Search
-
Research Shows Genetic Approaches to Breast Cancer Screenings Yield More Accurate Results
Clinical researchers with the Healthy Nevada Project co-author research paper with findings that emphasize the need for a comprehensive approach to breast cancer risk assessment – including a focus on genetic medicine – to help ensure that individuals at high risk are identified and supported proactively rather than reactively. Breast cancer is a leading cause of cancer death among women in the United States. According to the American Cancer Society, about 1 in 8 women will develop breast cancer and about 1 in 39 women will die from breast cancer. Breast cancer is associated with increased age, hereditary factors, obesity, and alcohol use. Since 1990, breast cancer death rates have declined progressively due to advancements in treatment and detection. In Nevada there are an estimated 2,310 new breast cancer cases a year, and genetic mutations such as in the genes BRCA1 or BRCA2 remain a top risk factor for this prevalent disease. Recognizing the urgency for progress in breast cancer research, a collaborative effort between physicians, advanced practice providers and scientists from the Healthy Nevada Project® (HNP) and Helix have unveiled groundbreaking research. This study explores how genetic screenings are a necessary supplement to traditional testing methods, together offering more accurate insights into a patient's likelihood of developing breast cancer in the future. HNP is operated by Renown Genomic Medicine and the Institute for Health Innovation and is one of the largest community-based population health studies in the country. Their team works in collaboration with Helix, a leader in precision health that delivers comprehensive genomic solutions. Together, this dynamic partnership aims to understand breast cancer risk factors and pave the way for more effective preventative measures. The combined research team studied 25,591 female HNP participants to evaluate the performance of different genetic screening approaches to identify women at high risk of breast cancer. The results of this research suggest that a combined monogenic, or single-gene, and polygenic, or multi-gene, approach to breast cancer screenings helped produce more accurate results and more closely identify study participants who have a high genetic risk of developing the disease. "Based on this research, we are advocating a shift in approach which would improve breast cancer risk assessment through a combination of effective family history ascertainment and genetic screening,” said Joseph Grzymski, PhD, principal investigator of the Healthy Nevada Project, research professor at the University of Nevada, Reno School of Medicine and co-author of the breast cancer research paper. “This tailored approach, founded on the assessment of individual genetic risk, not only intends to elevate patient well-being but also will improve efficiency and equity in healthcare." Complementing the team’s research on leveraging genetics to identify women at low genetic risk of breast cancer that could safely defer mammogram screenings by five to 10 years that was released in late 2023 in JAMA Oncology, the study suggests that incorporating genetic information can assist in personalizing breast cancer screenings and optimizing the use of screening resources. "Existing disparities persist across various facets of breast cancer screening and treatment; however, genetic screening is clearly a powerful tool to help facilitate early intervention for those at higher risk,” said Jamie Schnell Blitstein, APRN, a primary care nurse practitioner at Renown Health and co-author of the breast cancer research paper. “By placing a heightened focus on risk, we underscore the pivotal role of preventative breast cancer screening.” Despite the availability of effective methods for early screening, co-authors of this research found that 78 percent of women with a family history of breast cancer had their risk ascertained only after a breast cancer diagnosis. The findings emphasize the need for a comprehensive approach to breast cancer risk assessment – including a focus on genetic medicine – to help ensure that individuals at high risk are identified and supported proactively rather than reactively. “These findings that can profoundly impact how healthcare is delivered were only made possible by all the participants who were willing to consent to research,” said Alex Bolze, PhD from Helix and co-author of the publication. “Broad-scale collaboration projects like these between Renown Health and UNR that engage large populations where participants share both their genetic information as well as electronic health records drive advancements in preventative medicine, as well as fundamental biological research.” The research paper was officially accepted on Jan. 29, 2024, and will be published by Elsevier, Inc. on behalf of the American College of Medical Genetics and Genomics. The contents of the paper will appear in the international journal Genetics in Medicine Open. Read the full article by visiting sciencedirect.com. The Healthy Nevada Project is currently recruiting new study participants. Free to all Nevadans with a saliva sample or blood draw, participants and their referring providers receive access to whole-exome sequencing and clinical grade results that help provide insight into their unique genetic risks tied to heart disease and certain cancers. If you are interested in enrolling in the study, schedule a Virtual Consent Appointment through MyChart or contact the Renown Institute for Health Innovation at RenownIHI@renown.org or (775) 982-6914 to be connected to a Genomic Representative. About Renown Health Renown Health is the region’s largest, not-for-profit integrated healthcare network serving Nevada, Lake Tahoe and northeast California. With a diverse workforce of more than 7,000 employees, Renown has fostered a longstanding culture of excellence, determination and innovation. The organization comprises a trauma center, two acute care hospitals, a children’s hospital, a rehabilitation hospital, a medical group and urgent care network, and the region’s largest, locally owned not-for-profit insurance company, Hometown Health. Renown is currently enrolling participants in the largest community-based genetic population health study, the Healthy Nevada Project®. To join the Renown Health team, visit renown.org/careers. About Helix Helix is the leading population genomics and viral surveillance company operating at the intersection of clinical care, research, and data analytics. Helix enables health systems, life sciences companies, payers, and government partners to accelerate the integration of genomic data into patient care and public health decision-making. Learn more at helix.com.
-
Breast Surgical Oncology
Breast Surgery Care at Renown Health Renown Breast Surgery Care, located within the Center for Advanced Medicine B, is a comprehensive, fully integrated breast surgery clinic, addressing a wide spectrum of breast problems ranging from benign to cancerous: Benign breast conditions such as fibroadenoma, phyllodes tumors, and nipple discharge Breast cancer risk assessment and genetics High risk breast lesions such as atypical ductal hyperplasia, atypical lobular hyperplasia, LCIS, papillary lesions, and radial scars Advanced breast cancer surgical techniques including oncoplastic surgery for best aesthetic outcomes possible and nipple sparing mastectomies, working closely with skilled plastic reconstructive surgeons. Our highly experienced breast surgical oncologists are continuing to expand our team to better meet the evolving needs of our community and beyond. We are excited to soon be incorporating an oncology wellness team who can further support our patients with focused nutritional guidance, functional assessments for prehabilitation needs prior to surgery or medical treatments, and guidance for development of physical activity and other exercise programs, for best outcomes in cancer treatment as well as future risk reduction. The National Accreditation Program for Breast Centers (NAPBC) is a rigorous process designed to ensure high quality care for breast centers by meeting thoughtfully created standards that are constantly being reviewed and updated for ongoing improvement of patient care. We are the only NAPBC-accredited program in Northern Nevada.
-
Ladies! Get Screened for Breast Cancer
Early detection is a significant piece of the breast cancer puzzle. Susan Cox, Renown Health Director of Cancer Operations, discusses what you need to watch for and how the latest technology can help detect potential cancer sooner. When should women start getting breast exams? It depends on risk factors: Average-risk women: Most medical organizations recommend the first mammogram between 40 and 44. Higher-risk women: Dependent on their high risk, which will dictate when they start screening, but generally around the age of 30 and not before 25 years old.
-
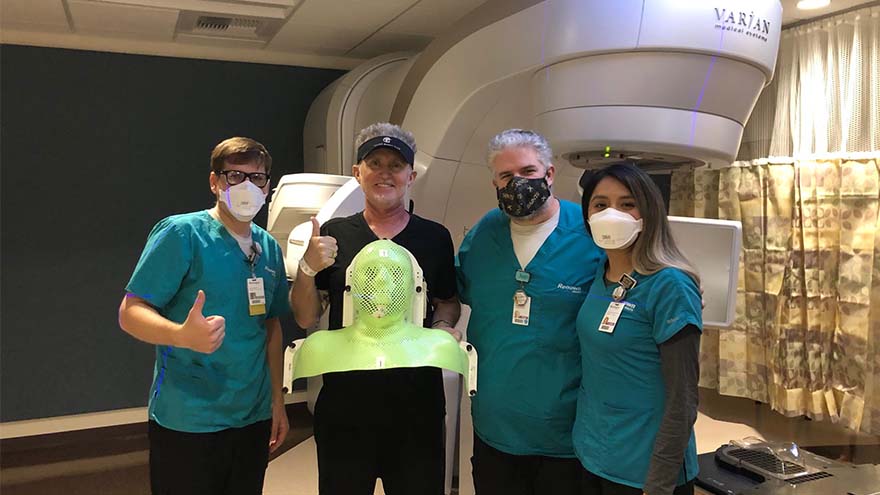
A Cancer Diagnosis and a Move to Reno
Michael Millman was all set to move to Reno from the Bay Area when he noticed a pimple-like growth on his forehead, and he decided to get biopsied "just in case." It was July 2020, less than six months into the COVID-19 pandemic, when Michael got the call that the biopsy came back cancerous. He was in shock. Still living in the Bay Area at the time, he immediately scheduled to have the basal cell carcinoma removed in August. After the removal, he thought he was in the clear, but a few months later, Michael noticed that his lymph nodes felt weird, and he even cut himself shaving because of some persistent swelling in the area. Given his recent history of skin cancer, Michael immediately scheduled an appointment with a specialist in the Bay Area. "I met with an ear, nose and throat doctor who suggested a fine needle biopsy of my lymph nodes, tongue and an MRI, both with and without contrast," Michael said. "I remember feeling dreadful and that I couldn't believe this was happening yet again." A Hard Decision Michael's squamous cell carcinoma, determined by the pathology report to be significantly influenced by the HPV virus, had metastasized to his lymph nodes on both sides of his neck, and his doctor said it could be stage four cancer. He remembers feeling like he was in quicksand, unsure if he should follow through with his move to Reno, or stay in the Bay Area for treatment. By now, it was early December 2020, and hospitals in the Bay Area and across the world were at limited capacity due to COVID-19. But, in what Michael describes as a positive twist of fate, the San Francisco ear, nose and throat provider he had seen about his biopsy results mentioned that he knew many providers in the oncology department at Renown, including Abhinand Peddada, MD. The San Francisco provider called Dr. Peddada's office with a referral, and Michael even remembers that Renown called him to hear more about his diagnosis before he even got the chance to call them "To be honest, I was feeling shut out in the Bay Area, and Dr. Peddada said he could help me expedite the treatment process," Michael said. "I finally felt a sense of relief." And so began Michael's 7-week chemoradiation cancer treatment program at Renown.
-
8 Important Health Screenings for Men
Men are generally less likely to visit their doctor for exams, screenings, and consults compared to women. To address this, we've collaborated with Dr. Bonnie Ferrara of Renown Health, to compile a list of eight essential screenings that can help men maintain their health. 1. Blood Pressure Tests Ages 20+ Blood Pressure tests measure the pressure in your arteries as your heart pumps. Biennial (every two years) checks are recommended if you have normal blood pressure or more frequently if you have high blood pressure (hypertension) or low blood pressure (hypotension). The United States Preventative Services Taskforce cites normal blood pressure below 120 systolic (top number) and 80 diastolic (bottom number). 2. Cholesterol Screening Ages 20+ High levels of cholesterol increase your risk of stroke and heart disease. A simple blood test will help your healthcare provider determine your numbers and if you're at risk. If you have a family history of diabetes or heart disease, you may need yearly screenings. But, again, your doctor can provide the best course of action.
-
Lung Cancer Screening and Early Detection
Lung cancer is the leading cause of cancer deaths in both men and women in the U.S. The good news is the five-year survival rate increases dramatically if lung cancer is treated before spreading to other parts of the body. Julie Locken, MD, of Renown Health Imaging, explains more. What are the signs and symptoms of lung cancer? As you might expect, most lung cancer symptoms appear in the chest and can affect your breathing. Watch for signs such as: Persistent cough Constant chest pain Shortness of breath Wheezing Bloody or rust-colored phlegm Hoarseness Swelling of the neck Pain or weakness in the shoulder, arm or hand Recurring pneumonia, bronchitis or other lung infections Loss of appetite and loss of weight can also be signs of lung cancer That said, there are usually no symptoms in the early stages of lung cancer, which means getting screened can truly be a lifesaver. If you have a history of smoking, you should get screened as a precaution. What are the risk factors of lung cancer? Around 80% of lung cancer cases stem from a history of smoking tobacco. But there are other known causes, such as secondhand smoke, radon, asbestos and diesel exhaust. It’s important to do what you can to eliminate exposure to all of these to reduce your lung cancer risk. People with an immediate relative – a parent, sibling or child – diagnosed with lung cancer and people between 50 and 80 years old are also at higher risk and may need to consider screening. People who are at the highest risk are those with a history of smoking tobacco, particularly smokers who averaged one pack of cigarettes per day for 20 years or more, as well as former heavy smokers who quit in the last 15 years.
-
How Regular Cervical Cancer Screenings Can Save Lives
According to the American Cancer Society, approximately 13,820 new cases of invasive cervical cancer will be diagnosed, and 4,360 women will die from cervical cancer. However, cervical cancer is preventable with regular screening tests and the HPV vaccine. It’s important to note that medical advances have allowed progress in diagnosing and treating cervical cancer. While it used to be one of the most common causes of cancer death for American women, the incidence of death has significantly declined. What to Know About the HPV Vaccine HPV vaccination is the best way to prevent cervical cancer and is recommended for all youth starting as early as age 9, or for teens and adults up to age 45 who didn’t start or finish the series. In Nevada, only 50.1% of teens ages 13-17 have been vaccinated for HPV. There are 13 types of HPV, and the vaccine Gardasil 9 protects against 9 of those HPV strains, greatly reducing the incidence of cervical cancer among vaccinated individuals. What to Know About Cervical Cancer Screenings The CDC says the most important thing you can do to help prevent cervical cancer is to have regular screening tests starting at age 21. And there are two common tests that can detect early stages of cervical cancer (or precancer) and improve health outcomes. The pap test (or pap smear). This screening looks for precancers. Women should begin getting pap smears when they’re 21. The human papillomavirus (HPV) test looks for the virus that can cause these cell changes. Cervical Cancer Screening Schedule The American Cancer Society offers the following guidelines for screenings: All women should begin cervical cancer screening at 21. Women between 21 and 29 should have a pap test every three years. Beginning at 30, the preferred way to screen is with a pap test combined with an HPV test every five years. This is called co-testing and should continue until age 65. A pap test (or pap smear) is performed during a regular screening appointment to look for precancers, cell changes on the cervix that might become cervical cancer if they are not evaluated or appropriately treated. Typically outpatient procedures can reduce the risk of long-term health impacts that prevent pre-cancerous cells from becoming cancer cells. Women over 65 who have had regular screenings in the previous ten years should stop cervical cancer screening as long as they haven’t had any severe precancers found in the last 20 years. How to Get Screened Request an appointment with your primary care physician or OBGYN to schedule a screening.
Read More About How Regular Cervical Cancer Screenings Can Save Lives
-
Celebrating Resilience: Raquel's Remarkable Journey Through Breast Cancer Treatment
Raquel was 33 when she was diagnosed with breast cancer. It was April 2023, when she found a lump in her breast and was referred to the William N. Pennington Cancer Institute. After comprehensive imaging, she was diagnosed with invasive lobular carcinoma, which is a type of breast cancer that begins in the milk-producing glands of the breast. Between June 2023 and January 2024, she received a total mastectomy, chemotherapy and radiation at Renown Health. “Breast cancer is uncommon in women under 40, but any woman with a mass or lump in her breast should have an exam by a physician and imaging at any age,” said Dr. Lee Schwartzberg. In fact, according to the Centers for Disease Control and Prevention (CDC), only 9% of all new cases of breast cancer in the U.S. are found in women younger than 45. “It was a pretty scary diagnosis, but I’ve been led by great people through the process,” she said. “They were so helpful and there for me throughout the chemo and radiation.” Raquel's journey through breast cancer treatment at the William N. Pennington Cancer Institute was marked by the exceptional care provided by the Renown Health team, including nurses, nurse navigators, therapists, support teams and providers. Among the dedicated professionals, Dr. Michelle Chu and Dr. Lee Schwartzberg played pivotal roles in Raquel's diagnosis and subsequent treatment plan. Their expertise, compassion and commitment to patient care left an indelible impact on Raquel's experience. Their thorough examination and comprehensive approach ensured that Racquel received the best possible care for her invasive lobular carcinoma. In addition to the care provided at Renown, Raquel greatly benefitted from being connected with a mentor by Dr. Chu. This mentor, Kayla, had undergone a similar diagnosis and treatment plan, and at the same age Raquel. They texted and called each other throughout Raquel’s treatment, providing additional support through a challenging time. As of January 2024, Raquel is done with her treatment and continues to see her care team for follow-up appointments. “I’m through the worst and ready to rebuild my life,” Raquel said. To help celebrate this milestone, Nevada Athletics invited Raquel to receive the game ball at a Nevada Men’s Basketball game. She was joined on the basketball court for this special recognition by her husband, Raul; mother, Arlene; and two daughters, Ryleigh and Rhiannon. Racquel's journey is not only a testament to her resilience but also a tribute to the invaluable contributions of Dr. Chu and Dr. Schwartzberg in guiding her towards triumph over breast cancer.
Read More About Celebrating Resilience: Raquel's Remarkable Journey Through Breast Cancer Treatment
-
3D vs Whole Breast Ultrasound Which is Right for You
Breast cancer is the leading cause of cancer deaths in women in the U.S. That’s why early detection is so important. Dr. George Krakora, a radiologist with Renown Institute for Cancer, explains what to watch for and how new technology can lead to early detection. Most women know the importance of breast health and staying current with annual breast exams, but may not know that both screening guidelines and technology is evolving. So we asked George Krakora, MD, a radiologist for the Renown Institute for Cancer, what every woman should know about breast cancer detection and which screening method is right for them. First off, when should women start getting breast exams? Generally, women should start getting breast exams using mammography or ultrasound after they turn 40 years old. But we also want women ages 18 to 39 to talk to their primary care provider and ask for what’s called a formal risk assessment to see if screening is needed sooner. And you want to make sure your care provider is giving you a breast exam starting at age 25. It’s also a good idea to be familiar with how your breasts look and feel so you can report any changes to your care provider. What are the risk factors for breast cancer? Are there any preventive steps women can take? There a few risk factors you can’t control, like your age, family history of breast or other cancers, and if you have dense breast tissue. Your risk for breast cancer increases as you get older, and most breast cancers are diagnosed after age 50. Knowing your family history is important because a history of cancer and shared lifestyle can raise your risk. Your breast density can also increase your risk: Women with high breast density are four-to-five times more likely to get breast cancer than women with low breast density. But the good news is there are quite a few things you can do to prevent breast cancer, like not smoking, watching your alcohol intake, and maintaining a healthy weight with good diet and exercise. There are a lot of newer screenings out today. What is the difference between 2-D and 3-D mammography? In a 2-D mammogram, the tech takes X-rays of the breast. These pictures can show the radiologist if there are any lumps or tumors you might not be able to feel. In 3-D mammography, the process is largely the same but more X-rays are taken and it takes a few seconds longer for each image. This kind of exam detects 41 percent more cancers and reduces the number of false-positive results given to patients. This improvement in technology is great for both patients and their care providers. 3-D mammography provides better images of the breast, which allow doctors to more clearly diagnose and avoid false positives, especially in women with dense breast tissue. And what about a whole breast ultrasound. What is that? A whole breast ultrasound uses sound waves to detect cancerous tumors in the breast without using any radiation — it’s an ultrasound just like pregnant women get to check up on their baby. And the exam only takes about 20 minutes. We recommend these exams for patients whose mammograms have shown that they have dense breast tissue. Dense breast tissue can make it harder for doctors to see any abnormalities, lumps or tumors in a mammogram, so this technology ensures better early detection.
Read More About 3D vs Whole Breast Ultrasound Which is Right for You