Search
-
When Should You Consider Hospice? 5 Important Signs
Deciding on hospice care for a loved one is a deeply personal and challenging decision, balancing their wishes and medical realities. Rebecca Edwards, DNP, from Renown Hospice Care, explains the signs indicating when it might be time for hospice and offers guidance on navigating this decision with compassion and clarity. Understanding Hospice Care Before exploring the decision-making process, it’s crucial to have a clear understanding of what hospice means. Hospice care represents a shift in how we approach living with a terminal condition, emphasizing comfort, dignity, and quality of life above all else. When there is no longer a pathway to a cure, side effects of treatment outweigh the benefits, or someone is simply tired of frequent hospital visits, then it may be time for hospice. Hospice care is mainly done in the home, where most people wish to be. It's a compassionate, team approach to care that focuses on meeting the physical, emotional, and spiritual needs, supporting their families, and honoring individual preferences. 5 Critical Signs to Be Aware Of Decline in Overall Health: When a loved one's health continues to decline despite ongoing medical interventions, this may be a sign that these treatments are no longer effective. Increasing Pain and Symptoms: When managing symptoms such as pain, nausea, fatigue or shortness of breath becomes increasingly challenging, hospice can offer specialized support and expertise in symptom management. Frequent Hospitalizations: Repeated hospitalizations or emergency room visits can signify that the disease has progressed to a point where managing symptoms and providing comfort at home or in a hospice setting is a more appropriate approach. Difficulty with Daily Activities: If your loved one is experiencing difficult with activity of daily living such as dressing, bathing, or mobility, it may be a sign that they require additional support and assistance. Prognosis of Six to 12 Months: Hospice Care is typically recommended for patients with a prognosis of about one year or less if the disease follows its normal course. However, it’s important to remember that every individual is unique and prognosis can vary.
Read More About When Should You Consider Hospice? 5 Important Signs
-
A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
Embarking on the path to bariatric surgery is a unique and deeply personal journey. Individuals like Mary Escobar choose this life-changing route for reasons ranging from improved cardiovascular health to managing diabetes or finding relief from various health complications. In Mary's case, her two-decade-long healthcare journey not only underscores the challenges she faced but also highlights the support and expertise that ultimately led to her successful transformation through bariatric surgery. Mary's Resilience: December 2002 through February 2003 More than two decades ago, Mary experienced unforeseen health complications just days after giving birth via c-section. Septic shock, hemolytic uremic syndrome, thrombocytopenia, renal failure and a blood clot in her lung plunged her into a critical state. Intensive care, plasma exchange and a long recovery followed. After being discharged with compromised kidney function, Mary faced complete renal failure two years later, leading to dialysis and a spot on the donor list. Mary's brother, a perfect match, selflessly donated his kidney on Dec. 14, 2007, marking a turning point in Mary's health. However, the post-transplant period brought new challenges, including diabetes, high blood pressure and a significant weight gain, reaching 230 pounds. Determined to regain control, Mary explored various diets without success until she consulted with a bariatric doctor. Journey to Bariatric Surgery: November 2009 - April 2021 In November 2009, Mary opted for a gastric band, shedding 40 pounds within a year. Despite initial success, issues with the gastric band arose, prompting a consultation with Dr. John Ganser at Renown Health in April 2021. Together, they decided to transition to a gastric sleeve, with comprehensive education provided to ensure long-term success.
Read More About A Transformative Journey: Mary's Bariatric Surgery Story at Renown Health
-
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
3 Ways to Foster the Wellbeing of LGBTQIA+ Kids and Teens
© alessandrobiascioli via Canva.com Ensuring a healthier and more inclusive future for LGBTQIA+ children and teens is of utmost importance to health systems in our community, especially Renown. Supporting the physical and mental health of youth in this community is key to those efforts, especially as they face unique challenges in terms of identity acceptance and social integration. Dr. Caroline Barangan, Adolescent Medicine Physician with Renown Children’s Pediatric Specialty Care, discusses what you as a parent, caregiver, friend or support system can do to be a safe space for children and teens who identify as LGBTQIA+. 1. Create a Safe Space at Home The most important action you can take for your LGBTQIA+ teen or child is to accept and support them for who they are, regardless of how they identify. “Being a teenager is already difficult enough, especially within the LGBTQIA+ community, which puts them at risk of being stigmatized, rejected and targets for bullying,” said Dr. Barangan. Your supportive words and actions can make a huge difference as a profound expression of love and understanding. Being patient and willing to learn are the foundations to a healthy and loving relationship with your LGBTQIA+ teen or child. 2. Encourage Regular Check-Ups with a Primary Care Provider (PCP) Establishing your child or teen with a PCP is not only important when an illness occurs but also for annual preventative visits and regular check-ups. “A primary care provider can screen for high-risk behaviors that would put a patient’s health in jeopardy, such as sexual experience, substance use, suicidality and self-harm,” said. Dr Barangan. “These screenings are an opportunity to provide the education and support these kids and teens need to stay healthy.” One of the main concerns LGBTQIA+ youth often have is that they will experience judgment from their provider, or the PCP will disclose sensitive information, including their sexuality or gender identity to their parents, when they are not ready to do so. Dr. Barangan emphatically reminds us that this legally cannot happen. “If a patient asks me to keep something confidential, unless they disclose that they have plans to harm themselves or others, I am legally not allowed to share that information with anyone without their permission,” said Dr. Barangan. 3. Locate Local Resources Northern Nevada is home to a variety of resources for the LGBTQIA+ community at large, including youth members of this community. "Finding resources to help them develop in a positive way and provide them with the information they need, whether it be in school, the household, the community or through a medical or mental health provider, is incredibly important,” said Dr. Barangan. Below is a list of local LGBTQIA+ community resources open to you and your children: Our Center LGBTQIA+ Health Services at Northern Nevada HOPES Northern Nevada Pride Festival & Community Parade (happens every July in Reno) Sassabration (happens every September in Carson City) Lake Tahoe Pride (events and resources shared on Facebook)
Read More About 3 Ways to Foster the Wellbeing of LGBTQIA+ Kids and Teens
-
Nurturing Your Child's Back-to-School Mental Health
The back-to-school season is here, and ensuring your child's successful transition involves more than just school supplies and schedules. At Renown Children’s Hospital, and in collaboration with Nevada Pediatric Psychiatry Solutions, we understand the vital role that mental health plays in a child's overall well-being and academic performance. Below we'll guide you through essential tips for a smooth back-to-school experience, with a special focus on nurturing your child's mental health. How to Support Your Child’s Mental Health from Home Remember, the below strategies can be adapted to align with your child's personality, learning style and household dynamics. Flexibility and understanding are key in tailoring these tips to suit your child's unique needs. 1. Be Open to Communication: Recognize that effective communication is the cornerstone of understanding your child's feelings and concerns. Create a safe space where your child feels comfortable expressing their thoughts. Listen to learn, without judgment. Make it a point to validate their emotions and ensure they are heard. Encourage sharing experiences,worries, friends and challenges they may be facing. Having open conversations about sensitive topics opens the door for discussion and understanding. Make yourself available. 2. Establish a Routine: A consistent routine can offer a sense of stability and predictability for your child, and anticipation helps to decrease anxiety and establish a sense of control. Join forces and design a daily schedule that includes time for schoolwork, play, physical activity, meals and relaxation. Be flexible about the structure to allow room for last-minute changes including extra activities based on that day’s needs as well. Always add time for play and bonding. 3. Practice Compassion: Back-to-school can come with big emotions. Listening reflexively and acknowledging these feelings can help you and your child act positively on these big emotions. 4. Get Involved: Actively engage in your child's school life by participating in school events, meetings and discussions. Show interest in their educational journey, ask about their experiences and provide guidance when needed. Being present in their academic pursuits not only boosts their confidence but also strengthens the parent-child bond. 5. Use Positive Reinforcement: Celebrate your child's achievements, no matter how small they may seem. This allows for a sense of accomplishment and boosts self-esteem. Praise efforts, progress and perseverance, whether it's completing an assignment, making a new friend or overcoming a challenge. This positivity encourages a growth mindset and resilience. 6. Organize a Schoolwork Zone: Create a comfortable workspace at home dedicated to school-related tasks. Customize the area based on your child's preferences and needs. Having a designated space for studying and completing assignments promotes focus, reduces distractions and enhances their overall learning experience.
Read More About Nurturing Your Child's Back-to-School Mental Health
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Department Spotlight: Infection Prevention
Hygiene in healthcare is an essential backbone to providing the safest, most optimal care to every patient. From everyday handwashing techniques and getting all necessary vaccinations to surveilling our health system before the onset of outbreaks, at Renown Health, creating and maintaining a low-infection environment is a group effort. From ensuring fundamental infection prevention practices are carried out to identifying process improvement opportunities, Renown’s Infection Prevention (IP) department is here to help care teams be successful in their role. This effort is led by members who are devoted in sharing evidence-based best practices to our patients, employees, healthcare organization partners and community. Making “Zero” A Reality Reducing healthcare-associated infections is possible when core infection prevention practices are incorporated into the daily care of our patients. These team members are dedicated to Renown’s commitment to creating a culture of Excellence, caring for our healthcare environment, and our care teams. “Often times, when asked what we do in our work it can be a challenge to answer because unpredictability is built into almost every day; and in that, we as a team must divide and conquer,” said Susanne James, Manager of Infection Prevention. Every day, each team member is assigned a day to perform required surveillance activities. Whether they are reviewing patients’ infections and isolation and evaluating lab orders for possible infectious processes or reporting communicable diseases to the local health authorities and the CDC, every Infection Preventionist participates in improvement projects and address issues as they arise. The Infection Prevention team plans, organizes, manages and evaluates the Infection Prevention Program and ensures IP policies reflect current best practice. They work closely with all departments at Renown in order to achieve high levels of standards that are implemented to reduce transmission of infection. “As a team, we perform ‘Infection Prevention Environment of Care Rounding’ on all units and departments to ensure our environment complies with regulatory requirements,” said Erika Clark, Operations Analyst at Renown Health. "We work together with Facilities and Site Practice Leaders to ensure a safe environment.” The pandemic challenged all Renown teams to find creative solutions for issues no one ever imagined. Our Infection Prevention department worked tirelessly alongside Renown's Hospital Incident Command Structure (HICS) and care teams in creating several lines of defense against COVID-19, including: Launching Renown's Alternate Care Site to meet the need for critical patients. Bringing on the new lab tests and specimen collection criteria. Managing demand for personal protective equipment (PPE). Bringing vaccines to staff and then to the community. Managing ill employees and our visitors. Keeping all locations informed on pandemic status and changes (which were occurring at breakneck speed). These initiatives enabled Renown's care teams to focus on providing the safest care possible to patients saving countless lives. This solidified the fact that together, the team can accomplish anything. “Infection Prevention is proud to be a valued and respected member of the care team,” said Susanne James. “We appreciate being a trusted resource and take this responsibility seriously as this enables us to provide staff the best possible tools to be successful.” Fight the Good Fight Against the Spread of Disease Educating patients and providers plays a huge part on the Infection Prevention stage. This team provides educational materials on a range of topics, some of the most important are, proper hand hygiene and the use of PPE. All these materials can be found throughout our health system and serve as an important reminder – infection prevention starts with all of us. “We partner with every aspect of the health system – environmental services, nutrition services, lab services, facilities, pharmacy, physical therapy and occupational therapy, respiratory care, patient access, security, nurses, providers and quality...just to name a few!” said Susanne James. Our Infection Prevention team also partners with Washoe County Health District and other public health agencies to report – and in turn, stop the spread of – diseases and exposures. These close partnerships poise our team to do what we do best: Fight the Good Fight. “I greatly appreciate everyone in the IP department for sharing their expertise as I learned a new position,” said Erika Clark. “I love working with my team and how closely we work with other departments to ensure excellence in all we do.” Our health system is ever-changing. But according to the experts in our Infection Prevention department, the three main ways to prevent illness and disease that remain the same time and time again are to: Clean your hands. Hand hygiene is the most effective way of preventing the spread of infections. The CDC recommends washing your hands with warm soap and water for 15-20 seconds or using an alcohol-based hand sanitizer. Clean your hands often and assist our patients to do the same. Learn expert hand-washing advice here. Get vaccinated. Immunizations are one of the top methods you can embrace the fight against preventable diseases, such as COVID-19, flu, measles, tetanus and more. Discover how you can get vaccinated with Renown. Keep germs from spreading. Practice good hygiene by covering your cough or sneeze or wearing a mask and sanitizing frequently touched spaces. Stay home if you feel ill to prevent the spread of illness and infection. Be sure to bring up any illness concerns with your primary care provider. “Every aspect of our health system has an infection prevention component, and we work daily to ensure our staff, patients and visitors are providing and receiving care free from potential harm or infections,” said Susanne James. “We are often the first call staff make when they have questions, concerns or just need someone to help improve process or outcomes.” Reveling with Renown Proudly defining themselves as a “small but mighty” team, the six-person Infection Prevention department moves mountains to ensure the safety of anyone who walks through Renown’s doors. The tight-knit nature of this team can be felt from miles away, and to them, being “small but mighty” is not a hindrance, as they have the support of the IP Champions and the entire health system. “I originally came to Renown in 2018 as a nurse traveler, the facility and people I worked with immediately made an impact on me,” said Brian Stroud, Infection Preventionist at Renown Health. “My wife and I chose Renown and Reno due to the positive impact the people had on us. Everyone is welcoming, helpful and caring. Now, I am a full-time employee, and the team has made my transition into infection prevention trouble-free." Renown’s mission of providing a genuine difference for the health and wellbeing of the community is heightened and echoed by the Infection Prevention team. “I chose Renown because of the reputation Renown has earned in the community because of the excellent care and level of services provided,” said Shannon Oriola, Infection Preventionist at Renown Health. “I absolutely love this team and my Renown family!” “What brought me to Renown was the opportunity to acquire diverse skills which then motivated me to pursue my master’s degree,” added Paul DeLeon, Infection Preventionist at Renown Health. “What keeps me here is the people – Renown attracts hard working, ethical and caring people.” "My wife and I loved coming out to the Nevada mountains on vacations," added Russ Laarman, Infection Preventionist at Renown Health. "After being in Michigan for 47 years, we took the plunge and made NV our home. The experience has been great! I work with a great team that is very knowledgeable and works hard to ensure positive outcomes for our patients and colleagues at Renown.” Their pride shines through with their own individual accolades, both inside and outside of work. This past year: Shannon Oriola received a scholarship from the Association for Professionals in Infection Control and Epidemiology (APIC) for “improving outcomes through knowledge and practice,” which provided her with a $1,000 scholarship to attend the annual APIC conference in Indianapolis. Paul DeLeon earned his Certification in Infection Control and Prevention from APIC. Erika Clark completed Renown’s High Potential program, a six-month program that gives employees hands-on learning experience with several competencies, including emotional intelligence, effective communication, building successful relationships and organizational knowledge. Brian Stroud and his wife Charla became official Nevada residents. Russ Laarman scaled Mount Whitney. ...And the list keeps growing! Charged with the goal of keeping disease spread at bay, our Infection Prevention team remains vigilant and dedicated to their mission. Their commitment to Renown and to keeping our health system clean and healthy proves the age-old saying true: not all heroes wear capes. “I’m so very proud of the work Infection Prevention does every day, working with the vast teams throughout the health system to improve lives,” said Susanne James. “We would like to thank all of you for protecting the health and safety of your colleagues, our patients and the community.”
-
Meditation: Give Yourself the Gift of Inner Peace
As we enter the holiday season, many of us are beginning to plan and partake in festivities such as shopping, cooking, baking, holiday parties and family gatherings. While the holidays often bring joy and cheer, the hustle and bustle can also lead to fatigue, stress, anxiety and sometimes depression. To avoid holiday burnout, it’s important to find ways to care for yourself mentally and physically. Galen Gorelangton, Renown's Spiritual Center Volunteer, discusses how yoga and meditation can benefit you. What is yoga and meditation? Yoga is defined as performing a series of postures and controlled breathing exercises to promote a more flexible body and a calm mind. As you move through poses that require balance and concentration, you're encouraged to focus less on your busy day and more on the moment. Meditation involves focusing or clearing your mind using a combination of mental and physical techniques. While there are many different types of meditation and yoga practices, they both share similar benefits including: Reduced stress Lower blood pressure Decreased anxiety and depression Increased energy Better sleep Lower inflammation and pain levels Improved strength, balance and flexibility Better focus and concentration And much more!
Read More About Meditation: Give Yourself the Gift of Inner Peace
-
Alzheimer's Safety Tips for Caregivers to Know
November is National Alzheimer’s Disease Awareness Month. At Renown Health, we know that Alzheimer's safety for your loved one is a priority, as the symptoms can sometimes lead to unsafe situations. We asked Dr. Jonathan Artz – a neurology physician with Renown Health and an assistant professor of clinical neurology at the University of Nevada, Reno School of Medicine – for tips on keeping loved ones safe and secure. According to the Alzheimer’s Association, Alzheimer’s disease affects safety in various ways, specifically due to body and brain adjustments. These changes can include: Judgment, including forgetfulness Sense of place – getting lost on the way home Behavior – being suspicious or fearful Body difficulty – losing balance Sensing ability – noticeable sensitivity in hearing, seeing or temperature Dr. Artz gives us four major tips to ensure your loved one’s safety as you both navigate this disease together. Watch for Wandering Those experiencing Alzheimer’s disease tend to wander and get lost. Try the following tips to reduce the risk of wandering: Get your loved one an ID bracelet and have them wear it at all times. You can also enroll your loved one in “Wandering Support.” Install door chimes so you know when exterior doors are open. Ask neighbors to call you if they see your loved one out alone. Go with your loved one when they insist on leaving the house. Don’t argue or yell. Instead, use distraction or gentle hints to get them to return home. Discourage Driving Driving can be unsafe for someone with this disease. With this in mind, ask a doctor whether it’s safe for your loved one to drive. For example, on a case-by-case basis, there are certain situations where doctors are required to report individuals with particular cognitive impairments, wherein a form of a driving assessment will be recommended. Limit access to the car. Keep the keys with you or lock them away. Ask an authority figure, such as an insurance agent or a doctor, to tell them not to drive. Adult-Proof Your Abode A simple living space is a safe living space. This means reducing clutter and removing any issues that may pose a safety concern. You may also want to get advice from an occupational therapist (home safety expert). Keep in mind that some changes may not be needed right away. Focus on major safety concerns first. Try the following tips: Add lighting (or glow-in-the-dark tape) to brighten dark areas, including stairways and halls. Use color contrast or texture indicators for dials, knobs and appliance controls. Remind your loved one not to carry items while walking to avoid a fall. Remove sharp objects from drawers and countertops. Avoid using small throw rugs or doormats, as they are easy to trip on. Move frequently used items so that they are easy to reach. Lock away alcohol and tobacco products, as they are not recommended for dementia patients. Install handrails in the shower, tub and near the toilet. Bathroom falls are especially common. Adjust the setting on your hot water heater so water does not scald. Those with Alzheimer’s can lose their sensitivity to temperature. Move and lock up hazardous chemicals and cleaning supplies, such as bleach and insecticides. Disable and remove guns or any weapons. Supervise any medication taken by your loved one. Promote a Positive & Healthy Lifestyle Continually emphasize the strengths of your loved one by promoting participation in meaningful activities, wellness visits and healthy habits to help them improve their well-being. Here are some ways to keep them physically and mentally active: Maintain regular vision and hearing screenings and make necessary adaptations. Establish a routine for daily activities. Encourage participation in self-care and leisure activities. Work with your loved one’s doctor to establish a healthy diet. Ensure proper hydration. It may help to set reminders for your loved one to drink fluids. Encourage regular exercise. Exercise delivers oxygen to the brain, improving brain health. Promote good sleep habits. Good quality sleep can increase overall brain health and has been associated with improving memory, attention and concentration. Resources and support are available with the Renown Memory Disorders Program. Providers within this program are specifically dedicated to treating several different memory-related disorders. Memory Disorders Resources & Support.
Read More About Alzheimer's Safety Tips for Caregivers to Know
-
Healthy Summer Salads
Reviewed by: Jessica Blauenstein, a Board-Certified Specialist in Oncology Nutrition and Registered Dietitian at Renown Health. As the temperatures continue to rise around northern Nevada, our farmer’s markets and home gardens are bursting with produce – making this the perfect time to prepare a fresh summer salad for you and your family. American salads have come a long way. No longer must we settle for iceberg lettuce topped with pale tomatoes and store-bought salad dressing. Fresh fruits, exotic vegetables and aromatic herbs are proudly taking up residence as entrees on menus around the globe. These refreshing Pritikin salad recipes are chocked full of phytonutrients – plant compounds that provide a host of anti-bacterial and anti-inflammatory benefits while supporting the body’s natural detoxification process. When it comes to ingredients, freshness counts! Try to use local and unsprayed produce in your salads whenever possible for added nutritional value. Already thinking of ways you can put your own personal touch on these recipes? Andria Herron, dietary educator with Renown’s Healthy Heart Program, encourages you to experiment. “Salads are the perfect recipes to substitute, omit and add in additional ingredients based on your personal preferences,” said Andria.
-
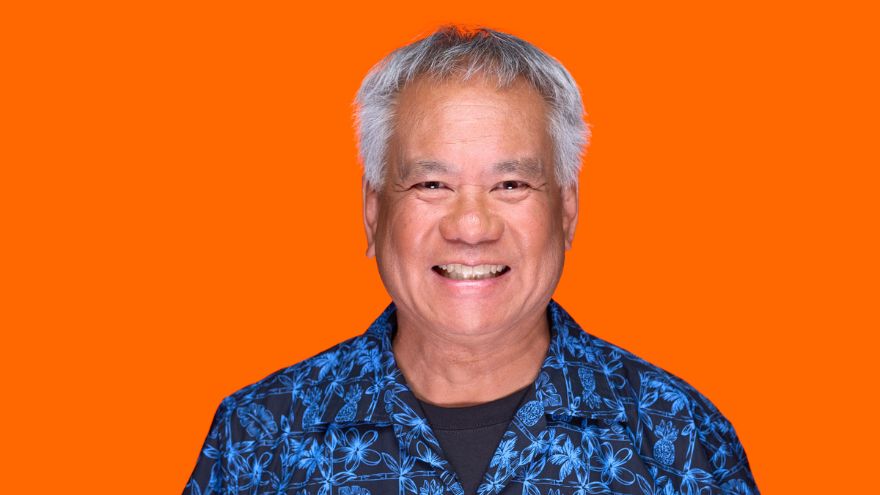
Meet Multifaceted Member Don Chang
Renaissance Don The Sterling Silver Club is honored to have thousands of members who’ve led and continue to lead incredibly vibrant and diverse lives. And we’re absolutely thrilled when those members volunteer to share their stories and experiences so we can all appreciate and learn from them. This issue’s featured member is no exception. From his love of cooking, travel and music to his drive to learn new languages, take on new hobbies and keep himself active and fit, Don is an aspiring Renaissance man who may already be deserving of the title. Revolutionary Family Roots Don’s father, who was born in Beijing, China, earned a master’s degree in metallurgical engineering from the University of California, Berkeley and was working on his PhD there on a full scholarship from his home country when the Chinese Communist Revolution occurred. In order to stay in the United States and avoid potentially being thrown into prison by the new communist regime (a fate that befell some of his family members), his father married Don’s mother, who was a U.S. citizen and also a student at Berkeley. Together, they started a family. “My father met my mother in a class and received his green card by marrying her,” says Don. “They proceeded to have six kids in nine years, I was number three. Dad never finished his PhD, but clearly earned what we like to call his “PSK” degree – Papa with Six Kids.” Proud (of) Papa: Don’s father was a professor of metallurgy and a brilliant research scientist who was responsible for virtually every breakthrough in the development of titanium in the 1960s.
-
Suicide Risk How to Spot a Friend in Crisis
How can you tell if a friend is in trouble or struggling with suicidal thoughts? And how can you support them in finding help? Are you feeling virtually exhausted? Life is always challenging, but the mental fallout of a global pandemic is real. Contributing to the loneliness epidemic is the shifting American lifestyle. More Americans live alone (28%) now than ever before, and fewer have kids. First, let’s acknowledge this is a time of anxiety and worry for everyone. Economic uncertainty, job transitions, grief, and loneliness are a perfect storm for mental stress. Even before the COVID-19 (coronavirus) pandemic mental health was a concerning issue, now it is a relevant topic of crisis. Secondly, anyone can struggle with suicidal thoughts. Those suffering from drug addiction are especially vulnerable. In particular the U.S. is currently seeing a rise in drug overdoses by almost 18% due to the pandemic. Unfortunately, suicide is responsible for one U.S. death every 11 minutes, according to the Centers for Disease Control and Prevention. Not to mention the millions who think about it, make a plan or attempt it. It is important to remember that suicidal thoughts, plans or intent must be helped immediately. Understanding Suicide Risk To clarify, depression is not a choice. No one wishes for endless days of feeling down, sleepless nights, and feeling as if you are in a dark tunnel. Currently, one in five Americans will experience a mental illness this year. This means one of your friends is struggling, right now. Specifically, consider this: When your body feels pain it talks to your mind. When your mind is suffering who does it talk to? So, how can you tell if a friend is in trouble? According to the National Institute of Mental Health be on the lookout for some depression clues below. Signs and Symptoms of Depression Persistent sad, anxious, or “empty” mood Feelings of hopelessness, or pessimism Irritability Loss of interest or pleasure in hobbies and activities Decreased energy or fatigue Moving or talking more slowly Feeling restless or having trouble sitting still Difficulty concentrating, remembering, or making decisions Signs and Symptoms of Suicide Risk Expressing feelings of hopelessness or having no purpose Talking about feeling trapped or being in unbearable pain Talking about being a burden to others Increasing the use of alcohol or drugs Sleeping too little or too much Withdrawing or isolation Displaying extreme mood swings. Talking about wanting to die or to kill oneself (Reference: Suicide Awareness Voices of Education) How to Help a Suicidal Friend It can feel awkward to approach the subject of suicide with a friend, but take any of the above warning signs seriously. Other ways you can help are by: Encouraging self-care and making sure they take care of basic needs Listen to their worries without judgement Ask them what they need from you, then follow through with action Let them know they are not a burden Don’t minimize or invalidate their feelings Point them to helpful resources Be their advocate and get them help If someone you know is in a life-threatening crisis situation, call 911 immediately. Suicide Risk Resources: National Suicide Prevention 24/7 Lifeline: 1-800-273-8255 Ayuda En Español: (Spanish National Suicide Prevention Lifeline) 1-800-628-9454 Crisis Text Line: Text HOME (or CONNECT) to 741741 to chat with a crisis counselor 24/7 free of charge. The National Alliance on Mental Health: 1-800-950-6264 Substance Abuse and Mental Health Services Administration: (SAMHSA) 24/7 helpline 1-800-662-4357