Search
-
Department Spotlight: Surgery & Procedure Scheduling
When it comes to intimidating procedures such as surgery, cardiac catheterization (Cath) or interventional radiology (IR), there can be a lot of unknowns. What can I expect on the big day? What will happen after I’m all done? Will I have to worry about my orders not being in the system? Who can I call if I have any last-minute questions? It’s easy for your thoughts to race as you approach your procedure date, but luckily, there is a team who puts your mind at ease. With Renown Health’s Surgery & Procedure Scheduling department, patients can breathe a sigh of relief knowing that all the nitty-gritty is taken care of before they step foot in the procedure room. This team operates in the mindset of a complex Tetris board – fitting in all the pieces to make sure every patient is set on the path for surgery success. Consistent Contact Our Surgery & Procedure Scheduling team has a unique history. Initially operating as two separate teams, over the last year, our leaders skillfully combined the two teams together under one umbrella. That allows the now singular team to have line of sight across every surgery and Cath or IR procedure plan and be better stewards of the resources they have at their fingertips to provide streamlined, more-connected care for patients. As one might imagine, with the merger of the two teams, the day-in-the-life of each team member is full of a variety of crucial checklist items to cross off – all supporting constant communication from patients to providers. On the surgery scheduling front, these team members are resource rockstars. From working with referring providers to get patients scheduled appropriately to ensuring rooms and equipment are available for every patient, this team makes sure everything and everyone is in place when the time comes to help create a successful procedure and the best possible patient experience. “In surgery scheduling, we handle inbound calls for the outside offices to get time scheduled for each patient in the operating room (OR),” said Lydia Sharkey, Senior Scheduler. “We make sure there are plenty of anesthesia resources and equipment for every surgery, including any important information that we need to schedule patients appropriately and adding all documents to the OR board. If we need to swap rooms or move patients around, we handle that process too.” Over on the IR/Cath scheduling side of things, this team is on the frontlines of patient communication. They are experts in helping patients navigate their procedure from start (seeing their provider and obtaining the proper referrals) to finish (the day of the procedure and post-procedure process). “My day is a little different than the hospital schedulers; our part of the team handles the outpatient aspect,” said Adrienne White, Senior Scheduler. “We are in constant contact with patients and the IR and Cath departments. We help them navigate their procedure, including what to expect during and after the procedure. We get them through the process as easily as possible and ease their minds, so they know what is going to happen every step of the way. It’s all about communication, communication, communication!” This department has a significant overarching role: make sure all documents and ancillary information is set up for all our clinical teams that help with surgeries and procedures. This critical work means that every process is followed, and no important details are left out. “No one wakes up and says, ‘I want to have surgery;” our team goes above and beyond to make sure every single detail is taken care of so that when patients arrive, everything is in place,” said Trisha White. “Our team works hard to ensure everything runs as efficiently as possible because we want to use our resources in the best way possible to serve our patients without delays. We make sure we receive all the orders, codes and insurance and that the teams that follow after us – including our pre-admit team and nurses – have all the information they need to do their job seamlessly." With all the work they accomplish daily – not to mention how they wholeheartedly support each other through it all – it’s no question that the entire team has a lot to be proud of. Besides helping make patient care possible, the team puts their departmental merger and the move to fully remote work at the top of the list. “We’re most proud of merging the surgery scheduling and procedure scheduling teams together and therefore more cohesive,” said Mary Gray, Senior Scheduler. “The merger has made our team blossom and be able to connect with and rely on one another even more. We aren’t afraid to speak up and say something. At the end of the day, we’re here to take care of the patient, but we also help each other out. Our morale has gone up, and everybody is happier. Even though we all work remotely, we are more connected and have a great work-life balance.” “Along with transitioning the two teams into one big team, the move to being fully remote was huge," added Patricia Cruz-Hernandez, Surgical RN Scheduling Coordinator. “We worked through all the glitches, and it was a seamless transition to move into a remote setting. What’s great is that it did not affect patients at all; everything still gets done exactly as it should.” No matter how busy the days may get, Renown’s surgery and procedure schedulers always remember one thing: they are incredibly grateful for their fellow team members. “We have a very efficient and hard-working team of women,” said Pam Chapa Valencia, Senior Scheduler. “I could not have handpicked better people for our team,” added Trisha White. “I feel so lucky to have the team that we have.” A Renown “Why” Our Surgery and Procedure Scheduling team members all have diverse stories to tell about their road to Renown and why they’ve stayed in the department for as long as they have. Whether they’ve been with us for two years or two decades, they all share the same strong calling to care for their community. “I always wanted to help people, and my grandma was a nurse,” said Pam Chapa Valencia, Senior Scheduler. “I loved hearing her stories, and it made me want to be involved in patient care.” “I have a caring nature, and a hospital nature seemed like the right fit – I've been here for 25 years,” added Mary Gray. Several of our schedulers recognized the influence Renown has within our community and the ability to grow professionally and personally, both of which were a driving factor in their decision to make our health system their long-term career. “I’m originally from southern California, and I moved here about eight years ago; my husband always talked so positively about Renown, especially with how big it is and how it has the only level II trauma center in northern Nevada, so my goal was always to get a job here,” said Lydia Sharkey. “It’s been a great environment to be a part of.” “I’ve been with Renown for 17 years, and I chose to come here because of the reputation of the services Renown provided and care they gave,” added Trisha White. “I also knew what opportunities there were for me professionally, and in doing so, we are taking care of our community. I’ve had the chance to grow within my own professional skills and leadership skillset.” A profound feeling of ‘home’ is a common theme among this department. These team members appreciate the sense of community Renown has, the strides we’ve made in expanding our reach and how our health system gives healthcare professionals who are new to the field a chance to succeed. “At the time, Renown was the only hospital that would train nurses, and as a brand-new nurse, I had no experience – Renown took a chance on me,” said Patricia Cruz-Hernandez. “I feel like this is home. Our health system is so community-based and people-first minded, keeping ‘mission over margin.’ We’re growing, we’re expanding, we’re everywhere!” “I was a part of a transition as the cardiology private practice I worked with became a Renown practice, and it was great,” added Adrienne White. “This transition enabled us to provide more services and better care to patients. I stay here because I see the leaps and bounds we’ve been able to make in terms of procedures, accessibility and patient experience.” As true advocates for both patients and each other, the team is proud to have found their niche – and the ultimate beneficiaries? Everyone undergoing a surgery or procedure at Renown. A Culture of Kindness and Gratitude When you meet the Surgery & Procedure Scheduling team, you are greeted with warm smiles and an enthusiastic “Nice to meet you!” You can’t help but smile back and feel the infectious kindness they exude. Renown operates with a People-First mindset, a vision that this department especially takes to heart. They emulate the exact definition of our “Collaboration” cultural commitment. “We’ve built very good relationships and rapport with the OR managers and board runners,” said Lydia Sharkey. “The communication that we have at all three locations is very solid.” “The OR leadership is always so willing to help out whenever they can, and the resources they’ve provided have been huge for us,” added Adrienne White. “All the teams that see the patients after us – especially the surgical pre-admit team and the case managers, are fantastic about collaborating with us and reaching out to solve any issues they may have,” added Trisha White. “We all work so well together, especially since we all impact patient care.” In any organization, strong and compassionate leadership is key to a thriving team. Luckily for our surgery and procedure schedulers, they have Trisha White on their side. They attribute a lot of their success to having a supportive leader who “gets it.” “Trisha has been a scheduler like us, so she completely understands when we’re having an issue, because she’s struggled with the same thing and knows where we are coming from,” said Mary Gray. “It makes us feel like we are not alone – I can always reach out to her, or any of my other coworkers, to ask questions and figure out a solution together.” Despite being a remote-only team that meets in-person only one or two times a month, this group never misses an opportunity to reconnect both online and offline. They frequently shout out their Culture Ambassadors, schedulers Pam Chapa Valencia and Roxanne Abundis, for their team’s high morale. “Even though we all primarily work remotely, our in-person days are some of my favorite days of the month,” said Trisha White. “We feel so uplifted, we laugh and we have fun. We love being with each other. Pam and Roxanne are our Culture Ambassadors, and they both have been amazing at planning fun things for our teams. They go above and beyond to make our team feel cohesive and included.” “Pam and Roxanne have been leaders in creating a fun environment and supportive culture for us,” added Lydia Sharkey. “Whether it’s creating care packages or making sure we all have a good time when we see each other in person, they deserve a lot of credit.” As this team excels in their roles and foster a culture rooted in kindness and gratitude, we can trust that Renown’s surgeries and procedures will continue to thrive, and patients will continue to benefit from their diligent efforts and commitment to efficiency. “We make the magic happen!” closes Mary Gray.
Read More About Department Spotlight: Surgery & Procedure Scheduling
-
Motivating Kids to Eat Healthy Foods
Do you have a picky eater in your household? Or maybe you've got a snack monster who’s all about chips and candy? We're here to share a few fun strategies to motivate your little superheroes to snack on healthy foods instead! Rainbow Power-Up Eating a rainbow isn't just for unicorns! Different colors mean different powers: Red foods like strawberries and tomatoes help your heart. Orange foods like carrots and sweet potatoes help your eyes spot things like an eagle! Green foods like spinach and broccoli help you grow super strong bones. So, create a plate with as many colors as possible. The more colors, the more powers! Super Smoothies Blend your favorite fruits, such as bananas, berries and mangoes. Add some milk or yogurt and a handful of spinach. Your kids won't taste the spinach, and they'll drink a supercharged smoothie that gives them the energy to tackle any challenge. Create a Parfait Packed with Delicious Layers! Veggie Villans Who said veggies can't be fun? Turn them into heroes by giving them cool names and fun shapes. Make carrot sticks "Captain Crunch" or broccoli florets "Broc the Rock." Dip them in hummus or peanut butter for an extra flavor kick. Snack Attack Plates Create snack plates that are as fun as they are nutritious. Combine: Cheese cubes Grapes or apple slices Nuts or seeds Whole-grain crackers Mix and match these for your perfect plate! Make Your Own Trail Mix Fuel-Up Challenges Challenge your kids to eat three different healthy foods each day. Turn it into a family game to see who can eat the most colors or try the most fruits and veggies. You can even draw up a "super snacks" chart to keep track of your progress. Final Super Tip! Even superheroes have cheat days. Don't worry if your family doesn't eat healthy every meal. Just aim to eat more of the good stuff than the not-so-great stuff. Your kid's bodies will reward them with tremendous energy, focus and strength.
-
Make Your Own Trail Mix: 4 Quick and Easy Recipes
Craving a crunchy, sweet, and nutritious snack? Try making your own trail mix! Perfect blends of nuts, dried fruits, and a touch of chocolate can be whipped up using bulk bin ingredients or pantry staples. Enjoy this delicious, healthy snack on a hike, at the office, or on your next road trip through Nevada's scenic deserts.
Read More About Make Your Own Trail Mix: 4 Quick and Easy Recipes
-
Nourishing Your Loved One Through Cancer Treatment
Eating healthy is a daily challenge for many, but for those with cancer, it is an even harder struggle. A cancer diagnosis affects not only those diagnosed but family members and friends, too. One key area of concern is making sure your loved one stays well by eating healthy food every day. Here are some vital cancer nutrition tips from Jessica Blauenstein, a Board Certified Specialist in Oncology Nutrition and Registered Dietitian at Renown Health. Help to Prepare Meals and Snacks for Daily Cancer Nutrition Make it grab and go. Easy-to-make meals help reduce the burden of having to cook and prepare food. Having easy to grab snacks on the counter or in the fridge can help ensure your loved one has access to those nutrients when needed. Sit outside of the kitchen. This allows your loved one to avoid cooking smells which can make them feel sick as a side effect of cancer treatments. Also try serving them cold foods such as sandwiches, cheese and crackers, or shakes which have a mild scent. Try drinkable meals. Some people with cancer find it easier to sip their calories over the course of 30 minutes to an hour. Consider smoothies or supplemental shakes such as Ensure Complete, Fairlife shakes, Orgain shakes, or Boost Plus to name a few. A great foundation for a smoothie is a protein source (Greek yogurt, protein powder, nut butters or milk) with a carbohydrate (fruits, juice or berries). Add other ingredients as desired, such as spinach, kale, and ground flaxseed or chia seeds to give it more vitamins, minerals, and fiber. Snack Ideas for Those Undergoing Cancer Treatment The following ideas are both quick and easy to make for your loved one. Chicken or tuna salad with whole grain crackers or as a sandwich on whole grain bread Greek yogurt mixed with cereal, fruit and/or nuts Cottage cheese with banana, cinnamon and/or peanut butter Favorite fruit with 100% natural peanut or almond butter spread - Try peanut butter with bananas, apples, or even celery Their favorite veggies dipped in a salad dressing of your choice - For example, carrots with hummus, tahini, or ranch dressing Cheese and whole grain crackers - Add tomato slices with a small amount of avocado, and a dash of oregano on top for more flavor Eggs scrambled with cheese, vegetables and/or salsa Peanut butter and jelly sandwich on whole grain bread A baked sweet potato with some favorite toppings Hard boiled eggs and/or egg salad with whole grain crackers, or as a sandwich on whole grain bread Oatmeal or cream of wheat prepared with milk, fruit and/or nuts Sometimes your loved one may not feel like eating or refuse to eat. If treatment side effects are impacting your loved one’s ability to eat, please visit the websites below containing recipes tailored to treat side effects. Cook for Your Life ELLICSR Of course, you may also consult a registered dietitian and/or the patients care team, if you have more cancer nutrition concerns.
Read More About Nourishing Your Loved One Through Cancer Treatment
-
Department Spotlight: Pharmacy
When it comes to each patient’s healthcare journey, medication is often a key chapter. After all, medication is one of the most common treatment methods to help patients on the road back to health. In 2023, 4.83 billion prescriptions were filled in the U.S., and with this number only anticipated to rise annually, having an expert pharmacy team on your side to make certain you are prescribed the ideal dosage to treat your condition, prepare your prescriptions on time and help you manage your medications responsibly is important. Fortunately, at Renown Health, we have best-in-class inpatient and outpatient pharmacy teams to fill both prescriptions and promises for excellent care. Renown Pharmacy plays a vital role in helping us foster a health system that prioritizes patient well-being above all else. This department exemplifies the impact that a unified, expert pharmacy team can have on patient outcomes now and in the future. The Masters of Medication Spanning three hospitals plus ambulatory locations across the health system, Renown’s growing pharmacy team – full of dedicated pharmacists, pharmacy technicians and even medical assistants – manages medications in a wide variety of patient settings, touching nearly every aspect of the healthcare continuum: Outpatient Retail Pharmacies Renown Regional Medical Center – 75 Pringle Way The Healthcare Center – 21 Locust Street Renown South Meadows Medical Center – 10101 Double R Blvd Inpatient Pharmacies Renown Rehabilitation Hospital Renown Regional Medical Center (including Renown Children’s Hospital) Renown South Meadows Medical Center COMING SOON: Conrad Breast Center Pharmacy (in honor of Kristina Ferrari) in the Specialty Care Center at Renown South Meadows Ambulatory Pharmacies Anticoagulation Services – Institute for Heart & Vascular Health (IHVH) Pharmacotherapy Program – IHVH and Renown Medical Group Locations Congestive Heart Failure Pharmacotherapy Program – Center for Advanced Medicine B at Renown Regional Chronic Obstructive Pulmonary Disease (COPD) Pharmacotherapy Program – Renown South Meadows Endocrinology Pharmacotherapy Program – Renown South Meadows Additional Pharmacy Programs Medical Reconciliation Pharmacy Residency Clinical pharmacists at Renown bridge the gap between medicine and compassionate support, making sure each patient receives personalized care one prescription at a time. “There are various roles pharmacists play within Renown,” said Clarissa Munoz, Clinical Pharmacist in the Renown Regional Inpatient Pharmacy. “Staff pharmacists work diligently to ensure correct medications are dispensed, and if compounded, make sure they were prepared properly. They also work hard to answer medication messages and phone calls, help verify orders and make sure ode trays/RSI kits are appropriately stocked and ready when needed. Clinical pharmacists work from satellite pharmacies on the floor and focus on reviewing patient charts and aim to provide additional interventions to the providers to optimize treatment strategies. We also serve as a resource for nursing staff and help answer medication questions.” “My role in the pharmacy is pretty expansive,” added Chanelle Ajimura, Clinical Pharmacist in the Renown Regional Outpatient Pharmacy. “I maintain inventory to confirm patients can receive their medications in a timely manner both for our discharge and retail patients while balancing the Meds to Beds program, which offers medication delivery to the bedside and bedside medication counseling; collaborating with an interdisciplinary team to find the most affordable price for patients; and verifying that the dose, strength, indication, etc. is appropriate for the patient from start to finish.” “In the pharmacy, I make sure patients are receiving appropriate drug therapy by checking for major drug interactions and ensuring appropriate dosing,” added Courtney Church, Clinical Pharmacist in the Renown Regional Outpatient Pharmacy. “I also make recommendations to providers so patients can get cost-effective therapy.” Our pharmacy technicians work behind-the-scenes ensuring efficient medication management, making a difference in the lives of patients every day. “A pharmacy technician is responsible for making sure the patient gets their medications on time and at the lowest price possible,” said Nate Graham, Pharmacy Technician in the Renown Regional Outpatient Pharmacy. “This is done by working with patients, insurance companies and case workers. We fill prescriptions, enter prescriptions into our system, receive and send orders for medications and maintain a clean pharmacy with an accurate inventory.” “We do a variety of things; the task people probably know the most is counting out the medications and putting them in the amber vials,” added Rachel Vallin, Pharmacy Technician in the Renown Regional Outpatient Pharmacy. “We also help patients at the front of the pharmacy, ring out their prescriptions, answer some basic questions (deferring to a pharmacist as necessary) and billing insurance. Meds to Beds is my favorite part because I feel the most involved. I take medications to patients who are discharging up to their hospital rooms so they have it with them when they leave.” “As a technician, I confirm that all medications of new admissions are available in our machines prior to admitting and then maintain stock during each patient’s stay,” added Tammara Axtman, Pharmacy Technician at Renown Rehabilitation Hospital. "I also assist our nurses when needed in regard to any of their questions with both EPIC and Omnicell.” Our pharmacy team is also on the move all across our health system, thanks to our Ambulatory Pharmacy programs. For patients experiencing a serious heart, lung, or endocrine condition that requires ongoing drug therapy maintenance and guidance, our ambulatory pharmacies step in to carefully monitor how their medications impact their health and well-being. “Our role as pharmacists in this department is non-traditional because we actually see patients in the exam rooms face-to-face,” said Cory Lankford, Ambulatory Care Clinical Pharmacist for Renown’s Anticoagulation Services. “We modify their medication regimens and drug recommendations under collaborative practice agreements.” “Because our role is so unique, we have a lot of opportunities to make a positive impact on patients,” added Janeen Abe, Ambulatory Care Clinical Pharmacist for Renown’s Anticoagulation Services. “We do a lot of direct patient interaction, including counseling patients on their medications and helping them navigate through their disease state.” “As a medical assistant in this department, we’re called the patient ‘liaisons’ to orchestrate who they should go to whether it’s a nurse, a provider or a pharmacist,” added Kiara Scruggs, Medical Assistant for Renown’s Anticoagulation Services. “We look at each patient’s medications and help with the Warfarin blood thinner monitor. We get to do a lot with patients." A key resource within the Pharmacy department and the emergency admission process, our Medical Reconciliation ("Med Rec") team stays on top of each patient's medication records. By ensuring each medication regimen is accurately reflected in each patient's chart and that patients continue to take their at-home medications while admitted to the hospital, this team provides vital insight into medications that could be a contributing factor to each patient's symptoms, including drug interactions. “Our medication reconciliation pharmacy technician team are true detectives,” said Heather Townsend, Clinical Pharmacy Supervisor. “When a patient arrives to the hospital, Med Rec works with patients, families, caregivers and outpatient pharmacies to compile a list of medications the patient has been taking a home. This list is used to make sure medications are not contributing to the patient’s symptoms and to assure medications are continued throughout the hospital stay. The addition of the medication reconciliation team has been one of the greatest advancements in medication safety.” “As a Med Rec Tech, we interview patients and family members and call pharmacies, skilled nursing facilities, etc. to obtain an accurate and complete medication list/history to outline what the patient is currently taking on a daily basis,” added Kara McGee, Medical Reconciliation Pharmacy Technician. “We make sure that we document the correct medication, dose, route, frequency and directions. This information is crucial because the nurses, pharmacists and physicians look at our work to figure out if any medications are contributing to the patient's health condition, and for the continuation of home medications on admission.” “Even though the Med Rec Tech might seem small in the hospital realm, it is very vital for patient information and beneficial to the patient's health,” added Brizza Villafan, Medical Reconciliation Pharmacy Technician. “There is never a dull moment in this work.” No matter the diagnosis, having Renown Pharmacy as an integral part of your healthcare team is a win-win situation for both you and them: you receive access to medication to help you heal, delivered to you with precision and care, and the pharmacy team has the opportunity to care for you and make a positive impact, a role they take seriously.
-
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
Celebrating Blood Sugar Balance This Holiday Season
As the holiday season draws near, we find more reasons to celebrate with loved ones. At Renown Health, we are kicking off the celebrations early this November with American Diabetes Month. Approximately 37 million Americans, including 270,000 Nevadans, have been diagnosed with diabetes with as many as 95% of those diagnosed living with type 2 diabetes mellitus (T2DM). What is Type 2 Diabetes? Type 2 diabetes is a chronic health condition that occurs because your body is not using insulin (a hormone made by the pancreas to help cells use the food we eat for energy) as well as it should, resulting in high blood sugar levels. It is important to obtain a diagnosis for T2DM and ensure it is well-controlled to prevent serious health complications. Those with diabetes are at higher risk for blindness, kidney failure, heart disease, stroke and amputation. Tips for Supporting Your Health with Type 2 Diabetes Know Your Blood Sugar Levels: Work with your healthcare provider to establish target blood sugar levels, and make sure to monitor your levels regularly as advised by your healthcare provider to prevent or delay health complications associated with T2DM. Focus on Your Plate: Eating foods such as fruits and vegetables, lean meats or plant-based proteins, healthy fats and whole grains supports diabetes management. If choosing healthy foods is difficult due to your busy schedule, cost or simply because you aren’t sure where to start, talk with your healthcare provider who may refer you to a registered dietitian. Registered dietitian nutritionists are certified nutrition specialists who can provide education and practical tips for eating to support your T2DM diagnosis with visits covered by many insurance plans. Prioritize Staying Active: Engaging in regular exercise is good for everyone, especially those living with T2DM. Exercise helps your cells become more sensitive to insulin and therefore supports healthy blood sugar levels. Always check with your healthcare provider prior to beginning a new exercise plan. Support Stress Reduction: Stress is unavoidable but can be managed through regular exercise, getting enough quality sleep (7-8 uninterrupted hours per night) and practicing meditation and other mindfulness techniques. Plan Ahead for Holiday Gatherings: There’s still room for celebration while focusing on blood sugar management. Consider bringing a healthy dish to your gathering, focus on filling your plate with vegetable sides and eating those first and incorporate a family walk after dinner. If traveling, pack nutritious snacks that support your health and keep you full. Lastly, enjoy the special dishes and desserts this season has to offer in single-serving portions.
Read More About Celebrating Blood Sugar Balance This Holiday Season
-
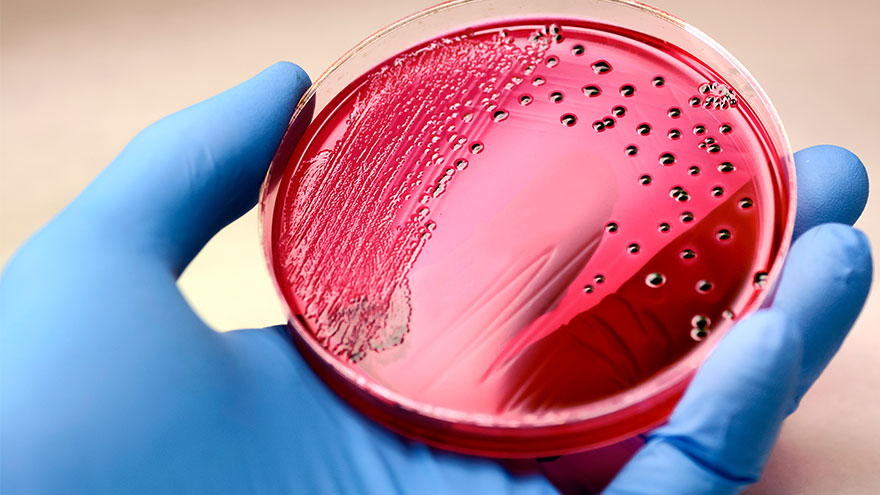
Sepsis: Causes & Symptoms
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.
-
Department Spotlight: Respiratory Care
This Department Spotlight is dedicated to Jason Simpson, Manager of Respiratory Services at Renown Children’s Hospital. Take a moment to breathe deeply. Inhale in, exhale out. We rely on our lungs to provide us with the air we need to live a healthy life – and this essential bodily function is something that many of us don’t think twice about since it comes easily for us. Now, imagine yourself as someone who is living with severe asthma, chronic obstructive pulmonary disease (COPD) or someone who was recently diagnosed with a frightening respiratory condition like COVID-19 or pneumonia. The simple act of breathing can prove to be an intimidating venture requiring the care of a professional. Who are the people that take on the challenge? Meet Renown Health’s Respiratory Care Services department. Serving patients across 13 service lines, three acute facilities, outpatient locations and telehealth, our respiratory specialists – including respiratory therapists, respiratory care aides, inpatient COPD respiratory therapy navigators and educators and more – use their expertise to help restore the vitality of all their patients with every inhale and exhale, shaping a healthier livelihood one lung at a time. The Guardians of Respiratory Wellness Whether they are managing lifelong respiratory conditions or offering crucial support in emergencies, the Respiratory Care team strives to enhance the quality of life for every patient. As an indispensable member of the clinical team at Renown, our respiratory therapists work collaboratively with doctors and nurses to tackle a wide range of tasks, tailoring care for each patient’s unique needs. “Respiratory care is involved with all stages of life, from beginning to end,” said Sarah Kurtz, Respiratory Therapist. “We work closely with nurses and doctors and perform arterial punctures, breathing treatments, weaning maneuvers for patients on life support, intubations and much more. We assess patients constantly to see if their care needs to be upgraded or if they can be weaned to get them back home with their families.” “You start your morning researching your assigned patients,” added Tim Start, Respiratory Specialist. “We go over lab values and chest radiographs and decide the best plan of care for each patient. Our objective is to improve their respiratory status by giving them medications and doing breathing exercises. We participate in other forms of care with nurses, such as activities of daily living (ADLs) and mobilization. We work as a team, and that enables us to provide great patient care.” For patients living with COPD, enjoying all that life has to offer comes with a separate set of obstacles. According to the Centers for Disease Control and Prevention (CDC), over 200,000 people across the Silver State are living with this chronic condition. Luckily for them, Renown has a specialized team to help these patients optimize their life and manage their condition with individualized treatment and education. “We run a report every morning to identify all the patients currently admitted who have a history of COPD, take respiratory medications or smoke,” said Amber Beck, Inpatient COPD RT Navigator. “After looking through their charts, we visit with the patient (and possibly their family) at the bedside to help them better understand how to manage their breathing issues.” As a vital part of the Respiratory Care team, Renown’s respiratory care aides help ensure the seamless operation of our respiratory care services. These dedicated professionals provide essential support to respiratory therapists not only during intricate procedures but also outside of face-to-face patient care by transporting equipment, restocking supplies, assisting in the mobilization of patients and more. “We are responsible for the maintenance of unit supplies and making decisions regarding levels of stock to be maintained,” said Dia Ramos, Respiratory Care Aide. “We also transport equipment, refill the oxygen tanks on the floors and intensive care units (ICUs), order and stock respiratory care supplies, mobilize patients and assist the respiratory therapists during bronchoscopies in the ICUs. In addition, we clean respiratory equipment like mechanical ventilators, continuous positive airway pressure (CPAP) and bilateral positive airway pressure (BiPAP) machines, high flows and aerosol poles.” Once the COVID-19 pandemic hit, a special spotlight shined upon respiratory care teams across the country for the heroic care they provided patients in respiratory distress. While their roles in health systems have gained a better understanding nationwide, this team understands it is vital for them to educate the community about the important jobs they hold for our patients. “Respiratory care can be under the radar,” said Pam Umek, Respiratory Specialist. “Once, when I told someone that I am a Respiratory Therapist, they said, ‘Oh, like a yoga breathing instructor?’ I then explained all the things we do: intubation, extubation, bronchoscopies, transports, traumas, codes, rapid responses, pediatrics/NICU, breathing medications/therapies, open heart rapid ventilator weaning … needless to say, that individual walked away with a better understanding of not just Respiratory Care Services but also the enormous effort it takes to care for our community.” The accolades and achievements continue to pour in, from national awards and certifications to implementing different jobs in care units to optimize the patient care experience. “We have earned and continue to maintain the Joint Commission Disease-Specific Certification for COPD,” said Amber Beck. “We are well below national averages for 30-day readmissions, lengths of stay and mortality due to COPD. Sandy, one of our COPD Coordinators, was a recipient of a patient advocacy award from the American Association of Respiratory Care and FACES Foundation.” “We have started implementing Respiratory Care Aides in the critical units, starting with the Cardiac ICU,” added Dia Ramos. “We work as one team and are always helping each other with their tasks.” Education and mentorship are at the core of Renown’s mission to make a genuine difference in the health and well-being of every patient. Nurturing the next generation of medical professionals – including respiratory care professionals – is a task that the Respiratory Care team takes seriously. “It has been great being able to help educate students in different disciplines,” added Pam Umek. “We have been able to offer shadow shifts to students in emergency medical services (EMS), nursing and medical school. These opportunities help students entering the medical field have a better understanding of the many ways we can help care for our respiratory patients.” From the moment of birth to the final stages of life, Renown is fortunate to have a Respiratory Care team that tirelessly ensures every breath counts, safeguarding their role as a trusted partner within our health system. A Tribute to Jason Simpson, Healthcare Hero
-
Department Spotlight: Renown Transfer and Operations Center
Stepping into the Renown Transfer and Operations Center (RTOC) means stepping into a transformative hub of excellence where lives are saved and healthcare is reimagined. As a cornerstone of Renown Health's commitment to exceptional patient care, the RTOC serves as a dynamic nerve center that seamlessly coordinates medical resources, ambulance rides, hospital bed space, remote home systems, hospital transfers and emergency preparedness. In this best-in-class facility, the boundaries of what is possible in healthcare are constantly pushed, and new horizons of patient care are discovered. Staffed with a dedicated team of skilled professionals, the RTOC harnesses the power of advanced technology and compassionate expertise to ensure that patients receive the highest level of care and support, no matter where they are. Through a synchronized network of communication, coordination, and compassionate care, the RTOC team ensures that patients receive the critical support they need when it matters most, working tirelessly to redefine what it means to deliver world-class healthcare. A National Standard Charged with the goal of overseeing the placement and transportation for every patient, the RTOC officially launched in 2021 as northern Nevada’s first and only transfer center of its kind and a nationally celebrated facility. As Renown’s highly coordinated care logistics system, this team uses the cutting-edge technology at their fingertips to customize healthcare to the needs of every patient, manage patient flow and drive healthcare innovation. “Compared to where we’ve started to where we are now, it’s a 180-degree difference,” said Kelli McDonnell, Manager of RTOC. “When we first started building our facility right before the pandemic happened, we took what was six conference rooms and classrooms and turned it into a command center that organizations across the country admire and come to Reno to see what we do. Mel Morris, the Director of RTOC, was recruited exclusively to build our facility with her history of building successful hospital command centers. Many people didn’t realize what a transfer center was or that Renown was the only center in the region – and we only continue to grow.” This best-in-class facility, and the masterful team behind it, handles: Coordinating all incoming patients transferred from neighboring hospitals and 27 counties across northern Nevada, Lake Tahoe, northeast California and neighboring states. Matching patients to the most appropriate bed placement using diagnostic, triage and Epic electronic medical record clinical information in conjunction with medical staff expertise to outline a plan of care that determines the best bed assignment given the patient’s needs. Coordinating video-enabled Telehealth monitoring capabilities for Renown’s four Intensive Care Units (ICUs), as well as Renown patient Telehealth and virtual visits. Monitoring Remote Home systems with Masimo during the COVID-19 pandemic, where some patients received hospital-level care in the comfort of their own homes while Renown clinicians monitored and evaluated their data and plan of care. Serving emergency and disaster management for area hospitals, first-responders and the community with local, regional and statewide emergency and disaster management for sudden-onset emergencies. The RTOC is home to many different critical roles for our health system, including Transfer Center Nurses, Ride Line Coordinators, RTOC Coordinators and more, many duties of which each team member cross-trains on to be able to fill in whenever needed. While their roles may differ, their commitment to their patients remains the same – and they all work together to achieve the same outcome: delivering the right care, at the right time and place. “As an RTOC Coordinator, we do a variety of different things,” said Anna Schaffer, RTOC Coordinator. “We do triage coordination to help our nurses and hospitalists get patients in the emergency department admitted, and we also do bed control to find patients appropriate bed placement. Communication is important, so we always make sure to stay closely connected with the charge nurses on those floors.” “We start with a basic ‘need to know’ and place patients accordingly,” added Karly Brown, RTOC Coordinator. “We get surgery numbers, ICU capacity and discharges and find beds for all patients as quickly as possible. We have the advantage of being able to see the entire hospital.” “I primarily schedule transportation for patients at the hospital who are either going home or going to a skilled nursing facility,” said Sarah Clark, Ride Line Coordinator. “I get requests from case managers to schedule rides, and I work with REMSA and other ambulance services to schedule them. It relies a lot on appropriate and efficient communication and critical thinking.” Patients in facilities across northern Nevada and northeastern California, especially the rural communities, look to the RTOC to help guide ambulances, bed coordinators and hospital staff in finding care for our rural patients. “As a transfer center nurse, I facilitate incoming patients from rural facilities in Nevada and surrounding areas in California,” added Meg Myles, Transfer Center Nurse Specialist. “There are days we may take up to 30 direct admissions from these areas.” “We are the point of contact for inter-facility transfers, whether we are sending patients out or bringing them into Renown,” said Lisa Lac, Transfer Center Nurse Specialist. “We take phone calls from those rural areas, identify what services are needed, connect them to the appropriate provider and coordinate any transfers.” “Simply put, we are the bed wizards,” said Addison Rittenhouse, RTOC Coordinator. The RTOC team continues to break barriers and push the boundaries of medical excellence through leveraging the technology at their fingertips and their unwavering dedication to the health of our community. Inspiring a new era of medical possibilities, these team members have achieved a multitude of accomplishments for both their department and their patients since the birth of the center. “We have significantly reduced the time it takes to get patient admit orders in, thanks in part to the new Triage Coordinator role, and we provide easier access for patients to transfer to us from other facilities,” said Beth Rios, RTOC Coordinator. “We have taken a bigger role in helping the smaller hospitals in our area in caring for patients and improve patient throughput.” “As a team, we’ve done a lot of work in creating an engaging and positive environment, and our internal morale committee has been a huge help with that,” said Kelli McDonnell. “We’ve been working tremendously over the last year and taking all the feedback that we received from the Employee Engagement Survey to make improvements. We had 100 percent survey participation within five days, which is incredible.” “I am so proud of our escalation and problem-solving skills,” said Becca Dietrich, RTOC Coordinator. “When an issue is raised to us, we will always find a timely solution on our end so our care teams can focus on the issue in front of them. We are the eyes in the sky, seeing movement everywhere.” Each day in the life of our RTOC team members is a testament to their commitment, resilience and timework, making a profound impact on countless lives.
Read More About Department Spotlight: Renown Transfer and Operations Center
-
Living with COPD? How to Maximize Your Summer Experience
June offers an official welcome to summer and the height of outdoor activities in northern Nevada such as hiking, camping, days spent at the lake and embracing long days and warm evenings with friends and family. Enjoying all that the summer season has to offer may not be as easy for those living with chronic obstructive pulmonary disease, or COPD, which effects more than 15 million Americans. What is COPD? COPD is a group of lung diseases including emphysema and chronic bronchitis that result in airflow blockages from the lungs. People may experience frequent coughing and shortness of breath among other symptoms. COPD typically impacts adults ages 65 and older and is becoming increasingly more common among women. Although smoking plays a key role in the development of COPD, air pollution and indoor air quality, and respiratory infection also contribute to disease development. While there is no cure for COPD, limiting progression of disease and managing symptoms can be achieved through lifestyle changes, therapy, and medications. Tips for Living with COPD This Summer, and Always Stay Hydrated: Staying hydrated is extremely important for people with COPD, especially during the summer. Not drinking enough water can make breathing more difficult because it increases respiratory symptoms. Make sure to always keep a water bottle with you and aim to drink 8-10 glasses of water daily. Be Mindful of Temperature: COPD symptoms can be exacerbated by hot weather. It is best to participate in outdoor activities during the cooler times of day, like the morning or evening. Check Air Quality Before You Go: Before engaging in outdoor activities, be sure to check the air quality index and plan your activities accordingly. Pace Yourself: Exercising can be difficult for people who have COPD. To make the most of your summer, try not to push yourself too hard and take breaks when you need them. If you start to feel out of breath or tired, take a break in a cool, shaded area until you feel better. Take Matters Into Your Own Hands To address the needs of community members living with COPD, the Renown Health Research Office has teamed up with Pulmonary Medicine to provide patients who are former or current smokers and have a history of frequent exacerbations with an option to participate in the ARNASA study. "COPD exacerbations have a huge negative impact on patient’s lung function” states Dr. Farah Madhani-Lovely, Chief of Pulmonary Medicine at Renown Health and Assistant Dean of Clinical Research at the University of Nevada, Reno School of Medicine. “We have had inhalers and prednisone for decades but patients are still having exacerbations. Now we have a new pathway we think will prevent exacerbations which is what this clinical trial is designed to prove.” This study will evaluate the efficacy and safety of astegolimab compared with placebo in participants 40-80 years of age with COPD. “This study in particular is so exciting because of the enthusiasm from the sponsor’s end” says Katie Buckley, Lead Clinical Research Coordinator working on pulmonology studies at Renown’s Clinical Research Office. “Often times sites aren’t assigned particularly passionate or engaged personnel who aid in carrying out these studies, but you can tell Roche Genentech’s team truly cares about the success of the study, the safety of their participants, and proving the efficacy of the investigational agent. Working on a study like this takes a village, and when the individuals on all ends share similar mindsets and work towards success as a collective unit instead of as individual moving parts, it’s amazing to see everything we’re able to accomplish.” Renown’s team of expert pulmonologists and researchers are available to join patients with COPD in support of their healthcare journey. If you are interested in learning more about this clinical trial option at Renown Health, talk to your pulmonologist at your next appointment or contact us at 775-982-3646. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
Read More About Living with COPD? How to Maximize Your Summer Experience
-
Multiple Sclerosis Research Opportunities in Northern Nevada
There are nearly 1 million adults living with MS in the United States alone. For comparison, that is roughly the entire population of the Reno/Sparks and Las Vegas areas combined. MS is a neurological autoimmune condition which means that the immune system of patients with MS attacks the body’s myelin, a protective substance that covers your nerves. When this happens, the unprotected nerves can be damaged. Patients with MS may experience many different symptoms ranging from mild to severe, such as mobility and vision problems, fatigue and difficulty thinking. MS is usually diagnosed between the ages of 20-50, but late onset MS can occur in patients over 50 years old. While there is no cure for MS, there are effective treatments that can help reduce the burden of patients’ symptoms and create a positive quality of life. At Renown Health, we have joined the fight against MS through a partnership between advanced neurology programs and providers and our research office. We are proud to offer newly diagnosed MS patients the opportunity to choose between standard care treatment options or participating in an open label clinical trial, the AGNOS study. This study is assessing the impact of a new medication, ofatumumab, as the first disease modifying therapy participants receive for managing relapsing remitting MS, the most common form of MS.
Read More About Multiple Sclerosis Research Opportunities in Northern Nevada