Search
-
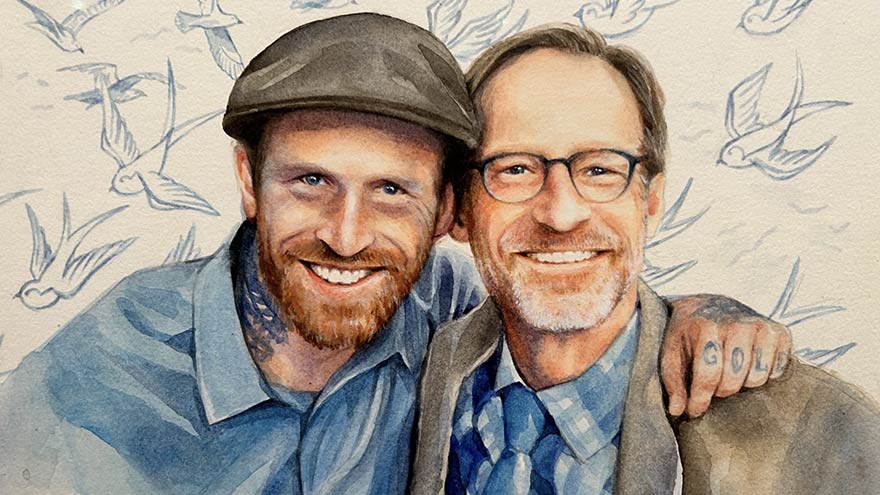
Why I Give: Dan’s Story
In the fall of 2020, Dan's world was suddenly shaken when he received a distressing call: his son, Jeremy, was admitted to Renown with complications from spinal meningitis. Without a second thought, Dan rushed from Southern California to be by Jeremy's side. For an agonizing 10 days, Dan remained in the ICU. He was overwhelmed with worry and helplessness as Jeremy fought for his life on a ventilator. During this time, Dan, an esteemed artist and professor, found comfort in the collection of artworks adorning the walls at Renown. With more than 2,000 pieces of original art, Renown has meticulously curated hospital rooms, hallways and various spaces to support those in need. Dan, who talks about art's magic every day as a professor, experienced its power in a new light.
-
Department Spotlight: Respiratory Care
This Department Spotlight is dedicated to Jason Simpson, Manager of Respiratory Services at Renown Children’s Hospital. Take a moment to breathe deeply. Inhale in, exhale out. We rely on our lungs to provide us with the air we need to live a healthy life – and this essential bodily function is something that many of us don’t think twice about since it comes easily for us. Now, imagine yourself as someone who is living with severe asthma, chronic obstructive pulmonary disease (COPD) or someone who was recently diagnosed with a frightening respiratory condition like COVID-19 or pneumonia. The simple act of breathing can prove to be an intimidating venture requiring the care of a professional. Who are the people that take on the challenge? Meet Renown Health’s Respiratory Care Services department. Serving patients across 13 service lines, three acute facilities, outpatient locations and telehealth, our respiratory specialists – including respiratory therapists, respiratory care aides, inpatient COPD respiratory therapy navigators and educators and more – use their expertise to help restore the vitality of all their patients with every inhale and exhale, shaping a healthier livelihood one lung at a time. The Guardians of Respiratory Wellness Whether they are managing lifelong respiratory conditions or offering crucial support in emergencies, the Respiratory Care team strives to enhance the quality of life for every patient. As an indispensable member of the clinical team at Renown, our respiratory therapists work collaboratively with doctors and nurses to tackle a wide range of tasks, tailoring care for each patient’s unique needs. “Respiratory care is involved with all stages of life, from beginning to end,” said Sarah Kurtz, Respiratory Therapist. “We work closely with nurses and doctors and perform arterial punctures, breathing treatments, weaning maneuvers for patients on life support, intubations and much more. We assess patients constantly to see if their care needs to be upgraded or if they can be weaned to get them back home with their families.” “You start your morning researching your assigned patients,” added Tim Start, Respiratory Specialist. “We go over lab values and chest radiographs and decide the best plan of care for each patient. Our objective is to improve their respiratory status by giving them medications and doing breathing exercises. We participate in other forms of care with nurses, such as activities of daily living (ADLs) and mobilization. We work as a team, and that enables us to provide great patient care.” For patients living with COPD, enjoying all that life has to offer comes with a separate set of obstacles. According to the Centers for Disease Control and Prevention (CDC), over 200,000 people across the Silver State are living with this chronic condition. Luckily for them, Renown has a specialized team to help these patients optimize their life and manage their condition with individualized treatment and education. “We run a report every morning to identify all the patients currently admitted who have a history of COPD, take respiratory medications or smoke,” said Amber Beck, Inpatient COPD RT Navigator. “After looking through their charts, we visit with the patient (and possibly their family) at the bedside to help them better understand how to manage their breathing issues.” As a vital part of the Respiratory Care team, Renown’s respiratory care aides help ensure the seamless operation of our respiratory care services. These dedicated professionals provide essential support to respiratory therapists not only during intricate procedures but also outside of face-to-face patient care by transporting equipment, restocking supplies, assisting in the mobilization of patients and more. “We are responsible for the maintenance of unit supplies and making decisions regarding levels of stock to be maintained,” said Dia Ramos, Respiratory Care Aide. “We also transport equipment, refill the oxygen tanks on the floors and intensive care units (ICUs), order and stock respiratory care supplies, mobilize patients and assist the respiratory therapists during bronchoscopies in the ICUs. In addition, we clean respiratory equipment like mechanical ventilators, continuous positive airway pressure (CPAP) and bilateral positive airway pressure (BiPAP) machines, high flows and aerosol poles.” Once the COVID-19 pandemic hit, a special spotlight shined upon respiratory care teams across the country for the heroic care they provided patients in respiratory distress. While their roles in health systems have gained a better understanding nationwide, this team understands it is vital for them to educate the community about the important jobs they hold for our patients. “Respiratory care can be under the radar,” said Pam Umek, Respiratory Specialist. “Once, when I told someone that I am a Respiratory Therapist, they said, ‘Oh, like a yoga breathing instructor?’ I then explained all the things we do: intubation, extubation, bronchoscopies, transports, traumas, codes, rapid responses, pediatrics/NICU, breathing medications/therapies, open heart rapid ventilator weaning … needless to say, that individual walked away with a better understanding of not just Respiratory Care Services but also the enormous effort it takes to care for our community.” The accolades and achievements continue to pour in, from national awards and certifications to implementing different jobs in care units to optimize the patient care experience. “We have earned and continue to maintain the Joint Commission Disease-Specific Certification for COPD,” said Amber Beck. “We are well below national averages for 30-day readmissions, lengths of stay and mortality due to COPD. Sandy, one of our COPD Coordinators, was a recipient of a patient advocacy award from the American Association of Respiratory Care and FACES Foundation.” “We have started implementing Respiratory Care Aides in the critical units, starting with the Cardiac ICU,” added Dia Ramos. “We work as one team and are always helping each other with their tasks.” Education and mentorship are at the core of Renown’s mission to make a genuine difference in the health and well-being of every patient. Nurturing the next generation of medical professionals – including respiratory care professionals – is a task that the Respiratory Care team takes seriously. “It has been great being able to help educate students in different disciplines,” added Pam Umek. “We have been able to offer shadow shifts to students in emergency medical services (EMS), nursing and medical school. These opportunities help students entering the medical field have a better understanding of the many ways we can help care for our respiratory patients.” From the moment of birth to the final stages of life, Renown is fortunate to have a Respiratory Care team that tirelessly ensures every breath counts, safeguarding their role as a trusted partner within our health system. A Tribute to Jason Simpson, Healthcare Hero
-
Department Spotlight: Renown Transfer and Operations Center
Stepping into the Renown Transfer and Operations Center (RTOC) means stepping into a transformative hub of excellence where lives are saved and healthcare is reimagined. As a cornerstone of Renown Health's commitment to exceptional patient care, the RTOC serves as a dynamic nerve center that seamlessly coordinates medical resources, ambulance rides, hospital bed space, remote home systems, hospital transfers and emergency preparedness. In this best-in-class facility, the boundaries of what is possible in healthcare are constantly pushed, and new horizons of patient care are discovered. Staffed with a dedicated team of skilled professionals, the RTOC harnesses the power of advanced technology and compassionate expertise to ensure that patients receive the highest level of care and support, no matter where they are. Through a synchronized network of communication, coordination, and compassionate care, the RTOC team ensures that patients receive the critical support they need when it matters most, working tirelessly to redefine what it means to deliver world-class healthcare. A National Standard Charged with the goal of overseeing the placement and transportation for every patient, the RTOC officially launched in 2021 as northern Nevada’s first and only transfer center of its kind and a nationally celebrated facility. As Renown’s highly coordinated care logistics system, this team uses the cutting-edge technology at their fingertips to customize healthcare to the needs of every patient, manage patient flow and drive healthcare innovation. “Compared to where we’ve started to where we are now, it’s a 180-degree difference,” said Kelli McDonnell, Manager of RTOC. “When we first started building our facility right before the pandemic happened, we took what was six conference rooms and classrooms and turned it into a command center that organizations across the country admire and come to Reno to see what we do. Mel Morris, the Director of RTOC, was recruited exclusively to build our facility with her history of building successful hospital command centers. Many people didn’t realize what a transfer center was or that Renown was the only center in the region – and we only continue to grow.” This best-in-class facility, and the masterful team behind it, handles: Coordinating all incoming patients transferred from neighboring hospitals and 27 counties across northern Nevada, Lake Tahoe, northeast California and neighboring states. Matching patients to the most appropriate bed placement using diagnostic, triage and Epic electronic medical record clinical information in conjunction with medical staff expertise to outline a plan of care that determines the best bed assignment given the patient’s needs. Coordinating video-enabled Telehealth monitoring capabilities for Renown’s four Intensive Care Units (ICUs), as well as Renown patient Telehealth and virtual visits. Monitoring Remote Home systems with Masimo during the COVID-19 pandemic, where some patients received hospital-level care in the comfort of their own homes while Renown clinicians monitored and evaluated their data and plan of care. Serving emergency and disaster management for area hospitals, first-responders and the community with local, regional and statewide emergency and disaster management for sudden-onset emergencies. The RTOC is home to many different critical roles for our health system, including Transfer Center Nurses, Ride Line Coordinators, RTOC Coordinators and more, many duties of which each team member cross-trains on to be able to fill in whenever needed. While their roles may differ, their commitment to their patients remains the same – and they all work together to achieve the same outcome: delivering the right care, at the right time and place. “As an RTOC Coordinator, we do a variety of different things,” said Anna Schaffer, RTOC Coordinator. “We do triage coordination to help our nurses and hospitalists get patients in the emergency department admitted, and we also do bed control to find patients appropriate bed placement. Communication is important, so we always make sure to stay closely connected with the charge nurses on those floors.” “We start with a basic ‘need to know’ and place patients accordingly,” added Karly Brown, RTOC Coordinator. “We get surgery numbers, ICU capacity and discharges and find beds for all patients as quickly as possible. We have the advantage of being able to see the entire hospital.” “I primarily schedule transportation for patients at the hospital who are either going home or going to a skilled nursing facility,” said Sarah Clark, Ride Line Coordinator. “I get requests from case managers to schedule rides, and I work with REMSA and other ambulance services to schedule them. It relies a lot on appropriate and efficient communication and critical thinking.” Patients in facilities across northern Nevada and northeastern California, especially the rural communities, look to the RTOC to help guide ambulances, bed coordinators and hospital staff in finding care for our rural patients. “As a transfer center nurse, I facilitate incoming patients from rural facilities in Nevada and surrounding areas in California,” added Meg Myles, Transfer Center Nurse Specialist. “There are days we may take up to 30 direct admissions from these areas.” “We are the point of contact for inter-facility transfers, whether we are sending patients out or bringing them into Renown,” said Lisa Lac, Transfer Center Nurse Specialist. “We take phone calls from those rural areas, identify what services are needed, connect them to the appropriate provider and coordinate any transfers.” “Simply put, we are the bed wizards,” said Addison Rittenhouse, RTOC Coordinator. The RTOC team continues to break barriers and push the boundaries of medical excellence through leveraging the technology at their fingertips and their unwavering dedication to the health of our community. Inspiring a new era of medical possibilities, these team members have achieved a multitude of accomplishments for both their department and their patients since the birth of the center. “We have significantly reduced the time it takes to get patient admit orders in, thanks in part to the new Triage Coordinator role, and we provide easier access for patients to transfer to us from other facilities,” said Beth Rios, RTOC Coordinator. “We have taken a bigger role in helping the smaller hospitals in our area in caring for patients and improve patient throughput.” “As a team, we’ve done a lot of work in creating an engaging and positive environment, and our internal morale committee has been a huge help with that,” said Kelli McDonnell. “We’ve been working tremendously over the last year and taking all the feedback that we received from the Employee Engagement Survey to make improvements. We had 100 percent survey participation within five days, which is incredible.” “I am so proud of our escalation and problem-solving skills,” said Becca Dietrich, RTOC Coordinator. “When an issue is raised to us, we will always find a timely solution on our end so our care teams can focus on the issue in front of them. We are the eyes in the sky, seeing movement everywhere.” Each day in the life of our RTOC team members is a testament to their commitment, resilience and timework, making a profound impact on countless lives.
Read More About Department Spotlight: Renown Transfer and Operations Center
-
Employee Blog: Team Renown at Northern Nevada Pride
It’s July 23, 2022, and I am arriving in Downtown Reno to walk in my first-ever Pride Parade. Even more amazing, I am going to be walking with a group of my coworkers, announcing to our entire community that our employer supports us being our full and truest selves. I arrived alone, but in the staging area I met new people who worked in other departments of Renown, coworkers I might never have met if not for Pride. I even took a selfie with one of these new friends. Someone passed around flags for us to hand out to the audience as we marched by. I took a rainbow-striped temporary tattoo in the shape of the Renown “R” and used my water bottle to apply it. There was an overwhelming atmosphere of excitement and joy that can only come from gathering with other human beings who are overflowing with love. We started the Parade waving handfuls of Pride flags high and gave those flags out to the audience as we passed. By the time we were done walking, our hands were empty, but our hearts were full. I couldn’t have stopped smiling if I’d tried. I’d joined the parade as a single person, but as we walked, I became part of a community. Not only the Renown community, but a community of Proud queer people across northern Nevada. And by extension, the LGBTQIA+ community all around the world – past, present and future. With the multiple recent state laws proposing to strip away the rights of LGBTQIA+ people, many of us have felt a noticeable decline in our mental health and feelings of personal safety. As a member of the queer community, I have felt these mental health effects too. I am fortunate and privileged enough to not have experienced workplace discrimination in my current position. But before Renown, I – like so many others in the LGBTQIA+ community – had a negative experience at a previous job, and afterwards I was hesitant to share my full self while at work. To be able to walk in a Pride Parade with my current employer, healed a little bit of that past pain inflicted by my former employer. When our liberties are under attack, Pride is more important than ever. We must remind ourselves, especially when others cannot seem to remember, that we are loved and worthy of love. I am grateful to work for an organization that is willing and able to fight this good fight with us. I will certainly be back to walk in this year’s Pride Parade, and I sincerely hope to see you there too! Be sure to wear comfortable walking shoes, sunglasses and of course keep your skin safe with sunscreen. Whether you’re part of the LGBTQIA+ community, or just an ally, you are welcome.
Read More About Employee Blog: Team Renown at Northern Nevada Pride
-
Living with COPD? How to Maximize Your Summer Experience
June offers an official welcome to summer and the height of outdoor activities in northern Nevada such as hiking, camping, days spent at the lake and embracing long days and warm evenings with friends and family. Enjoying all that the summer season has to offer may not be as easy for those living with chronic obstructive pulmonary disease, or COPD, which effects more than 15 million Americans. What is COPD? COPD is a group of lung diseases including emphysema and chronic bronchitis that result in airflow blockages from the lungs. People may experience frequent coughing and shortness of breath among other symptoms. COPD typically impacts adults ages 65 and older and is becoming increasingly more common among women. Although smoking plays a key role in the development of COPD, air pollution and indoor air quality, and respiratory infection also contribute to disease development. While there is no cure for COPD, limiting progression of disease and managing symptoms can be achieved through lifestyle changes, therapy, and medications. Tips for Living with COPD This Summer, and Always Stay Hydrated: Staying hydrated is extremely important for people with COPD, especially during the summer. Not drinking enough water can make breathing more difficult because it increases respiratory symptoms. Make sure to always keep a water bottle with you and aim to drink 8-10 glasses of water daily. Be Mindful of Temperature: COPD symptoms can be exacerbated by hot weather. It is best to participate in outdoor activities during the cooler times of day, like the morning or evening. Check Air Quality Before You Go: Before engaging in outdoor activities, be sure to check the air quality index and plan your activities accordingly. Pace Yourself: Exercising can be difficult for people who have COPD. To make the most of your summer, try not to push yourself too hard and take breaks when you need them. If you start to feel out of breath or tired, take a break in a cool, shaded area until you feel better. Take Matters Into Your Own Hands To address the needs of community members living with COPD, the Renown Health Research Office has teamed up with Pulmonary Medicine to provide patients who are former or current smokers and have a history of frequent exacerbations with an option to participate in the ARNASA study. "COPD exacerbations have a huge negative impact on patient’s lung function” states Dr. Farah Madhani-Lovely, Chief of Pulmonary Medicine at Renown Health and Assistant Dean of Clinical Research at the University of Nevada, Reno School of Medicine. “We have had inhalers and prednisone for decades but patients are still having exacerbations. Now we have a new pathway we think will prevent exacerbations which is what this clinical trial is designed to prove.” This study will evaluate the efficacy and safety of astegolimab compared with placebo in participants 40-80 years of age with COPD. “This study in particular is so exciting because of the enthusiasm from the sponsor’s end” says Katie Buckley, Lead Clinical Research Coordinator working on pulmonology studies at Renown’s Clinical Research Office. “Often times sites aren’t assigned particularly passionate or engaged personnel who aid in carrying out these studies, but you can tell Roche Genentech’s team truly cares about the success of the study, the safety of their participants, and proving the efficacy of the investigational agent. Working on a study like this takes a village, and when the individuals on all ends share similar mindsets and work towards success as a collective unit instead of as individual moving parts, it’s amazing to see everything we’re able to accomplish.” Renown’s team of expert pulmonologists and researchers are available to join patients with COPD in support of their healthcare journey. If you are interested in learning more about this clinical trial option at Renown Health, talk to your pulmonologist at your next appointment or contact us at 775-982-3646. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
Read More About Living with COPD? How to Maximize Your Summer Experience
-
Department Spotlight: Patient Access
Health systems across the country recently celebrated Patient Access Week from April 2-8. Join us in recognizing our Patient Access team at Renown! Fighting the Good Fight starts the moment a patient steps onto the grounds of our health system. When patients visit Renown on their healthcare journey, they look to the experts to not only help them navigate through the complexities of the process but also ensure their experience with us starts off on the right foot. Renown Health’s Patient Access Representatives (also referred to as “PARs”) are the faces of this entire process. As the key links between patients, providers and insurers, they strive to create a welcoming and respectful environment for everyone. PARs are committed to providing all of Renown’s patients access to the quality care when needed. After all, it’s in their name! A Friendly Face PARs are the front faces of almost all clinical areas at Renown. As the starting point for much of the patient experience, the day-in-the-life of PARs can vary. Checking patients in and out, getting demographic information, verifying insurance, answering phone calls, fostering communication between patients and their care teams, scheduling patients for follow-ups, explaining financial responsibilities and our financial aid programs, creating an overall positive experience and environment, the list goes on – but they all remain united under one goal: setting patients off on the right foot as they access care through our health system. “Each day, PARs are met with new patients who are seeking solutions to different concerns,” said Macy Betts, PAR for Renown Women’s Health. “We are the front doors to this department. We are not just checking patients in and out; we are the first step to the patients receiving the care they deserve.” “We take pride in our work,” added Tanya Quintanilla, Shari Longley and Nancy Arroyo Garcia, PARs for Renown Pediatrics. “Usually, we are the first point of contact within Renown, so we don’t take our role lightly. For example, when we see a newborn, we must ensure the registration has been verified, which consists of patient demographics, patient preferences and insurance verification. We need to be consistent and thorough because what we do affects every point of contact a patient may have within Renown.” “As my team’s senior PAR, my day begins with gathering the outpatient therapy work queue numbers and assigning the team to work them,” added Logan Johnson, Senior PAR in Pre-Registration at Renown. “Our goal is to contact and schedule patients for physical, occupational and/or speech therapy as soon as possible so that they have the maximum benefit and can get back to a normal life as quickly as possible. Our encounters can make or break the entire experience.” PARs never underestimate the power of good communication and compassion. Even during the busiest of times, our PARs work diligently to ensure all patients and their care teams fully understand the administrative side of whichever part of their journey they are about to embark on, lending a helping hand and a smile. “Whether you’re communicating with patients, leaders or coworkers, communication is key,” said Jonathan Figueroa, PAR for the Renown Institute for Heart & Vascular Health (IHVH). “We try and make sure that we do everything possible to make their visit go as smoothly as possible.” “Communication makes the world go round,” added Keith Madrona, Sherry Riley, Erika Rios and Andie Kilpatrick, PARs at Renown Urgent Care – Ryland. “Having a friendly attitude and demeanor is very important. “The PARs in Labor & Delivery do so much more than just registering patients – from escorting expectant parents to their rooms, welcoming newborn babies, processing pre-estimates and more – and the patience and excellent communication I receive from other teams is what keeps me going,” added Nanci Barash-Vietti, PAR for Renown Labor & Delivery (L&D). “This is critical to the success and effectiveness of the PARs in our department.” Shift changes for PARs mimic other teams at Renown, leveraging technology and both written and spoken communication to ensure the next shift begins successfully. "When I come in, the night shift will give me a report on what is going on and what the schedule looks like during the day; then I log in to my computer and get everything that I will need for that day up on the screen,” said Allie Boracchia, PAR for Renown L&D. “Usually around this time we have a 7-8 a.m. induction scheduled for the first patient, so I will grab the pre-made packet that the night shift put together, the unit clerk will call the nurse to get a room number, and I take the patient to the room and have them sign all the forms. After the patient has the baby, then we admit them and finish registration. This is continuous all day long.” Our PARs all agree that regardless of the setting, whether it be emergent or routine, every patient is looking for that advocate from the moment they enter through our doors. “Being friendly, patient and understanding is a must,” said Sheryl Lundgren, PAR for the William N. Pennington Institute for Cancer. “It is so nice being able to brighten the days of patients who are living with a cancer diagnosis.” “In the urgent care setting, a lot of the patients we see are not feeling their best, so it is important that we show them we care and are here to help make check in go smoothly,” added Sam Deithrich, PAR at the Renown Urgent Care – Los Altos. “Patients are relieved that they are speaking to a real person that will help set up appointments,” added Rick Jordan and Celeste Landry, PARs in Lab Services at Renown South Meadows. PARs embrace lifelong learning at Renown, especially as their roles differ day-to-day. They are always ready to jump in and assist on tasks that might be new for them, growing their skills on the job and never hesitating to say, “How can I help?” “As a PAR, you are always learning new things, even when it seems like you know just about everything,” said Liz Cardenas-Ramos, PAR for Renown Endocrinology. “It’s been such a positive experience.” “Giving yourself grace to learn and grow in Patient Access is the key,” said Maggie Savoie, PAR for Renown Primary Care – Fernley. “I find myself learning every day at Renown, and if you’re learning, you’re growing. Being able to take a breath and say, ‘this is a learning opportunity for me, and tomorrow I will be better a better PAR because I’ve gained this knowledge’ is an amazing way to stay positive in the position.” “In L&D, we are all multi-tasking, and every day I am learning something new about my department and patients, as well as how to excel in my position,” added Nanci Barash-Vietti. Renown PARs are the front lines to health care access, and they wear that badge with pride. Jeanette Flores, PAR in the Emergency Department at Renown South Meadows, sums up the role of Patient Access well: “Talk about first impressions!” “I am proud of our team and the excellent care we give our patients,” said Dawn Linker, PAR for the Renown IHVH. “We want them to have a good experience.” Impactful Accomplishments The role of our Patient Access team members goes beyond the desk. A patient’s healthcare journey begins, and sometimes even ends, with the helping hands of our PARs, leaving a lasting positive impression of Renown. "Our interactions with the patients make a difference before they see the provider, so we always demonstrate a welcoming and helpful atmosphere for the patients to feel like their needs are being met,” said Mary Dettling, PAR for Renown Endocrinology. “I love seeing the difference we make in peoples’ lives,” added Shannon Leone, PAR for the Stacie Mathewson Behavioral Health & Addiction Institute. “We can get patients at their toughest and worst times. Watching them overcome their fears, traumas and addictions has been very rewarding.” Our PARs don’t just make goals for themselves – time and time again, they surpass them, all in the name of patient experience and excellence. “We have not only met our monthly point-of-sale scores, but we also have exceeded our stretch goal for the last eight months and our scores have been in the 50th percentile or higher,” said Jeanette Flores. “Along with being the top point-of-sale collectors, we have also been known to be some of the sweetest and most helpful staff at South Meadows,” said Katie Morrill, PAR in the Emergency Department at Renown South Meadows. As their teams grow, so does their impact on our patients. PARs are dedicated to providing the best customer service possible, and with their expanding teams, that service goes even further, even throughout the pandemic. “A year ago, we only had one PAR; now, we have a full and amazing team,” said Alex Bucholz, PAR for Renown Advanced Wound Care. “We have come so far in a short amount of time.” "During the pandemic, we have maintained a core group of individuals who come in every day and help keep this office and all its parts moving smoothly,” added Shannon Leone. “We have maintained a full patient load the last three years and never had to close our office for any reason. We have even had the opportunity to start our Medicated Assisted Treatment and Transcranial Magnetic Stimulation programs.” "We successfully operated and maintained our pediatric COVID clinic, which is the only one within our five clinics,” added Tanya Quintanilla, Shari Longley and Nancy Arroyo Garcia. “We feel proud knowing our tiny humans are protected with the COVID vaccine.” Like many other teams at Renown, our PARs are masters at teamwork. Despite any obstacles that may happen along the way, they are always there for each other to ensure every patient gets the care and attention they deserve. “We call ourselves the ‘A-Team’ here in Pulmonary,” said Shannon Birnberg, PAR for Renown Pulmonary & Sleep Medicine. “We have persevered through changes, additions and departures. We are most proud of bringing different personalities to the team and being super strong and effective.” “I have noticed the team always steps up whenever needed,” added Brittany Hughes, PAR for the Renown IHVH. “Everyone has a great attitude and is very positive!” “While our team is fairly new, we are growing together, learning our strengths and weaknesses and always pushing for stronger unity,” added Angel Freer, PAR in the Emergency Department at Renown Regional. When our PARs find ways to simplify a process or make a workflow run more efficiently, they don’t waste any time in making that happen. They take any opportunity to enhance patient experience. “Our team came up with a solution on how to get patients registered faster,” said Jess Castillo-Marquez, PAR in Lab Services at Renown Regional. “We came up with modalities which assign each PAR their own procedure in which they will be registering for during their scheduled shift. It has been a great success, helping our productivity and keeping our patients satisfied with our service.” “We are proud of our successful implementation of our new therapy workflow,” added Logan Johnson. “Patients are now waiting much less to be contacted about their care.” Our PARs know that teamwork makes the dream work, and their commitment to the patients they serve – and the goals they continue to blow out of the water – continue to inspire them daily. “You are only as strong as your team,” said Aundie Yonker, PAR in the Emergency Department at Renown Regional.
-
Your Ultimate Cold and Flu Survival Guide
While viruses can attack year-round, colds, flus and other respiratory illnesses are typically more prevalent during fall and winter. People spend more time indoors, which allows viruses to pass more easily from one person to another. The cold, dry air can also affect the respiratory system, making it more susceptible to germs. According to the CDC, flu activity in the U.S. often begins to increase in October and peaks between December and February. “Flu season” can last as late as May. When it comes to the cold and flu, prevention and preparation are key. Getting the flu shot and a COVID-19 vaccine is the first and most crucial step in protecting against these two respiratory illnesses. Preventative actions, such as washing your hands, covering your mouth and nose when coughing or sneezing and getting enough sleep can also help you avoid getting sick. However, despite your best prevention efforts, the time may come this winter when you start to feel a little scratch in your throat or a fever coming on. By taking steps ahead of time to assemble a cold and flu survival kit, you’ll be more prepared for whenever illness strikes, allowing you to stay home, rest and avoid spreading germs. Tips for Managing Symptoms Keep these tips in mind to ease your cold or flu symptoms: Stay home and rest Drink plenty of fluids Treat aches and fever with over-the-counter medication such as ibuprofen or acetaminophen Manage a cough with over-the-counter expectorants or suppressants Run a humidifier or sit in a steamy bathroom to ease congestion What to Stock in Your Flu Survival Kit Be ready when a cold or the flu strikes by having a flu survival kit filled with these get-well essentials stocked in your pantry, fridge and medicine cabinet: Over-the-Counter Medications: Take advantage of over-the-counter medications to make yourself feel better and ease most common flu symptoms of fever, headache, cough, muscle aches, sore throat, and runny or stuffy nose Pain relievers - Ibuprofen (Motrin and Advil) or Acetaminophen (Tylenol): for fever and aches Decongestants: for sniffles and congestion Cough expectorant (guaifenesin): for a “wet” cough to help clear secretions from the lungs Cough suppressant (dextromethorphan/DM): for a severe “dry” cough to block the cough reflex Cough syrups and drops Drinks: Water Herbal tea Low-sugar sports drinks Pedialyte Foods: Chicken soup Broth Vitamin C-containing fruits and vegetables Oatmeal Toast (add some avocado, honey or egg) Miscellaneous items: Tissues Lozenges Protective mask Thermometer Humidifier When to Seek Care and Where to Go Most healthy adults who have a cold, the flu, or other mild respiratory illnesses don’t need to see a care provider and will recover at home with self-care measures. Because these are viral illnesses, antibiotics won’t work against treating them. Your care provider may be able to prescribe an antiviral medication that can relieve your symptoms and shorten the duration and severity of your illness; however, this needs to be started within 48 hours of symptom onset and is often only prescribed to individuals at high risk for developing complications from the flu or those experience severe symptoms. Primary Care or Urgent Care Contact your primary care provider or visit an Urgent Care if you are at an increased risk, including those who: Are 65 years of age or older Have chronic medical conditions Are pregnant or recently gave birth Have a weakened immune system Find a primary care provider If you are otherwise healthy and not at increased risk of complications, seek medical advice if your flu symptoms are unusually severe, such as mild difficulty breathing, a severe sore throat, coughing that produces a lot of green or yellow mucus, or feeling faint. Emergency Care Go to the Emergency Department if you are experiencing emergency warning signs such as severe pain (chest, abdomen), concern for heart attack or stroke (slurred speech, new localized weakness), severe dehydration (needing IV fluids) or severe shortness of breath.
-
Top Safe Sleep Tips for Your Baby
Becoming a parent for the first time means lots of new unknowns – from learning to breastfeed and swaddle to buckling your newborn into the car seat for the first time. But when it comes to putting them to bed safely, it’s important to remember it really can mean life or death. It’s something we’re taught before our little one is even here: the correct way to put your baby to bed safely. Sadly though, the number of infant deaths continues to climb. The main culprit of sleep-related infant death continues to be all the items parents leave in the crib with their babies. According to the Center for Disease Control and Prevention, there are about 3,500 sleep-related deaths among babies each year. “The best advice is ‘bare is best.’ Keep your infant’s sleep space clutter free – no blankets, bumpers, toys or pillows,” said Karen Wagner, Pediatric Nurse Practitioner. Follow the ABCs for Safe Sleep Remembering the ABCs is an easy way to remember how to put your little one to bed safely. A: Alone No blankets, toys or pillows. “We do recommend using a sleep sack as a blanket alternative,” said Karen. “It prevents the risk of suffocation and keeps your baby warm.” Keep in mind, the greatest risk for suffocation happens when babies are under 1 year of age, so it’s best to save the toys, blankets and pillows for their “big kid bed,” or around 18 months old. B: Back The slogan “back is best” is another good reminder. Keeping your baby on their back until they’re old enough to rollover helps reduce the risk of Sudden Infant Death Syndrome (SIDS). C: Crib It is best to have your baby sleep alone in their crib. While co-sleeping may be enticing, especially after a late-night feed, it increases the risks of possible suffocation. However, “having your child in your room, in their own crib or bassinet, is protective for SIDS,” Karen said. “In fact, we think co-rooming reduces SIDS risk by almost 50 percent.” Co-rooming allows parents to keep new babies in close reach and helps parents oversee their baby’s sleep, just in case something happens.
-
Department Spotlight: Clinical Engineering
Renown Health strongly supports and advocates for innovative medical technology. Our diverse lineup of medical equipment enables our care leaders to provide quality care to every patient. But what if a piece of technology breaks down? What happens when our care teams are ready for technological upgrades? Where do employees go when they have a question about a complicated piece of equipment? Enter the Clinical Engineering department. This sophisticated team is staffed with intelligent, science-minded individuals who are ready to jump in and help at any given second. From newborn incubators to robots that clean the hospital floors, these team members are the med-tech masters that keep our health system running. Equipment Experts Upon entering the Clinical Engineering department’s workshop, you are welcomed with an abundance of high-tech equipment undergoing repairs and upgrades. The department takes care of more than 26,000 pieces of equipment throughout the entire healthcare network, including the technologies at the University of Nevada, Reno School of Medicine, which they just took over this past year. To the average person, this may seem overwhelming; however, for this team, this is the exact environment they thrive in to make the technology magic happen. “I am motivated and engaged every day at work,” said Tony Martinez, Supervisor of Clinical Engineering for Renown. “Our department is fast-paced and rewarding, and that’s a big plus.” While some team members enter the department as equipment generalists, this team offers training to develop their skills on certain pieces of equipment, eventually becoming specialists. “Every month, we encourage our colleagues to undergo specific training on more delicate equipment,” said Tony. “Once we get to that point in their training, we assign different equipment to our team members every month. They pick up the experience very quickly.” As a Clinical Engineering Technician for Renown, Rylie Nickerson took advantage of the training and educational opportunities offered to her and is now a ventilator specialist especially for Renown’s neonatal intensive care unit (NICU). “Regardless of whether I’m working on ventilators or on another piece of equipment I’m assigned to, I’m always thinking about how I can help the patients, nurses and doctors,” said Rylie. Raul Hernandez, a Clinical Engineering Specialist for Renown, is the go-to person for anesthesia, heart-lung bypass, red cell saver and life support equipment. He embraces the fact that, regardless of whether you are a specialist or a generalist, there is no typical day working in this department. “Every day brings different challenges,” said Raul. “I really enjoy the mental exercises I do every day. They keep me grounded and focused.” On top of their day-to-day work and any special projects or emergencies that come up, the team is on an ongoing preventative maintenance schedule. Think of this work like your car’s oil change – routine maintenance to prevent something from breaking down in the future. “At any point, we might have 100-200 extra pieces of equipment to handle during preventative maintenance,” said Taylor Gray, a Clinical Engineering Technician for Renown. “We are always helping each other through any issues.” Our Clinical Engineering team shows exactly what it means to be collaborative. Even though their to-do lists are ever-growing, this team never feels alone. They know they can always lean on each other for support, regardless of the workload. “We always have each other’s backs,” said Taylor. “I feel so happy and satisfied in my job, and my coworkers are a large part of that.” Celebrating the Genuine Difference The Clinical Engineering department is driven by their desire to help and take care of the entire health system, and in turn, make a genuine difference for the communities we serve, from the medical staff to the patients. “The satisfaction you get in our field when we impact patients’ lives and their healing process is so motivating and engaging,” said Tony Martinez. “It’s a great feeling.” The team knows the common saying ‘Walk a mile in someone’s shoes’ very well; so well, in fact, that they take it to the next level, doing everything they can to prevent frustrations and extended down times. “We try to walk a mile in someone’s shoes before they get angry,” said Reagan Jordan, Director of Clinical Engineering for Renown. “Your satisfaction is our mission, and our team continually works to improve their outcomes every day.” This department is where the entrepreneurial spirit and science-focused mind meet. For people like Raul Hernandez, who came from a business background as well as decades of medical technology experience, Renown helps him bring both his personal and business skills into focus. “This environment is very beneficial for Renown, me, and of course, the patients,” added Raul. Being members of a team that is committed to excellence and purpose inspires them to reach new heights in patient care. “I am constantly reminded of the positive impact we have by witnessing the individual experiences we have and hearing the enthusiasm and thankfulness in their voices,” said Raul. “It gives me a great sense of pride to work at Renown.” "There is a strong feeling of mutual respect here,” added Ed Trejo, a Clinical Engineering Technician at Renown. “We are always here to help.” The proof is in the data. The Clinical Engineering team scored as one of the top departments in the recent Renown employee engagement survey, with their results sitting at more than 94 percent. “This speaks to not only our department leadership but also the team as a whole,” said Reagan. “I am extremely proud of them. Despite the pandemic, they are knocking it out of the park.” For this department, coming to Renown is easy; staying at Renown is even easier. “Staying at Renown is the easy choice,” said Raul. “And this team is only going to grow.” Workflow Whizzes and Kindness Champions “Rolling with the punches,” as Tony Martinez says, comes naturally to the Clinical Engineering team. With the constant workflow of equipment coming into the shop, every team member has learned how to be experts at prioritizing, especially based on the needs of our organization. Even though their jobs can bring a lot of intensity, this department’s positive attitude radiates throughout the hospital. Upon entering the workshop, everyone is greeted with a smile from every team member, along with an immediate willingness to dive into the complex world of engineering. “The experience of helping other people with their unique needs is invaluable,” said Taylor Gray. If this work environment sounds enticing, great news – the Clinical Engineering team is growing. Motivated, aspiring engineers with a passion for healthcare and an associate’s degree in a related field are welcome. Military experience is also valued very highly in this team. As many of our military servicemen and servicewomen gain specialized engineering experience while enlisted, the military-to-engineer career ladder at Renown is especially strong. In fact, according to Paul Joseph, a Clinical Engineering Technician at Renown, the majority of their teammates come from a military background. Above all, being capable of prioritizing on the fly, thinking critically, having an open-mined outlook and being self-driven are the top skills that this department values. As Ed Trejo states, “If you’re willing to wear different hats, you will do very well here." “Go with the flow, and expect the unexpected,” added Rylie Nickerson. Those who join this team feel at home. The warm embrace of the team’s kind nature and the supportive environment they all foster inspires an efficient workflow that helps our entire hospital system function at the top of its game. At the end of the day, everyone who joins the team, or anyone who even interacts with the team in any capacity, will be in good hands. Mandy Noriega, a Clinical Engineering Technician for Renown, closes these thoughts with a great reminder to each and every one of us: “After all, teamwork makes the dream work.”
-
What Foods to Eat and What to Avoid When Pregnant
Eating a well-balanced and nutritious diet when pregnant is one of the more essential things you can do for your baby and yourself. The basic principles of what to eat when pregnant are quite similar to how we should be eating all the time. This includes focusing on fruits, vegetables, whole grains, lean protein and healthy fats. Of course, there are a few areas that you should pay close attention to when you’re pregnant and a few foods you should avoid. We consulted Renown Health’s Caitlin Bus, RD, LD, CDE to learn more about pregnancy nutrition. Foods to Eat Regularly: Veggies Vegetables of all kinds -- and in all forms -- are beneficial for you and your baby during pregnancy. Veggies ensure your body is getting the fiber, vitamins and minerals it needs. However, fresh or frozen veggies are considered best, but if you choose to eat canned veggies, make sure you choose a low sodium product. The more greens, the better! If you have an aversion to vegetables, especially in the first trimester, try sneaking them into smoothies. Healthy Proteins Protein-rich foods support your baby's growth while giving your body the nutrients to build and repair tissues, including your muscles, hair, skin and nails. Although protein requirements vary from person to person, a pregnant woman needs additional protein for her baby's growth, especially in the second and third trimesters. Regularly eating high protein foods -- like fish, chicken, turkey, eggs, peanut butter, nuts and beans –– promotes your baby's healthy brain and heart development. Grains Food like brown rice, quinoa, whole-wheat pasta and oatmeal are great to eat while pregnant. They are rich in fiber, iron, B vitamins and folic acid, which are all beneficial to physical development. Grains also help alleviate constipation and hemorrhoids. Fruits Fruit can help satisfy any sugar cravings you have when pregnant while also supplying your baby with nutrients – it's a win-win. Some people advise against fruit consumption while pregnant, but this is a myth. Like with all foods, moderation is key. Fruit can be high in sugar, so it is important to be aware of your intake. Also, make sure you are mindful of your preparation – thoroughly rinse produce under running water for 30 seconds to help avoid foodborne illness. Pasteurized Dairy Dairy products like milk, cheese and yogurt can be great sources of protein and calcium needed for the healthy development of a baby's bones, teeth and muscles. These foods also help with ensuring healthy heart function and nerve transmission. When buying these products, make sure to choose pasteurized products to avoid exposing your body to germs and bacteria. The American College of Obstetrics and Gynecology recommends 1,000mg of calcium per day for pregnant and lactating women. This equates to 4 servings of dairy or calcium-rich foods such as leafy greens, broccoli, tofu, almonds or dried figs. DHA Omega-3 Fats Omega-3s like DHA help support the health of a baby's brain and parts of their eyes. Women who are pregnant or breastfeeding should eat at least 8 ounces and up to 12 ounces of seafood each week. Ideally, food sources that offer DHA omega-3 and that are lower in mercury should be emphasized in your diet, including fish like salmon, sardines and anchovies. If you do not eat fish or omega-3 fortified foods, a DHA omega-3 supplement is recommended. Choline Did you know that 92% of pregnant women fail to meet the daily choline recommendation? Choline is crucial for an infant's brain and central nervous system development. One egg supplies 33% of the recommended daily intake. Although choline is often absent or low in prenatal vitamins, the best food sources include eggs, meats, fish, dairy, navy beans, Brussels sprouts, broccoli and spinach. Iron and Folic Acid Iron is the most common nutrient deficiency during pregnancy. Foods with high and moderate amounts of iron include red meat, chicken, fish, fortified cereals, spinach and beans. Folic acid is used to make the extra blood your body needs during pregnancy. Consuming adequate folic acid early in pregnancy reduces the risk of birth defects that affect the spinal cord. It is recommended to consume 400 micrograms (mcg) per day for pregnant women. This amount is included in your prenatal vitamins. Water Staying hydrated is one of the best things you can do for yourself and your baby when pregnant. In addition to just being good for you, hydration alleviates morning sickness and nausea, while dehydration can lead to contractions and even pre-term labor. Aim for 10 cups of fluids per day, on top of the water naturally occurring in foods. Foods to Avoid: Raw Fish and Fish with High Mercury Content Sorry sushi fans, according to the Center for Disease Control and Prevention, pregnant women are 10 times more likely to get infected by Listeria, a bacteria found in raw or undercooked fish. Also, avoid fish often found to be high in mercury, including swordfish, king mackerel, tuna and marlin. Processed or Raw Meat Similar to eating raw fish, eating undercooked or raw meat increases your risk of infection while pregnant. Hot dogs and lunch meats should also be avoided, unless they have been reheated to be steaming hot (for example, in a microwave). Alcohol Drinking alcohol when pregnant can impact your baby’s brain development and increases your risk of premature birth, low birth weight or miscarriage. Just don’t do it! Minimize Caffeine High caffeine intake during pregnancy can restrict your baby’s growth; therefore, it is recommended that pregnant people limit their caffeine intake to less than 200 mg per day – that’s roughly two cups (16 fl oz) of coffee per day. Runny Eggs Eating raw or runny eggs when pregnant increases your risk of Salmonella, which can cause fever, nausea, vomiting, stomach cramps and diarrhea. Always make sure your eggs are cooked through or use pasteurized eggs.
Read More About What Foods to Eat and What to Avoid When Pregnant
-
Breast Feeding Doesn't Have To Mean Sore Nipples
If you think sore nipples are just a normal part of breastfeeding, think again. Robin Hollen, APRN, and Breastfeeding Medicine Specialist, says that nursing can be an enjoyable experience for mom and baby without pain and discomfort. A top concern of nursing moms within the first week after delivery is how to prevent sore nipples. Even moms who’ve nursed before struggle with this common issue. While many women think it is a regular part of the nursing experience, it is actually a sign that something isn’t quite right. “Nursing your baby should be enjoyable,” says Robin Hollen, Breastfeeding Medicine Specialist with Renown Health. For over 30 years Robin has been supporting moms to breastfeed. Below she shares some valuable information and tips, helping you create a happy and healthy breastfeeding experience for you and your baby. What causes sore nipples? The most common cause of sore nipples involves incorrect latching. For a proper latch, a baby’s mouth takes in the entire nipple and some of the breast, so that the nipple rests at the back of the mouth where the palate is soft. With an improper latch, the mouth may slip down to the tip of the nipple while the baby nurses. This constant pressure on your sensitive skin may cause discomfort and pain. A board-certified lactation consultant can help assess if your baby is latched correctly and troubleshoot your breastfeeding concerns. Less common causes of sore nipples include: • Improper tongue placement of baby • Clenching • Incorrect breast pump use How can a mother prevent sore nipples from an improper latch? Breastfeeding is a learning experience for both mom and baby. Ask for help with the latch so your baby learns it correctly and maintains its depth. In the past, new mothers were surrounded by a community of women — their own mothers, grandmothers, or other family and friends — to provide assistance and guidance with every latch at the beginning of an infant’s life. In today’s culture, new moms can find themselves on their own with no extended family to lend their knowledge. Nurses, pediatricians and lactation consultants now fill that role; they are the eyes and hands along with the much-needed experience to guide new mothers. Our Breastfeeding Medicine experts assist nursing moms with latch every day. Even a single visit with a lactation consultant observing your breastfeeding baby can provide valuable insight on achieving, and maintaining, the proper latch - preventing future nipple soreness and discomfort. How to heal sore nipples from breastfeeding To heal sore nipples, you must first fix the cause, and correcting the latch prevents further damage. A lactation consultant can also help you address the pain. Below are some breast healing tips: • Your own expressed breast milk is excellent to rub into the nipple for anti-bacterial protection. • For those moms who need more lubricant or fat than breast milk offers, use a lanolin or a cream that is labeled safe for the baby. • Soothies are a gel pads providing comfort in between feedings, but should not be used with lanolin products. • Breast shells, not to be confused with shields, can guard the nipples from irritation or pressure in between feedings. If you have more questions about preventing and healing sore nipples or general breastfeeding concerns, talk to your pediatrician or a Renown Health Breastfeeding Medicine specialist at 775-982-6365.
Read More About Breast Feeding Doesn't Have To Mean Sore Nipples
-
4 Breastfeeding Tips for New Moms
While breastfeeding is natural, it's not always easy. We asked Certified Lactation Counselor Sarah Mitchell for some tips to help make the process easier for mom and baby. From increased infant immunity to improved maternal health and well-being, the benefits of breastfeeding are many. Still, only 60 percent of U.S. moms in the United States continue to breastfeed past their baby's first six months. There are for many reasons for why moms stop, including the mother's their need to return to work. We reached out spoke to Sarah Mitchell, a certified lactation counselor at The Lactation Connection at Renown, for some expert advice. Tip 1 At first, it's normal to expect obstacles. Even in cultures where close to 100 percent of moms breastfeed, they can experience issues, including getting the baby to "latch on," sore nipples, and milk production. In addition, it sometimes can take several weeks for mom and baby to get comfortable. Tip 2 Line up a coach, even before the baby is born. This can be a professional lactation coach, family member, or friend who is experienced and encouraging. While online videos can be helpful, most new moms need the one-on-one guidance that a coach can provide. Renown offers outstanding resources in its Lactation Connection center, including expert consultants, products, and support. Tip 3 Well ahead of the due date, set up a support network of friends, family members, or community groups such as La Leche League. Women historically have relied on extended support systems to help them with raising children, and breastfeeding is one of those areas that, while natural, still needs encouragement from the women who’ve been there. Tip 4 Don’t get discouraged if you need to supplement at times with formula. This, too, as it turns out, is not uncommon in other cultures. In other parts of the world, babies are given beverages and foods such as tea, broth, soup, juice, mashed bananas, and papaya. The American Academy of Pediatrics recommends supplementation only with approved formula -- but the point is, it’s ok to supplement if you need to. Finally, don’t forget the importance of breastfeeding for connecting with your baby. It’s essential to maintain breastfeeding over the weekends, preferably “on-demand,.” and will keep that special bond strong after you have returned to your job.




.jpg?rev=ddb15541cee845129a2355ba27384fb5)





