Search
Results for 'nurses'
Clear-
Department Spotlight: Labor & Delivery
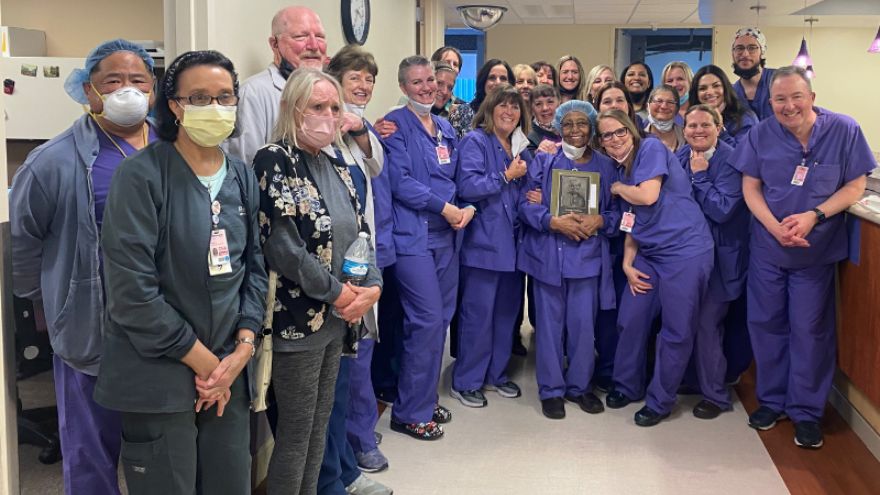
Parents welcoming their new bundles of joy into the world might be overcome with emotions. They're exhausted yet excited to meet their new baby and hold them in their arms. That’s where Renown Health’s Labor & Delivery (L&D) department comes in. When patients arrive at the L&D unit in Renown Regional Medical Center, they are embraced with caring, compassionate nurses, surgical technicians and physicians ready to serve their family. As they get ready for the big moment in their private L&D room or family suite, you can be certain that you, they can be certain that they will receive the excellent care they deserve. Unpredictable, but Never Unprepared Ushering in new life can bring a lot of surprises for parents, but the L&D department is prepared for any challenge. Whether the unit is helping with a routine or high-risk delivery, every patient and newborn are treated with personalized care that is uniquely tailored to their own individual needs and birth preferences, from labor evaluation and birth to post-birth lactation consultation and navigating the nursery. “Our floor is never predictable,” said Bri Goode, Renown L&D nurse. “Our nurses and our staff work as a team to ensure the best care for our patients. I commonly say that we are all 'nurses’ for each patient!” The state-of-the-art technology at their fingertips – including advanced 3D ultrasound machines – coupled with the love and passion the team has for their patients allows them to create an optimal environment for every mother and baby. The unit is also equipped with a Labor Assessment Area, where expectant mothers are evaluated to determine what stage of labor they are in, removing the guesswork and allowing providers to treat the patient and unborn child more efficiently and meet them exactly where they are at in the labor process. Nothing can replace the careful guidance and words of encouragement a patient needs in the delivery room. The L&D department are true patient advocates and firmly believe in the power of listening and the power of staying calm and collected. “To help our patients and ease their fears and anxieties, we always ensure them that our biggest goal is to have a healthy mom and healthy baby,” said Lindsay Strowmatt, Renown L&D nurse. “We constantly reinforce that they are strong and capable. Empowerment goes a long way!” “We always take the time to actually sit down and listen to the patient, no matter how busy we are,” added Krystie Mortensen, Renown L&D nurse and DAISY Award winner. “It’s important for us to understand where their nerves are stemming from and address any changes in plan of care along the way.” While the L&D unit is seen as a “happy place,” as described repeatedly by the members of the team, a seemingly low-risk patient can also turn into an emergency in a matter of seconds. "Our line of work can involve high-stakes emergency care,” said April Tucker, Renown L&D nurse. “We view change as a necessary part of growth, and we save lives.” These steps result in high patient outcome scores, which can be attributed directly to the unit. “We have continually great outcomes from hard work and consistency in care,” said Roya Galata, Renown L&D nurse and Nursing Organizations Alliance (NOA) Lifetime Achievement awardee. “I have tremendous love for my patients and the type of work I do.” Awards Without End With patient safety and experience always top of mind, and with the team continually going above and beyond for all parents and their newborns, it’s no wonder why the L&D department has achieved a long and growing list of both local and national awards and accolades. This year, U.S. News & World Report ranked the L&D unit at Renown Regional as "High Performing in Maternity Care – Uncomplicated Pregnancy.” This award is only the latest in this department’s “Best Of” accolades list, as the unit also achieved a win as the Best Place to Have a Baby in the 2022 Best of Reno Awards. Not only is the department continually recognized, but individual team members also receive coveted awards within their professional associations. As previously mentioned, Krystie Mortensen is a DAISY Award winner, which means that she has been recognized for the “super-human work” she has done throughout her career. Additionally, three team members, including Roya Galata, have received NOA awards, celebrating their contributions to the nursing profession as a whole. Many nurses in this department also choose to pursue lifelong learning by taking advantage of the educational benefits that Renown offers. Several team members have completed their continuing education in midwifery and advanced practice, reaffirming their dedication to delivering healthy babies and helping parents manage their first few days with their newborns. “The teamwork on this unit is phenomenal, and the energy and commitment that the staff comes in with every single day amazes me,” said Lora Carlson, Renown L&D Manager of Nursing. Internally, the L&D department loves to show their spirit at Renown. In December, they received the Best Holiday Decoration award during the 2021 holiday season. The team also enjoys participating (and scoring well) in Renown-sponsored Halloween costume contests. In 2023, the L&D department will only pursue greater heights to continue producing patient outcomes. A Work Family “I stay here because this is my family. My work family.” These strong words were proudly stated by Jeanne Bufkin, Renown L&D Surgical Technician, and echoed by virtually every L&D employee. Having each other’s backs during both times of need and times of celebration is a must in this department, and they do so proudly. “Our staff constantly back each other up,” added Lora Carlson. “They display a lot of adaptability and flexibility. That’s why our unit functions as well as it does.” Several team members in this department experienced the care of the L&D unit at Renown before they became fully-fledged employees. “I had two of my babies here and had wonderful experiences both times,” said Judy McBride, Unit Clerk. “I love being a part of the reason why the next woman can say the same!” Bri Goode also delivered her child at Renown and loved her experience so much that she was also inspired to join the team. “I chose to work at Renown because when I had such a positive experience during my delivery while I was in nursing school, I knew it was a team I wanted to be a part of.” Coming to Renown was clearly an easy decision for this team; staying at Renown is even easier. “I stay here because I love what I do and who I do it with,” said Judy McBride. “I truly feel like I am treated as an asset to this department, and it makes me want to come to work every day and make a difference in these mothers’ lives.” The closeness of this department and the top-of-the-line collaboration displayed by every provider can be felt by the patients during their entire stay at Renown. “We have an amazing collaborative team of physicians, nurses, scrub techs, unit clerks, patient access representatives and environmental services personnel that strive to provide our patients with the best possible care,” said April Tucker. The labor and delivery process is a team effort – and those interested in jumping in on this team effort are welcome to join. Delivering healthy babies and supporting new mothers are cornerstone acts in meeting Renown’s mission of making a genuine difference in the communities we serve. Our L&D department does precisely this and more, never giving up in Fighting the Good Fight.
-
Department Spotlight: NICU Transport
Bringing in new life is an exciting and beautiful occasion. The possibilities for the newest members of our world are endless – what will the child grow up to become? What will they achieve in their lifetime? Anyone will agree that a new life is precious and protecting that life by any means possible is a necessity. Sometimes, however, a baby’s journey into our world brings along obstacles. Prematurity, congenital defects and other complications can accompany a birth and the baby’s first few moments of life. But what happens when these complications happen outside of a fully-functioning Labor & Delivery unit, or if the complications need a special level of intervention with a health system capable of caring for their unique needs? Enter the NICU Transport team at Renown Health. As the only Neonatal Intensive Care Unit (NICU) Transport team in northern Nevada, these dedicated nurses, respiratory therapists and neonatal nurse practitioners – who have normal unit duties of their own at Renown Regional Medical Center – step up to the plate to take on this extra duty to support members of their community facing some of the scariest moments of their lives. To them, transporting babies in critical condition and giving them the best chance of life isn’t just a responsibility; it’s a calling. The NICU on Wheels When the Saint Mary’s maternity unit, which was Renown’s partner in NICU transport duties, made the decision to close, our dedicated NICU nurses and respiratory therapists diligently rose to the occasion to fill the demand. Dubbed the “NICU on Wheels,” Renown’s team went from taking on transport duties every other day to 365 days a year – and they are always ready to go at a moment’s notice, whether it’s by ambulance or by fixed-wing aircraft. “When we learned about the closure we knew it was our calling and knew we had to step up,” said Rachel D., Neonatal Transport RN at Renown. “We still have regular days on the floor, and we each switch off being on-call for transport. Once we get a distress call, we have 30 minutes to get to the hospital, grab our gear and go. We have to essentially put a whole room’s worth of portable equipment in one bag.” “I really enjoy being a part of the transport team and making a difference from northern Nevada to northern California,” added Sam V., Supervisor of Respiratory Care at Renown. “We are able to practice at the top of our skill level and use autonomy that not every practitioner gets to use.” Each NICU Transport unit works in teams of three when heading out into the field: one nurse (our bedside experts), one nurse practitioner (our education experts) and one respiratory therapist (our lung and breathing experts). With several years – and in many cases, decades – of experience in NICU nursing, NICU transport duties and respiratory therapy, this team is poised to provide state-of-the-art lifesaving care en route to the hospital. This diverse array of experiences among the team especially comes in handy as they continue to face the increased transport workload. “We are so thankful to have Saint Mary’s employees come over and work on our team after their maternity ward closed,” said Melyssa H., RN, NICU Transport Coordinator at Renown. “Helping the babies, as well as helping the scared families, will always be our top priority.” “I love the complexity that babies provide in the NICU,” added Jennifer J., Neonatal Transport RN at Renown. “Providing hands-on care right at the bedside along other members of the team is such a rewarding experience.” Education is also a crucial tool in NICU care, especially in the field. The nurse practitioners on this team make it their mission to outreach to the community, including our rural health partners, and help them build the tools and skills they need to care for our smallest and most critical patients. “I have been on a few transports where we went out and did not have to bring the baby over to the hospital, and we were able to provide lots of education instead,” said Shiela A., Respiratory Specialist at Renown. “For instance, I was called out to Fallon for a baby that was in respiratory distress. When we arrived, we saw the baby was awake and active although intubated. The tube came out, and we retaped it. While we stayed to observe the baby to make sure everything was okay, the nurse practitioner on the team provided educational tools to the family on what they can improve on regarding their baby’s tubing. Our nurses do such a great job with these teachings.” “When I started, I quickly noticed that more education was needed in the field,” added Jennifer J., RN. “Now I see the momentum we’ve had in these communities really take full force. Because of this education, and the confidence we instill in our patients’ families, each baby’s transition to our team has become so much easier. It has been awesome to watch this progress over the years.” With immense experience, education and a strong commitment to their community under their wing, the NICU on Wheels is only just getting started. Teamwork Makes the Dream Work Running a successful NICU Transport operation, especially as the sole health system participating, takes a village. With only three professionals out in the field, the team leans on their fellow nurses, physicians, surgeons and specialists to make the operation run as smoothly as possible. From REMSA and Care Flight helping load patients in and get them to the hospital safely, to Renown’s Clinical Engineering team who are first on the scene when machines need repairs and troubleshooting, everyone rises to the occasion to achieve the best-possible outcome for our youngest patients at some of the most challenging moments of the beginning of their lives – and they are fully trusted to move those mountains. “Being a part of the NICU Transport team has given us the opportunity to facilitate a deeper, meaningful relationship with providers and a patient’s entire care team,” said Rachel D., RN. “They entrust us with our assessment skills, opinions and skill levels. There is an equal layer of trust between us and them.” Despite the pressure they feel every day, the NICU Transport team never let it overtake them and instead let it empower them. “We are under a lot of pressure and stress regardless of the case, and yet, we all work so well together; the teamwork really is incredible,” said Lisa A., Respiratory Specialist at Renown. “I am very proud of how our team steps up and is very intricate, even down to organization. For example, team members like Shiela arrange all the respiratory bags and make sure they are laid out in a way that makes the procedure as simple as possible to ensure there are no complications.” The nurses and respiratory therapists also partner together on the NICU floor and are always ready to provide coverage when their transport colleagues get a call. Committed to collaboration and ready to jump into action, the NICU Transport team works together to elevate each other and the bottom line for each patient. “This is a full-time gig, and the group works together to make sure everyone is covered; we are all very collaborative,” said Sarah K., Respiratory Specialist at Renown. “We all think of our patients as extra special, and it’s nice to know that you can make a difference in the baby’s life and the lives of the family. We all have a sense of purpose in giving back to the community.” “I am just so thankful to be a part of this team,” added Marcia A., Neonatal Transport RN at Renown. “We really have developed a strong bond.” A Track Record of Success The life-saving measures that each member of the NICU Transport team take surpass hospital walls. The impact they have on each baby are remembered and celebrated for years, and they often develop lifelong relationships with patients and their families after their stay in the NICU. One prime example of this can be found in an impassioned letter from Tess, the mother of a young boy who was in the midst of respiratory distress and needed immediate intervention. Because of the valiant efforts of Renown’s NICU Transport team, her child, Warren, is a healthy and happy baby to this day. She recalls the experience: Warren had stopped breathing while getting routine blood work. He was resuscitated twice while at an area hospital. We made the decision to transfer him to Renown for him to be admitted into the NICU. Within an hour and a half of this decision, Renown had sent a team consisting of a respiratory therapist, nurse and nurse practitioner to come and get him. As soon as the team entered the room, we immediately felt safe and comforted. The team made sure we knew exactly what was going on and what was going to happen in the following hours, and they let us know they would do everything for Warren. He was resuscitated two more times by the respiratory therapist while getting ready for transport. At that time, the decision was made to intubate for a smoother ride to Renown. We knew you all had his best interest in mind, and of course, we trusted you with everything. The intubation went well, and he was packed up and ready to drive. Today, Warren is hitting all of his developmental milestones and is a normal, happy baby in everyone’s eyes. We can’t thank the NICU Transport team enough for taking such good care of Warren and helping him Fight the Good Fight. “This success wasn’t just due to our three-person unit – our manager, Jason, also jumped in and drove all the way to Carson City to stabilize the child,” said Shiela A. “This just goes to show that no matter our title, we are always here to help and make a huge difference in the lives of our patients.” Success stories of children like Warren describe the common mission of the NICU Transport team in detail, and while there are more of these stories to come, the team is always ready to make the necessary sacrifices for the greater good of their patients. “Sarah K. is like Warren’s guardian angel,” said Tess. “We call her ‘Auntie Sarah’ now. He wouldn’t be here if it weren’t for her and the entire NICU Transport team. It takes a special kind of person to work in the NICU. I can never repay this team for what they’ve done for Warren and our family.” “I am proud of this team, their flexibility and the sacrifices they have made to do transport 365 days a year,” added Melyssa H., RN.” The remarkable success of the NICU Transport team serves as proof of the unwavering and tireless commitment of each and every team member, bringing hope to families during their most difficult moments. “NICU Transport forces you to be confident in yourself and your abilities and to push yourself a step further,” said Rachel D., RN. “I am a better nurse because I joined the transport team.”
-
Department Spotlight: Children’s Infusion Services
Help us celebrate the holiday season by sharing joy with our Children’s Infusion Services team! Thinking about blood can make any of us squeamish, and seeing it can be even more intimidating to the children in our lives. Being treated for a condition that requires blood transfusions or chemotherapy infusions is no easy feat, especially during the holiday season. This time of year, we are proud that we can offer our pediatric patients the power of proximity and excellence by having access to high level care close to home. The Children’s Infusion Services (CIS) department at Renown Children’s Hospital is committed to bringing the gift of quality care to our community’s youngest patients. Whether they are caring for a child with a blood disorder or giving expert infusion care for a child battling cancer, no team does what they do better than these expert nurses, medical assistants, intake coordinators and physicians. ‘Tis the Season to Bring Hope As the only pediatric oncology and hematology program in the region, the CIS department has a lot of responsibility on their shoulders. From inpatient chemotherapy to outpatient infusion services, this team treats a long list of pediatric blood conditions including: Pediatric cancers Anemias Immune-mediated blood disorders Sickle-cell disease Bone marrow failure syndromes Bleeding disorders “Our team provides a large variety of services from labs draws, sedations for procedures, infusions for diagnoses such as Crohn's disease, blood transfusions, as well as chemotherapy,” said Jen Torres, RN. “Our team works extremely well together. We try to go above and beyond for our patients every day. It may be something as simple as a hug to comfort a parent or a special birthday gift for a patient.” “My job allows me to work with several departments and providers when coordinating care for our littlest of patients,” added Jane Strawn, Intake Coordinator. “I assure proper authorizations are in place for the care that is needed, I communicate with our families when scheduling appointments, I organize End of Treatment Celebrations, as well as birthday shout outs and work closely with our Child Life team to help make the challenging appointment little easier.” To best serve their patients, the team thrives on being expert multitaskers. Central line care, chemotherapy administration, blood transfusions, medication management, preventative injections, lab draws, lumbar punctures, biopsies, imaging – you name it, they do it. And they do it all with the utmost focus on safety and support. “Our days have a lot of variation, as we perform a number of different services,” said Meagan Bertotti, RN. “We provide infusions for patients with chronic or acute medical conditions and chemotherapy/biotherapy treatment to patients undergoing cancer treatments. Overall, though, we work as a team to make these difficult procedures and treatments as easy as possible for the patients and families by providing engagement and support.” “While we handle a lot of chemotherapy treatments for pediatric patients, we also do other infusions and transfusions as well such as blood and platelet transfusions, enzyme replacement therapies, different types of injections such as Rabies vaccine or Synagis for high-risk babies who need that extra protection during the RSV season, and lab draws,” said Chelsea Angues, RN. “We care for patients that get their therapies from outside hospitals, but the patient lives within the Reno area. We receive orders from those outside hospitals to care for those patients, so they can still be with their families and not have to travel.” As members of the Children’s Oncology Group, a highly-regarded clinical trials group where over 90% of pediatric cancer patients across the U.S. receive treatment, teams like CIS in Renown Children’s Hospital deliver the highest standard of care. This partnership is a true testament to the devoted collaboration and relationship-building this team commits to on behalf of their patients every day. "One of the biggest accomplishments of our team is the fact that we became a member of the Children’s Oncology Group, and the Children's Infusion Center and Pediatric Oncology became one unit,” said Shelby Nolte. "Instead of being a clinic on one side and an infusion center on the other, we really came together to make it a whole unit that collaborates on almost everything.” “We've put much time into trying to understand other departments, their flow, their rationales and their processes so we can come to a solution that benefits our patients the greatest,” added Tiffany Macie, RN. “We've taken the last few years to really build our relationships with our pharmacy staff, our lab staff and our central supply resources. Our relationship building extends beyond the walls of the Renown building as well and out to the community providers too. In the past few years, we've been able to build relationships with the providers in the community where they trust they can send us their patients for treatment and lab draws. Finally, we've spent much time working on the relationships as a team. It's emotional work we do on our unit, and these families become our family. It's important to us that we take the time to be together outside of our shifts to enjoy one another and laugh!” In the compassionate realm of pediatric healthcare, CIS knows that the complexities of a cancer or blood disorder diagnosis can take an emotional toll on their patients and families. The team firmly believes that emotional support can be as important as the physical and medical support throughout each patient’s unique care journey, striving to be a comforting presence during daunting times. “The most important part of my day is collaborating with the Children's Infusion team to make life manageable for the families that are going through this experience,” added Shelby Nolte, Senior Medical Assistant. “We work as a team to make life easier for the blow of a cancer diagnosis. We are there for our families in every way. If they need a shoulder to cry on, an ear to listen or just someone to play cards with or tell a funny story too, we are there.” “One of the things our team does extremely well to help our patients and their families with new diagnoses is to simply meet them where they are,” said Tiffany Macie. “That looks different for every family and every patient. We work in an environment where can build relationships with our patients and their families. This allows us the unique opportunity to really get to know them. We learn their fears, their joys, their worries, what their family lives are like, and we learn how to best meet them where they are.” Transcending the conventional boundaries of care, the CIS department closely supports each patient, offering them solace tailored to the unique fabric of each family's life.
Read More About Department Spotlight: Children’s Infusion Services
-
Breast Feeding Doesn't Have To Mean Sore Nipples
If you think sore nipples are just a normal part of breastfeeding, think again. Robin Hollen, APRN, and Breastfeeding Medicine Specialist, says that nursing can be an enjoyable experience for mom and baby without pain and discomfort. A top concern of nursing moms within the first week after delivery is how to prevent sore nipples. Even moms who’ve nursed before struggle with this common issue. While many women think it is a regular part of the nursing experience, it is actually a sign that something isn’t quite right. “Nursing your baby should be enjoyable,” says Robin Hollen, Breastfeeding Medicine Specialist with Renown Health. For over 30 years Robin has been supporting moms to breastfeed. Below she shares some valuable information and tips, helping you create a happy and healthy breastfeeding experience for you and your baby. What causes sore nipples? The most common cause of sore nipples involves incorrect latching. For a proper latch, a baby’s mouth takes in the entire nipple and some of the breast, so that the nipple rests at the back of the mouth where the palate is soft. With an improper latch, the mouth may slip down to the tip of the nipple while the baby nurses. This constant pressure on your sensitive skin may cause discomfort and pain. A board-certified lactation consultant can help assess if your baby is latched correctly and troubleshoot your breastfeeding concerns. Less common causes of sore nipples include: • Improper tongue placement of baby • Clenching • Incorrect breast pump use How can a mother prevent sore nipples from an improper latch? Breastfeeding is a learning experience for both mom and baby. Ask for help with the latch so your baby learns it correctly and maintains its depth. In the past, new mothers were surrounded by a community of women — their own mothers, grandmothers, or other family and friends — to provide assistance and guidance with every latch at the beginning of an infant’s life. In today’s culture, new moms can find themselves on their own with no extended family to lend their knowledge. Nurses, pediatricians and lactation consultants now fill that role; they are the eyes and hands along with the much-needed experience to guide new mothers. Our Breastfeeding Medicine experts assist nursing moms with latch every day. Even a single visit with a lactation consultant observing your breastfeeding baby can provide valuable insight on achieving, and maintaining, the proper latch - preventing future nipple soreness and discomfort. How to heal sore nipples from breastfeeding To heal sore nipples, you must first fix the cause, and correcting the latch prevents further damage. A lactation consultant can also help you address the pain. Below are some breast healing tips: • Your own expressed breast milk is excellent to rub into the nipple for anti-bacterial protection. • For those moms who need more lubricant or fat than breast milk offers, use a lanolin or a cream that is labeled safe for the baby. • Soothies are a gel pads providing comfort in between feedings, but should not be used with lanolin products. • Breast shells, not to be confused with shields, can guard the nipples from irritation or pressure in between feedings. If you have more questions about preventing and healing sore nipples or general breastfeeding concerns, talk to your pediatrician or a Renown Health Breastfeeding Medicine specialist at 775-982-6365.
Read More About Breast Feeding Doesn't Have To Mean Sore Nipples
-
Remove the Guesswork with Renown’s Labor Assessment Area
Pictured above: A section of Renown’s Labor Assessment Area. When patients expecting a new child are about to give birth, nerves can be especially heightened. Questions flood their minds: Is the baby actually on the way? What’s going to happen next? Are we ready to push? Lucky for them, at Renown Health, the guesswork can finally end with Renown’s Labor & Delivery unit Labor Assessment Area. This unique space is a triage area that helps make more precise labor diagnoses by determining exactly what stage expectant parents are at in the labor process. Funded by a state grant more than a decade ago, the six-bed Labor Assessment Area sees 500-600 patients per month – from patients entering the unit directly, unsure if they are in active labor, to patients who are sent over from elsewhere experiencing labor symptoms, such as high blood pressure and water breaking. The area also serves as a pre-operation space for patients getting ready for procedures such as C-sections. The six cubicles that are enclosed with doors and curtains ensure each patient gets the private, one-on-one care they need. Furthermore, rather than sitting in a waiting room, this area allows expectant parents a comfortable place to prepare for labor. “We are a unit that prides ourselves on getting patients into beds very quickly,” said Debbie Hawley, Associate Nurse Manager in Renown’s Labor & Delivery unit. “This area has allowed us to triage more effectively and allow more patients to collaborate with their provider in a quick manner.”
Read More About Remove the Guesswork with Renown’s Labor Assessment Area
-
How to Safely Store Breast Milk
Breast milk. It's often referred to as liquid gold. And fortunately, it can be safely refrigerated or frozen for later use, which can allow you to be a bit more flexible in your new routine with baby. Whether you're getting ready to return to work, planning for the chance date night out or just exclusively pumping, it's crucial to understand the guidelines for proper breast milk storage. Storing Breast Milk Use clean bottles with screw caps, hard plastic cups that have tight caps or nursing bags (pre-sterilized bags meant for breast milk). Be sure to label each container with the date the milk was pumped and your baby's name if the milk is going to childcare providers. You can add fresh, cooled milk to milk that is already frozen, but add no more than is already in the container. For example, if you have two ounces of frozen milk, then you can add up to two more ounces of cooled milk. For healthy full-term infants, milk can be stored as follows: Room temperature - six to eight hours (no warmer than 77°F, or 25°C). Refrigerator - up to five days at 32°-39°F (0°-3.9°C). Freezer– Varies depending on freezer type. Up to two weeks in a freezer compartment located within the refrigerator. Three to six months in a freezer that is self-contained (standard kitchen fridge/freezer combination) and kept at 0°F (-18°C). Breast milk should be stored in the back of the freezer and not in the door. Six to 12 months in a deep freezer that is kept at -4°F (-20°C). Be sure to leave about an inch of space at the top of the container or bottle to allow for expansion of the milk when it freezes. Thawing Breast Milk Place frozen breast milk in the refrigerator to thaw (about 24 hours) then warm by running warm water over the bag or bottle of milk and use it within the next 24 hours. If you need it immediately, remove it from the freezer and run warm water over it until it's at room temperature. Never microwave breast milk and do not refreeze it. Once your baby has started to drink from the bottle, you should use it within one hour. You may find that different resources provide different recommendations about the amount of time you can store breast milk at room temperature, in the refrigerator and in the freezer. Talk to your doctor or lactation consultant if you have any concerns or questions.
-
Bye-Bye Holidays, Hello Routines! Getting Kids Back into the Groove
The kids are back in school and the holidays are all but a distant memory: Now what? Karen Wagner, APRN, offers specific tips about getting kids back to their routines in the post-holiday-hustle-and-bustle. Are you finding the kids struggling with bedtime routines? Having trouble getting them to tackle homework? There’s a simple reason: The holidays messed with their mojo! Here, we talk with Nurse Practitioner Karen Wagner about what to do to get them back on the straight and narrow. Why Routines Are Important “Holidays are a fantastic time to get together with family and friends, so our routines are usually off — and this is understandable, “Wagner says. “While the holidays are exciting, they are chaotic and can put our kids out of the routines.” So how do you get kids back into those routines they crave? “Consistency/routines are crucial for our kids,” she says. “Most people — kids and adults — experience a let-down feeling after the holidays, and post-holiday adjustment takes time.” So what can we do, specifically? Wagner recommends the following: Re-establish family routines, including before- and after-school programs or child care routines. Once kids are back on the regular schedule, they’ll find that sense of familiarity as the old routine returns. But keep in mind, this won’t happen overnight. Encourage healthy eating, as the upheaval of their schedule can be offset by a balanced diet. Make sleep time a priority: Keep in mind that it might take up to three nights of strict bedtime to get them back on track. But enforcing normal bedtime will get their bodies back on a normal schedule. Return to usual chores and expectations. Nothing encourages a return to routine like reminding them of the basics. Incorporate indoor and outdoor time. They likely spent lots of time outdoors during our unseasonably warm winter break — and they even had a snow day or two! So encouraging both indoor and outdoor time will help them return to a circadian rhythm and tire them out from exposure to fresh air. “It is never too early to encourage a love for physical activity in kids by exposing them to fun fitness activities and sports,” Wagner says. “Physical activity improves bone health, cardiorespiratory and muscular fitness, decreases levels of body fat, reduces symptoms of depression, and improves cognitive skills and the ability to concentrate.”
Read More About Bye-Bye Holidays, Hello Routines! Getting Kids Back into the Groove
-
Top Safe Sleep Tips for Your Baby
Becoming a parent for the first time means lots of new unknowns – from learning to breastfeed and swaddle to buckling your newborn into the car seat for the first time. But when it comes to putting them to bed safely, it’s important to remember it really can mean life or death. It’s something we’re taught before our little one is even here: the correct way to put your baby to bed safely. Sadly though, the number of infant deaths continues to climb. The main culprit of sleep-related infant death continues to be all the items parents leave in the crib with their babies. According to the Center for Disease Control and Prevention, there are about 3,500 sleep-related deaths among babies each year. “The best advice is ‘bare is best.’ Keep your infant’s sleep space clutter free – no blankets, bumpers, toys or pillows,” said Karen Wagner, Pediatric Nurse Practitioner. Follow the ABCs for Safe Sleep Remembering the ABCs is an easy way to remember how to put your little one to bed safely. A: Alone No blankets, toys or pillows. “We do recommend using a sleep sack as a blanket alternative,” said Karen. “It prevents the risk of suffocation and keeps your baby warm.” Keep in mind, the greatest risk for suffocation happens when babies are under 1 year of age, so it’s best to save the toys, blankets and pillows for their “big kid bed,” or around 18 months old. B: Back The slogan “back is best” is another good reminder. Keeping your baby on their back until they’re old enough to rollover helps reduce the risk of Sudden Infant Death Syndrome (SIDS). C: Crib It is best to have your baby sleep alone in their crib. While co-sleeping may be enticing, especially after a late-night feed, it increases the risks of possible suffocation. However, “having your child in your room, in their own crib or bassinet, is protective for SIDS,” Karen said. “In fact, we think co-rooming reduces SIDS risk by almost 50 percent.” Co-rooming allows parents to keep new babies in close reach and helps parents oversee their baby’s sleep, just in case something happens.
-
Children's ER, Urgent Care or Wait it Out? Here's Your Guide
We’ve all been there: Your child gets sick right after urgent care closes — or worse, in the middle of the night. So do you wait it out, or do you load up and head to the Children’s ER? Pediatric Emergency Physician Joey Gassen, MD, with Northern Nevada Emergency Physicians, has insight. As parents, we often wish we had all the answers. And while a short-and-sweet comprehensive parenting guide is elusive, we can help if your questions involve whether to go to the children’s ER or wait it out. Here, a pediatric emergency physician explains when you should take your child to the Children’s ER at Renown Children’s Hospital, and what makes a children’s ER different. How do you know when it’s time to take your child to the ER? Having a sick or injured child is stressful. If you have a true emergency, you should go straight to the ER or call 911. When to go to the ER: Allergic reactions Asthma or severe shortness of breath Fever (infants less than two months old) Choking or poisoning Coughing up or vomiting blood Fainting, confusion or seizures Fractures or broken bones Head injuries Severe bleeding If you determine your child’s condition isn’t life-threatening but needs to be taken care of right away, urgent care is the best choice. Those conditions include: Cold and flu Coughs and sore throat Fevers Vomiting, diarrhea, stomach pain Cuts and severe scrapes Minor injuries and burns What is different about Renown Children’s ER compared to the adult ER? The difference starts when you first bring your child in. We have a lobby dedicated to our community’s smallest patients. The 24/7 lobby incorporates a child-friendly atmosphere with vibrant colors to help decrease anxiety that can accompany emergency situations. Our children’s ER also has equipment sized just for kids of any age. We offer a distraction machine, as well as games and movies, to help children cope with what can be a traumatic experience, like getting an IV. In addition, we have Child Life Specialists available to provide the emotional support to both children and their families. Why is it important to have an emergency room and lobby open 24/7 dedicated to children? Children aren’t just little people. They have special needs that require specialized care. Our children’s ER is staffed with skilled physicians and pediatric nurses certified in advanced pediatric emergency care to give your child the highest level of support. Renown Children’s Hospital From newborns to teens, Renown Children’s Hospital offers many different services and treatments designed specifically to take care of our community’s children. We provide a range of specialized services — from a dedicated Children’s ER and Pediatric ICU to a children’s imaging center and child’s asthma program. Explore Children’s Services
Read More About Children's ER, Urgent Care or Wait it Out? Here's Your Guide
-
A Day in the Life of a Child Life Specialist
March is Child Life Month, meaning this is the perfect time to ask: What exactly does a Child Life Specialist do? To find out, we “virtually” tagged along with one for a day. This is what a typical day looks like in this important role. For Child Life Specialist Brittany Best, play is a natural part of her work day. She approaches her role with a keen understanding of how the seemingly small tasks she performs every day — comforting children prior to a procedure, writing thank-you notes to donors, training interns — positively impact the lives of the children she serves and their families. So what does it take to work in Renown’s Child Life Program? Best shares some of the highlights from a “typical” shift. A Child Life Specialist’s Day 7:30 a.m. Clock in, put my belongings in my office, and print the patient census information. This helps me to get a sense of the day ahead, as I’m covering three areas today. 8-9 a.m. I look over the census sheets for all three areas and check in with the nurses in each area and then try to prioritize my day. 9:00 a.m. I attend Interdisciplinary Rounds for the Pediatric Intensive Care Unit, where the most critically ill or injured children are treated. Additionally, Interdisciplinary Rounds enable several key members of a patient’s care team to come together and offer expertise in patient care. 10:00 a.m. I come up to the specialty clinic/infusion center to check on the patients that have arrived already and see how things have been going since I had last seen them. We see patients frequently up here, as they are receiving treatment for cancer or other disease processes. 10:55 a.m. I’m notified by an RN that a patient needs an IV started, so I go meet with the patient and their family. I meet with a 6-year-old and mother to explain what an IV is and why it is needed. We go through an IV prep kit, looking at all the different items the nurse will use including cold stinky soap, a tight rubber band and also a flexible straw. I also teach this patient a breathing exercise to help them relax during the procedure with a simple exercise known as “smell flowers, blow out candles.” I demonstrate how to take a deep breath in through the nose — like smelling flowers — then how to blow that breath out — like blowing out birthday candles. 11:10 a.m. I walk with the patient and mom to the procedure room on the Children’s Patient Floor for an IV procedure. The Vecta distraction station is set up and running with its bright lights and water tube that bubbles with plastic fish swimming. The parent holds the patient in their lap, and with the distraction and medical preparation, we are successful! I give the patient a toy and provide emotional support to both the young patient and his mom. It’s easy to forget that these procedures can be stressful for the parents as well. 11:30 a.m. I finish rounding with staff to catch up on patients. In addition, I introduce myself to patients and put my contact number on the board in each room so the families know how to get a hold of me should they need anything. With support from volunteers, we distribute movies, games, and “All About Me” forms to patients and their families. These forms help us get to know our patients with things like their favorite foods and televisions shows. 12:45 p.m. I help with a lab draw in Children’s Specialty Care. A 3-year-old patient is very anxious about the “shot,” so I meet with the patient and parents to discuss coping techniques. The patient holds the Buzzy Bee and does well during the lab draw. The mom is relieved, and the patient is excited for a toy. The Buzzy Bee actually helps block the transmission of sharp pain on contact through icy numbing and also tingly vibration. 1 p.m. Joan, an artist with our Healing Arts Program, arrives on the Children’s Patient Floor to perform art therapy with patients. She helps two young patients who are interested in watercolor paintings. 1:15 p.m. Time for lunch and also a trip to Starbucks. 1:45 p.m. I finishing rounding and introducing myself and our services to the patients I have not met yet. 3 p.m. At this time, I meet with the parents of a newly diagnosed diabetic patient who is in intensive care. A new chronic diagnosis is always difficult, so I am there to provide emotional support. It’s instances like this that remind me every day why I love the work I do. 3:30 p.m. I meet with a new volunteer, discuss their role and also give the new volunteer a tour of the units. We are very thankful for all our volunteers on the floor, as their contributions help us provide a variety of basic services to a larger number of children. This also allows the Child Life Specialist to devote time to children who require more intense or specialized service. 4-5 p.m. I finish charting on patients and help two newly admitted families before I start to wrap up for the day. This evening we have a volunteer covering the times during shift change, which is helpful as it makes for a smooth transition for families during the meal time and change of shift. During this time, I write a note for this volunteer indicating the patients I want her to focus on. 5-5:30 p.m. Check in with critical patients and families before leaving for the day. All-in-all, it was a good day.
Read More About A Day in the Life of a Child Life Specialist
-
Pregnancy & Childbirth
Choosing Renown Women's Health is the first step to a healthy pregnancy. Our exceptional family-centered care with complete prenatal services is designed for the health and well-being of you and your baby. Board-certified primary obstetricians (OBs) coordinate pregnancy care and develop personal relationships with every mom-to-be, understanding birth choices and preferences. Labor & Delivery: 775-982-5759 Our specialties include: Managing high-risk pregnancies including twins, multiples, multiple miscarriages, history of previous premature births and diabetes Age 40+ pregnancies Pre-pregnancy medical conditions Infertility evaluation and treatments such as: Hormone treatments, fertility drugs and surgery