the correct dosing and effects in larger and more diverse groups of people. Why is Clinical Research Important? Did you know that all medications, diagnostic tests and medical devices prescribed and used today by physicians and health practitioners were once tested in clinical trials? Clinical research advances medical care by helping us understand how to prevent disease and to provide new and better treatments for a wide range of health conditions. At Renown Health, we know the importance of offering the latest opportunities in healthcare, especially when standard of care options have been exhausted. What Are Some Considerations for Participating in Clinical Research? Research volunteers are often drawn to participating in studies because they are interested in accessing the latest health care treatments and/or they want to contribute to scientific discovery. If you are interested in becoming a research volunteer, you should first make sure you fully understand what the study and researcher is asking you to do and consider whether you are comfortable with the study activities and commitments to time and travel such as for required study appointments. Remember, participating in a research study is completely voluntary. That means you choose whether to participate, and you can choose to stop participating in a research study at any time, for any reason. Where Can I Find More Information About Clinical Research? There are many resources you can access if you have questions or want to learn more about clinical research. Your healthcare provider can assist you in your healthcare journey by discussing care options and exploring if participating in a clinical trial may be right for you. The Nevada Division of Public and Behavioral Health recently launched their Clinical Trials Info for Nevadans webpage which provides information on finding clinical trials in Nevada, understanding the importance of diversity in clinical trials, and linked resources to learn more about clinical trials. The U.S. Department of Health and Human Services Office for Human Research Protections provides informational videos, questions to ask researchers prior to participating and information on regulations in place to protect research participants. Finally, at the Renown Research Office, we are always here to support your clinical research journey and can be reached at Renown-CRD@renown.org or 775-982-3646. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
Read More About Clinical Research: Advancing Healthcare in Northern Nevada One Study at a Time
-
Optimizing Mammogram Screenings: A Genetic Approach to a Personalized Screening Schedule
Breast cancer screening has long been a cornerstone of women's healthcare. With 1 in 8 women diagnosed with breast cancer in their lifetime1, the United States Preventive Services Task Force (USPSTF) has developed screening recommendations to help detect early-stage cancer. Notably in 2023, the USPSTF revised the recommended age for biennial mammogram screenings for women with average risk to start at age 40 instead of 502, estimated to result in 19% more lives being saved3 by starting screening earlier. While initiating screening at an earlier age offers advantages to a wide demographic, concerns about the potential of over-screening prompted research into the feasibility of identifying women with lower breast cancer risk who could safely delay mammograms. While guidelines address high-risk individuals, a notable gap exists in providing recommendations tailored to those at lower risk. To gain insight into a patient's risk level, physicians are able to utilize genetic testing to understand an individual's genetic makeup, providing precise insights into their predisposition to various health conditions, including breast cancer. Armed with this genetic information, healthcare providers could craft tailored screening strategies that align with an individual’s specific risk profile. This genetic risk-based approach underscores the value of genetics in individualizing the onset of screening to help avoid over-screening and its associated costs. Surprisingly, genetic information is not currently being widely utilized to identify women at risk of breast cancer or other diseases in clinical practice, despite its potential to make a significant positive impact for patients. A recent retrospective analysis of 25,591 women from the Healthy Nevada Project4 sheds light on the potential benefits of this genetic risk-based approach. The study classified 2,338 (9.1%) of these women as having a low genetic risk for breast cancer. What's remarkable is that these women exhibited a significantly lower and later onset of breast cancer compared to their average or high-risk counterparts. This finding suggests that it might be safe for low-risk women to delay mammogram screening by 5 to 10 years without compromising their health.
-
Celebrating Blood Sugar Balance This Holiday Season
As the holiday season draws near, we find more reasons to celebrate with loved ones. At Renown Health, we are kicking off the celebrations early this November with American Diabetes Month. Approximately 37 million Americans, including 270,000 Nevadans, have been diagnosed with diabetes with as many as 95% of those diagnosed living with type 2 diabetes mellitus (T2DM). What is Type 2 Diabetes? Type 2 diabetes is a chronic health condition that occurs because your body is not using insulin (a hormone made by the pancreas to help cells use the food we eat for energy) as well as it should, resulting in high blood sugar levels. It is important to obtain a diagnosis for T2DM and ensure it is well-controlled to prevent serious health complications. Those with diabetes are at higher risk for blindness, kidney failure, heart disease, stroke and amputation. Tips for Supporting Your Health with Type 2 Diabetes Know Your Blood Sugar Levels: Work with your healthcare provider to establish target blood sugar levels, and make sure to monitor your levels regularly as advised by your healthcare provider to prevent or delay health complications associated with T2DM. Focus on Your Plate: Eating foods such as fruits and vegetables, lean meats or plant-based proteins, healthy fats and whole grains supports diabetes management. If choosing healthy foods is difficult due to your busy schedule, cost or simply because you aren’t sure where to start, talk with your healthcare provider who may refer you to a registered dietitian. Registered dietitian nutritionists are certified nutrition specialists who can provide education and practical tips for eating to support your T2DM diagnosis with visits covered by many insurance plans. Prioritize Staying Active: Engaging in regular exercise is good for everyone, especially those living with T2DM. Exercise helps your cells become more sensitive to insulin and therefore supports healthy blood sugar levels. Always check with your healthcare provider prior to beginning a new exercise plan. Support Stress Reduction: Stress is unavoidable but can be managed through regular exercise, getting enough quality sleep (7-8 uninterrupted hours per night) and practicing meditation and other mindfulness techniques. Plan Ahead for Holiday Gatherings: There’s still room for celebration while focusing on blood sugar management. Consider bringing a healthy dish to your gathering, focus on filling your plate with vegetable sides and eating those first and incorporate a family walk after dinner. If traveling, pack nutritious snacks that support your health and keep you full. Lastly, enjoy the special dishes and desserts this season has to offer in single-serving portions.
Read More About Celebrating Blood Sugar Balance This Holiday Season
-
Department Spotlight: Interventional Radiology
National Radiologic Technology Week is from Nov. 5-11, 2023. Join us in celebrating Renown's Interventional Radiology department!Try to put yourself in the shoes of someone who is told that they have a massive blood clot in their lung, someone who needs a biopsy to determine the next steps of their care, someone facing a stroke or brain aneurysm or someone who needs a catheter to receive treatment such as chemotherapy. You may immediately think that an intense and intimidating surgery is on the horizon. What if, instead of surgery, your care teams were able to use the necessary tools to treat your blockage or administer your medicine with an image-guided procedure? That’s precisely what the Interventional Radiology (IR) team at Renown Health does. Behind the doors of this department is where you’ll find a team of highly skilled individuals who operate like a well-oiled machine, ensuring that each procedure is executed with precision and care. Their commitment to excellence knows no bounds as they provide essential interventions to patients of all ages, from the tiniest newborns to the elderly. Their mission extends beyond diagnostic and therapeutic procedures; they are experts in understanding and serving the ever-evolving needs of their patients. Minimally Invasive, Maximally Impactful With their advanced expertise, our IR teams at both Renown Regional Medical Center and Renown South Meadows Medical Center harness the power of X-ray, CT and ultrasound technologies to navigate their way through life-saving minimally invasive procedures, such as thrombectomies, angioplasties, stent placements, embolizations, catheter and drain insertions and needle biopsies. In the world of medicine, Interventional Radiology often offers an alternative to traditional surgical methods, reducing the risk of hospitalization and helping patients embrace recovery more quickly. Our IR teams have a diverse and busy daily work life in order to make these complex and life-saving interventions happen – and they all have each other’s backs to ensure that every patient gets the care they deserve. “Every day is different, and no two days are alike,” said Ryan Nunes, Specialty Procedure IR Technologist at Renown Regional. “The day can start off first thing in the morning with several emergent cases, such as ruptured brain aneurysms to brain blockages. We all work really well together; we help each other out and come together to do things as a team.” Like every other team at Renown, patient well-being is always a number one priority. The IR department takes this commitment seriously, upholding the highest standards of ethics and safety. “We start the day by preparing rooms and making sure they are well-stocked, checking that all devices are working, performing safety checks and making sure the entire team is well-prepared for whatever cases come through the door,” said Aubrey Goldsmith, Supervisor of Clinical Nursing in IR at Renown Regional. “We have routine cases like drain placements, biopsies, line placements and more, and we also have life-threatening cases that come at a moment’s notice. Our nurses are responsible for monitoring patients throughout the procedure to make sure they are doing well the entire time and are there to respond if the patient has a decline.” "After completing the prior assessment of each patient, we look for any medical problems the patient may have before confirming it is safe for the patient to have procedure done,” said Brandon Hartwig, Interventional Radiology RN at Renown South Meadows. “We work closely with the physicians on all our cases while assessing each patient, going through labs and vitals and personalizing the procedure for each patient.” Even though the procedures they oversee are minimally invasive, the IR team understands that any procedure, regardless of the severity, can be incredibly frightening for any patient. Their best tool for handling patient anxieties? Communication. "The best thing we can do to reduce anxieties and fears in patients is to have communication with them to ensure they know what is going on and what to expect,” said Megan Rios, IR Technologist at Renown Regional. "We set clear expectations for the patients and give reassurance throughout the entire procedure.” "All of our team members are very attentive to our patients when it comes to potential fears and anxieties that they may have,” added Jazmynn Kimsey, IR Technologist at Renown Regional. “We always take the extra time to listen to our patients and break things down, explaining every step before, during and after the procedure.” Knowledge sharing is also a crucial part of the IR process. No patient will ever have to wonder, “what exactly is going on here?” “We provide each patient with education and advocacy throughout the process,” said Blaire Henderson, Interventional Radiology RN at Renown Regional. “We ensure every patient is as comfortable as possible at all times.” “When it comes to procedures, patients tend to be scared and nervous,” added Ryan Nunes. “The silver lining to what we do is that it is all done through very small openings of the skin, and we all explain this to patients. Most procedures we do are done under moderate sedation which helps put the patient more at ease.” In a world where advanced medical care meets the human touch, the IR team exemplifies Renown’s commitment to making a genuine difference in the health and well-being of everyone they serve.
Read More About Department Spotlight: Interventional Radiology
-
6 Healthcare Action Items for the LGBTQIA+ Community
Every patient, regardless of how they may identify, greatly benefits from preventive healthcare and early detection. Members of the LGBTQIA+ community face unique considerations when it comes to their health, and a proactive approach to preventive screenings and vaccines is important in order to address their individual health needs. Dr. Karen Thiele, Family Medicine Physician with University Health and Assistant Professor of Family and Community Medicine at the University of Nevada, Reno School of Medicine, breaks down key steps that LGBTQIA+ patients should take to safeguard their health. PrEP and PEP Pre-exposure prophylaxis (PrEP) is a strategy to prevent human immunodeficiency virus (HIV) infection. It is an important measure for those who are HIV-negative but may be at risk of contracting it. The highest risk sexual practice is receptive anal intercourse, due to the relative fragility of rectal tissue. This medication can stop HIV from spreading in the body and help patients maintain their HIV-negative status. PrEP is available in both pill form, which is taken every day, and injection form, of which the first two injections are initiated one month after another while all other injections are initiated every two months. Post-exposure prophylaxis (PEP) is an antiretroviral drug regimen taken after potential HIV exposure to prevent an HIV-negative individual from converting to HIV-positive status. PEP is only for emergency situations and must be started within 72 hours of exposure – sooner is always better than later – and must be taken for 28 days. PrEP and PEP are available in many ways, including visiting your primary care provider (PCP) or an urgent care location. HPV Immunization All genders and identities can protect themselves against human papillomavirus (HPV), a sexually transmitted infection (STI) that can lead to the risk of cervical, mouth, head, neck, throat, anal, vaginal, penile and vulvar cancers. HPV is so common that nearly all sexually active people, regardless of sexual orientation and practices, will be exposed at some point in their lifetime. The HPV vaccine (common brands include Gardasil and Cervarix) is a safe and effective method to prevent HPV, according to the Centers for Disease Control and Prevention (CDC). This vaccine protects against infections that can lead to HPV-related cancers and precancers, as well as genital warts. While patients should start receiving the vaccine at 9 years old years old, unvaccinated adults up to the age of 45 can also receive the vaccine through their PCP – better late than never! STI Testing Sexually-transmitted infections form from bacteria, viruses or parasites that can be transmitted by person-to-person sexual contact through semen, vaginal, blood and other bodily fluids. According to the U.S. Department of Health and Human Services, there are more than 20 million estimated new STI cases across the nation each year. Luckily, most STIs are preventable. Annual STI testing for HIV, gonorrhea, chlamydia and syphilis is important to stay on top of your sexual health. Because these STIs may sometimes have no symptoms, screening is recommended regularly and with any change in sexual partners. Depending on the specific condition, tests for these infections include urine, swab and blood tests. Speak with your primary care provider on a screening schedule that works best for you. Prostate Exams Prostate exams look for early signs of prostate cancer in patients who still have a prostate. The CDC recommends those who are at least 55 years old get regular prostate screenings; however, for patients with a family history of prostate cancer, screenings may be recommended as early as 45 years old. These exams are done via two common methods – a prostate specific antigen (PSA) blood test and a digital rectal examination (DRE). Your provider can help you determine your risk and when you should start getting screened. Pap Tests and Pelvic Exams Patients of all genders who have a cervix, uterus, vagina and/or ovaries will benefit from regular pelvic exams and Pap screenings. A pelvic exam consists of a provider looking inside the vagina and at the cervix for anything unusual. A Pap test, also known as a Pap smear, involves your provider using a small, soft swab to collect cervical cells to check for early signs of cancer. Generally speaking, people with these organs should have a Pap test every three years starting at age 21 through the age of 30. After age 30, patients should receive a Pap test with HPV co-testing every five years until age 65. These recommendations are changing based on new research, so it is important to have a conversation with your PCP about the current guidelines so you can make an informed choice about what schedule you should follow. A gynecologist or your primary care provider can counsel you and perform these screenings. Mammograms and Breast Exams People with breast tissue, especially dense breast tissue, are at risk for breast cancer, and regular breast screenings are your best line of defense. At-home breast self-exams are the first step – you will want to check your breasts for any lumps, changes, fluid leaks, irregular tissue thickening or anything else that feels unusual. The Breast Cancer Risk Assessment tool, provided by the National Cancer Institute, is a good place to start to identify your risk. Talk with your primary care provider about the risks and benefits of starting screening at age 40 so you can make an informed decision about when to start. If you have any family history of breast or ovarian cancer, your PCP will offer you genetic testing for BRCA 1 and 2 mutations. Nevadans over the age of 18 can also get BRCA genetic test for free by enrolling in the Healthy Nevada Project. Mammograms are important screening tools, but for a significant portion of people with breast tissue, density of the breast tissue may make mammograms less helpful in detecting cancer. Your primary care provider can help you decide what additional imaging (such as breast ultrasound) might be best for you.
Read More About 6 Healthcare Action Items for the LGBTQIA+ Community
-
Sepsis: Causes & Symptoms
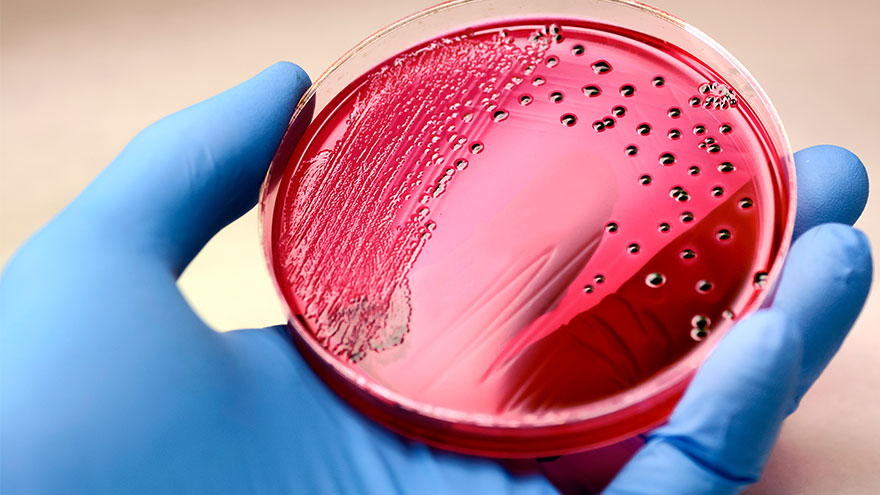
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.
-
Department Spotlight: Respiratory Care
This Department Spotlight is dedicated to Jason Simpson, Manager of Respiratory Services at Renown Children’s Hospital. Take a moment to breathe deeply. Inhale in, exhale out. We rely on our lungs to provide us with the air we need to live a healthy life – and this essential bodily function is something that many of us don’t think twice about since it comes easily for us. Now, imagine yourself as someone who is living with severe asthma, chronic obstructive pulmonary disease (COPD) or someone who was recently diagnosed with a frightening respiratory condition like COVID-19 or pneumonia. The simple act of breathing can prove to be an intimidating venture requiring the care of a professional. Who are the people that take on the challenge? Meet Renown Health’s Respiratory Care Services department. Serving patients across 13 service lines, three acute facilities, outpatient locations and telehealth, our respiratory specialists – including respiratory therapists, respiratory care aides, inpatient COPD respiratory therapy navigators and educators and more – use their expertise to help restore the vitality of all their patients with every inhale and exhale, shaping a healthier livelihood one lung at a time. The Guardians of Respiratory Wellness Whether they are managing lifelong respiratory conditions or offering crucial support in emergencies, the Respiratory Care team strives to enhance the quality of life for every patient. As an indispensable member of the clinical team at Renown, our respiratory therapists work collaboratively with doctors and nurses to tackle a wide range of tasks, tailoring care for each patient’s unique needs. “Respiratory care is involved with all stages of life, from beginning to end,” said Sarah Kurtz, Respiratory Therapist. “We work closely with nurses and doctors and perform arterial punctures, breathing treatments, weaning maneuvers for patients on life support, intubations and much more. We assess patients constantly to see if their care needs to be upgraded or if they can be weaned to get them back home with their families.” “You start your morning researching your assigned patients,” added Tim Start, Respiratory Specialist. “We go over lab values and chest radiographs and decide the best plan of care for each patient. Our objective is to improve their respiratory status by giving them medications and doing breathing exercises. We participate in other forms of care with nurses, such as activities of daily living (ADLs) and mobilization. We work as a team, and that enables us to provide great patient care.” For patients living with COPD, enjoying all that life has to offer comes with a separate set of obstacles. According to the Centers for Disease Control and Prevention (CDC), over 200,000 people across the Silver State are living with this chronic condition. Luckily for them, Renown has a specialized team to help these patients optimize their life and manage their condition with individualized treatment and education. “We run a report every morning to identify all the patients currently admitted who have a history of COPD, take respiratory medications or smoke,” said Amber Beck, Inpatient COPD RT Navigator. “After looking through their charts, we visit with the patient (and possibly their family) at the bedside to help them better understand how to manage their breathing issues.” As a vital part of the Respiratory Care team, Renown’s respiratory care aides help ensure the seamless operation of our respiratory care services. These dedicated professionals provide essential support to respiratory therapists not only during intricate procedures but also outside of face-to-face patient care by transporting equipment, restocking supplies, assisting in the mobilization of patients and more. “We are responsible for the maintenance of unit supplies and making decisions regarding levels of stock to be maintained,” said Dia Ramos, Respiratory Care Aide. “We also transport equipment, refill the oxygen tanks on the floors and intensive care units (ICUs), order and stock respiratory care supplies, mobilize patients and assist the respiratory therapists during bronchoscopies in the ICUs. In addition, we clean respiratory equipment like mechanical ventilators, continuous positive airway pressure (CPAP) and bilateral positive airway pressure (BiPAP) machines, high flows and aerosol poles.” Once the COVID-19 pandemic hit, a special spotlight shined upon respiratory care teams across the country for the heroic care they provided patients in respiratory distress. While their roles in health systems have gained a better understanding nationwide, this team understands it is vital for them to educate the community about the important jobs they hold for our patients. “Respiratory care can be under the radar,” said Pam Umek, Respiratory Specialist. “Once, when I told someone that I am a Respiratory Therapist, they said, ‘Oh, like a yoga breathing instructor?’ I then explained all the things we do: intubation, extubation, bronchoscopies, transports, traumas, codes, rapid responses, pediatrics/NICU, breathing medications/therapies, open heart rapid ventilator weaning … needless to say, that individual walked away with a better understanding of not just Respiratory Care Services but also the enormous effort it takes to care for our community.” The accolades and achievements continue to pour in, from national awards and certifications to implementing different jobs in care units to optimize the patient care experience. “We have earned and continue to maintain the Joint Commission Disease-Specific Certification for COPD,” said Amber Beck. “We are well below national averages for 30-day readmissions, lengths of stay and mortality due to COPD. Sandy, one of our COPD Coordinators, was a recipient of a patient advocacy award from the American Association of Respiratory Care and FACES Foundation.” “We have started implementing Respiratory Care Aides in the critical units, starting with the Cardiac ICU,” added Dia Ramos. “We work as one team and are always helping each other with their tasks.” Education and mentorship are at the core of Renown’s mission to make a genuine difference in the health and well-being of every patient. Nurturing the next generation of medical professionals – including respiratory care professionals – is a task that the Respiratory Care team takes seriously. “It has been great being able to help educate students in different disciplines,” added Pam Umek. “We have been able to offer shadow shifts to students in emergency medical services (EMS), nursing and medical school. These opportunities help students entering the medical field have a better understanding of the many ways we can help care for our respiratory patients.” From the moment of birth to the final stages of life, Renown is fortunate to have a Respiratory Care team that tirelessly ensures every breath counts, safeguarding their role as a trusted partner within our health system. A Tribute to Jason Simpson, Healthcare Hero
-
Managing Your Uncontrolled High Blood Pressure
Renown Health, the region's leading cardiology care provider, is offering a clinical trial for eligible patients struggling to control their high blood pressure. Nearly half of adults (119.9 million) in the United States have hypertension, or blood pressure that is higher than normal. Hypertension can put you at risk of other life-threatening disease, such as a heart attack or stroke. There are methods that cardiologists use to manage high blood pressure, but only 1 in 4 adults with hypertension (27.0 million) have their blood pressure under control.* Some patients with high blood pressure experience resistant hypertension, which does not respond well to multiple antihypertensive medications given at the same time. This means that there are many important opportunities for healthcare professionals to explore new ways to treat hypertension. At Renown Health, we lead the region in cardiology care with our technological expertise and patient-centered approach. That is why our cardiology team is partnering with the Renown Research Office to offer the RADIANCE Continued Access Protocol (RADIENCE CAP) clinical trial to eligible patients. RADIANCE CAP is a non-randomized study designed to allow for continued access to ultrasound renal denervation therapy via the Paradise System, and to allow for the on-going collection of safety and effectiveness data in patients with uncontrolled hypertension despite the prescription of antihypertensive medications. The body’s complex communication system between the brain, heart and kidneys can sometimes become overactive, increasing your blood pressure through messages in the nervous system. Renal denervation is a minimally-invasive procedure which reduces activity from the nerves in your kidneys to lower blood pressure. This is the third in a series of renal denervation clinical trials Renown Health has offered to patients with resistant hypertension over the last several years, with over 40 local participants. “All the participants that I have had the pleasure to work with on these studies are very excited and grateful to have this option for helping control their blood pressure” states Lisa English, Lead Clinical Research Coordinator for Cardiology studies at Renown Health. “I love getting to know each one of them and helping on their healthcare journey. We have an amazing team of providers and staff at Renown that go out of their way to make patients experiences positive and the studies successful.” Dr. Michael Bloch, Cardiologist and Principal Investigator for the RADIANCE CAP study at Renown Health’s Institute for Heart and Vascular Health adds, “Despite lifestyle modifications like diet and exercise and the widespread availability of effective and well-tolerated medications, approximately 50% of all people with hypertension have inadequate blood pressure control putting them at risk for stroke, heart failure and kidney disease. As a one-time durable procedure, renal denervation with the Paradise endovascular system from ReCor Medical, Inc. may help millions of patients improve their blood pressure control without necessarily needing to increase their medications.” Our teams of expert providers and researchers are here to support you on your healthcare journey. Talk to your provider about the RADIANCE CAP clinical trial at your next appointment to see if participation may be right for you.
Read More About Managing Your Uncontrolled High Blood Pressure