Search
-
Why I Give: Tami and Richard's Story
If you have the chance to meet Tami and Richard Dethmers, you will quickly discover a remarkable couple who embody a heartwarming spirit. Married for 44 years, they cherish family above all else. With five children and 10 grandchildren, their family is not just their priority—it's their whole world. It is this love and their steadfast faith that led Tami and Richard to make a transformative donation to Renown Children’s Hospital. The Heart of Giving In 2023, Tami toured the construction of the new Wilbur D. May Neonatal Intensive Care Unit and Pediatric Intensive Care Unit at Renown Children's Hospital. She was touched by the idea of creating a special place for sick children and their families. That night, she talked with Richard about how they could help. Together, they both agreed to make a generous donation that could help ease the pain for families with children in the hospital. A Comforting Consultation Room Their donation established a consultation room in the Wilbur D. May NICU and PICU at Renown Children's Hospital. Tami and Richard's motivation stems from personal experience, having seen their grandson endure four open-heart surgeries. "I remember challenging conversations with doctors, surrounded by other families in the open PICU. It was difficult,” said Tami. In this new consultation room, families have a private space to learn about the next steps in their journey, gaining insights into the illnesses affecting their children. It is a dedicated space where doctors can discuss treatment plans and medical information with families. Designed to be a supportive and calming environment, the room features art on the walls, and a window bathes the space in beautiful, natural light, offering comfort to families in need. Tami and Richard’s donation ensures that families in the NICU and PICU can navigate difficult conversations with doctors in a thoughtfully designed space. Because We Love You and We Care In the new consultation room, a powerful message is printed and framed: 'Because we love you and we care.' This phrase is an important part of Tami and Richard’s donation, reflecting words they spoke to their children while they were growing up. For them, it symbolizes love, care, and a commitment to offering support. A Legacy of Comfort Tami and Richard, along with their family, are dedicated to an ongoing legacy of giving. Together, they also donated blankets to patients and families who use the consultation room. “I hope they provide an added layer of comfort,” said Tami. Each blanket includes a custom tag repeating those same words 'Because we love you and we care.' Richard echoes Tami's sentiments. “We do what we can because we love children, and there is no greater pain than a child in distress,” Richard said, emphasizing their shared dedication to helping children in need. Together, with their children and grandchildren, they continue to make a difference, embodying the power of compassion and generosity in their family's legacy.
-
The Impactful Role of Renown Health Foundation's Board of Directors
Above: Brian Cushard (left), Renown Health Foundation Board Chair, with his family At Renown Health Foundation, our mission is simple yet powerful – to raise funds that support Renown Health, the largest not-for-profit health system in northern Nevada. We are the driving force behind initiatives that bring state-of-the-art equipment, conduct groundbreaking research, enhance healthcare services, improve patient outcomes and contribute to the overall well-being of our community. Our Dedicated Board of Directors Our impactful work would not be possible without our Board of Directors – a fantastic team of 27 local volunteers. They bring diverse skills to the table, working together to create positive changes in healthcare for northern Nevada. Our board is at the core of our Foundation's success by guiding important decisions, sharing valuable insights and actively engaging in community relationships. Meet Brian Cushard – Renown Health Foundation’s Chair Brian Cushard took on the role of Foundation Board Chair at the beginning of 2024. Brian, who is the President of LP Insurance Services in Reno, will lead us for the next two years, bringing a wealth of experience and a deep commitment to community well-being. Since joining Renown Health Foundation’s Board in 2018, Brian has been instrumental in shaping our strategic direction. Brian’s Vision: Advocating for Renown Health’s Mission and Making a Difference We had the opportunity to sit down with Brian and explore his passion for healthcare philanthropy and the positive changes he envisions. Brian's 'why' is firmly rooted in the belief that a robust health system serves as the backbone of the community. His vision extends beyond fundraising; it's about inspiring the community by sharing remarkable stories of care and championing Renown's impactful contributions. Q: Why does Renown's mission matter to you, and how do you see your role making a difference? A: Renown's mission matters deeply to me because, without a highly functioning healthcare system, the economic structure of the community can be impacted. At LP Insurance, where I work, we see ourselves as guardians of our clients' hopes and dreams. This translates to my role on the Board as stewards for the health of others. Advocating for a highly functioning health system is crucial in supporting community members and clients alike. Surrounding ourselves with a solid network is essential. As advocates, our voices are integral in ensuring that everyone's voices are heard. Q: Can you share a moment that made you want to support healthcare causes? A: There are those stop-in-your-tracks healthcare moments that make you reassess life's priorities. I've had moments where life comes to a standstill, and what you once thought was important takes a backseat to the basics of life—getting better, one step at a time. In those vulnerable moments, you realize the importance of every person at the hospital. In desperate need, we rely on them. It's eye-opening and gives perspective on what's truly valuable in life. Q: Tell us about a time when you saw the positive impact of healthcare or philanthropy. How did that influence your decision to get involved? A: One impactful moment in philanthropy stands out — the Music and Miracles concert featuring the Beach Boys. LP Insurance was a major donor, contributing $100,000 to benefit Sophie’s Place, a music therapy room coming to Renown Children's Hospital. On the day of the event, my wife and I volunteered and saw the remarkable community support for Renown Children’s Hospital. The collective efforts that day raised over $1 million, specifically designated to establish Sophie’s Place. This experience inspired me to want to do more, as I recognized the profound positive impact that philanthropy can have on healthcare and the community. Note: Sophie’s Place, opening later this year, will offer vital care and healing experiences for young patients at Renown Children’s Hospital.
Read More About The Impactful Role of Renown Health Foundation's Board of Directors
-
Department Spotlight: Renown Health Foundation
Kick off 2024 with us as we celebrate the team behind our very own Renown Health Foundation! When you visit Renown Health, you take a look around and can’t help but notice the robust programs in place. You look left and see our thriving Children’s Miracle Network Hospital at Renown, making a lasting impact on pediatric healthcare in our region. You look right and see the advanced William N. Pennington Cancer Institute, providing leading-edge treatments right here in our community. You look around you and notice an influx of smiling nurses from the Orvis School of Nursing at the University of Nevada, Reno (UNR) who receive tuition assistance, thanks to generous donations to the Gerald “Jerry” Smith Academic Practice Partnership. Then, you think to yourself: “These programs must need a lot of money and support. So, how on earth is this all possible?” What you may not know is that these programs are funded by the generosity of our community, all made possible by the work of Renown Health Foundation. As the largest not-for-profit health system in northern Nevada, our mission to make a genuine difference in the health and well-being of everyone we serve flourishes because of the donations, sponsorships, endowments and more that our Foundation brings in from philanthropists all over the region. Making It Happen The reach of Renown Health Foundation has proven to be virtually limitless, with a clear focus on supporting and raising funds for programs and initiatives that enhance the lives of our patients and their families, all for the betterment of our community for years to come. Under their growing umbrella, the dedicated team at the Foundation makes miracles happen through administering a wide range of philanthropic programs, including: Children’s Miracle Network Hospitals (CMNH), a nonprofit organization that supports the health of 10 million children in the U.S. and Canada every year. Renown Children’s Hospital is proudly recognized as a member of CMNH. Gerald "Jerry" Smith Academic Practice Partnership, a partnership between Renown Health and the UNR Orvis School of Nursing to provide 24 nursing students a year with full-ride tuition assistance and a guaranteed career in nursing at Renown. Fianna’s Healing Garden, a healing garden bringing serenity to all at Renown Regional Medical Center, built from the vision of Fianna Dickson Combs. Miracles at Montreux Golf Tournament, an annual golf tournament that takes place at Montreux Golf & Country Club and consistently raises hundreds of thousands of dollars for Renown Children’s Hospital. A full slate of individual giving programs, including Legacy Giving, Employee Giving and Leadership Giving. But it doesn’t stop there – the Foundation is helping our health system build more ways to care for our community by securing major gifts to fund advanced healthcare facilities and innovative healthcare solutions: William N. Pennington Cancer Institute, the premier oncology institute in the region providing a large array of personalized cancer care services, including Medical Oncology, Infusion Services, Clinical Research and more. Renown Institute for Robotic Surgery, offering the latest advancements in surgical technology with robotic-assisted surgeries, which ensure precision, faster recovery and improved outcomes. Sophie’s Place, a state-of-the-art music therapy room currently in construction at Renown Children’s Hospital. This new space will be specially designed for children and their loved ones to enjoy the healing power of music and engage in the arts. Conrad Breast Center, the latest addition to the planned Specialty Care Center at Renown South Meadows Medical Center which will include breast imaging, infusion and surgery services along with a wellness center. Jeanne and Raymond Conrad donated a $5 million lead gift to support this important project and the Foundation team is currently working to raise an additional $6 million in 2024. It may go without saying that a day-in-the-life of these spirited team members is never a dull one. Every day brings on a new challenge to face and a goal to meet. “A day at the Foundation is a day full of emails, calls and visits with friends of Renown,” said Abbey Stephenson, Planned Giving Officer. “Our main goal is to raise funds to support the mission of Renown, and most of our outreach efforts are to encourage philanthropy and donations. We have a very collaborative team, so we can often be found in each other’s offices strategizing about fundraising initiatives, communications and next steps with specific supporters.” “For me, a typical day involves making sure I have a donor scheduled for coffee or lunch, working on proposals that may need research and preparing presentations,” added Jerry Cail, Major Gifts Officer. “Staying connected, I send thank you notes for any donations-usually once a week and make at least three ‘Grateful Patient’ calls to set appointments. I always make sure I am ready to contribute to any meetings I have for the Foundation." While the scope of the Foundation’s charitable efforts goes beyond hospital walls, they also thrive right here in our own health system. Through our Grants Program, Renown’s departments and programs can leverage the connections and skills Renown Health Foundation has in order to secure funding from a multitude of grant sources. "Grant funds from foundations, and local, state and federal governments benefit the patients and communities we serve to further our mission, vision and values,” said Pam Citrynell, Development Officer. “Past grants have supported the purchase of state-of-the-art equipment, facility development, pandemic recovery, research and clinical trials, physician and researcher recruitment, community health programs and educational training for our healthcare professionals.” Every Foundation team member lives their passion every day while at work, frequently expressing gratitude for the immense impact they have the opportunity to make. “I love coming to work because I get a very real opportunity to make a genuine difference and meet some fantastic people who believe in and support our mission,” said Leah Nelson, Director of Community Giving. “I have had the honor of meeting donors and the families they support. I couldn't be prouder of what our team has accomplished over the years and am excited for what is to come.” The impact of the Foundation team’s tireless efforts extends far into the future, securing Renown’s lasting legacy in contributing to the continued health and well-being of our community. “Philanthropy is not only a financial science but a very specific methodology where connecting resources are paramount; it requires careful intelligent management coupled with lots of hard work, patience, and vision,” said Yvonne Murphy, Development Officer. “The work that the foundation does every day makes resources available to enhance the healthcare experience for all those who seek care at Renown. Our work impacts not only this present moment but in fact is a legacy that will bless this community beyond our lifetime.”
Read More About Department Spotlight: Renown Health Foundation
-
A Token of Appreciation: Renown’s Employee Giving Program
Pictured above from left to right: Jessica Bajwa, Nancy Bell, Laurie Goodman and Troy Fernandez As we approach the holidays and the season of giving, we reflect on the generosity and kindness that our employees here at Renown embody. Since 2007, Renown employees have donated $2,931,018 through Renown’s Employee Giving Program. This program provides our staff with the opportunity to make a difference by funding advanced equipment, research, community health initiatives, professional training and more. Regardless of the dollar amount, every contribution has a meaningful impact and remains entirely within Renown to support our mission. Employees can participate in the program at any time of the year by signing up for recurring payroll deductions or by making a one-time donation of any dollar amount. They can donate to one of Renown’s top priority areas of support or a different fund of their choice. Meet Jessica, Nancy, Laurie and Troy Renown employees Jessica Bajwa, Nancy Bell, Laurie Goodman and Troy Fernandez all have their own reasons for participating in the Employee Giving Program, but they all share the same goal: To give back to their community. Jessica Bajwa has been working at Renown for about seven years. She was at an employee event five years ago and found out about the Employee Giving Program through Renown Health Foundation. They explained the different areas she could donate to and how to get signed up. When Jessica looked back on the comforting care and healing her daughter had received at Renown Children’s Hospital, she felt empowered to give back to other children and families staying at Renown, so she enrolled in recurring payroll deductions to donate to Healing Arts. “It’s so easy and convenient to sign up,” said Jessica. “It means a lot to me to give to this area where they provide a healing environment, especially for patients and families at Renown Children’s Hospital – My daughter still has a blanket they gave her when she was there,” Jessica said she likes that the Employee Giving Program allows employees to choose their area of support to donate to and donation amount. Nancy Bell said she’s proud to give back to Renown after having received a great amount of support from her coworkers during an incredibly difficult time when a family member of hers was being cared for in Renown’s ICU, just three weeks into her employment at Renown. “I had employees from not just my team but also across the organization reaching out to me and checking in to see how I was doing,” said Nancy. Nancy said she was positively impacted by that kind of support through her work family at Renown and decided to start giving back in 2011 by signing up for recurring payroll deductions to donate to the William N. Pennington Cancer Institute – to this day, she is still making donations to this area of support. When Laurie Goodman began working at Renown in 2013, Renown’s Human Resources team offered her different ways to give back as an employee. “At the time, I was often caring for foster children and seniors,” said Laurie. “My family and I have always wanted to help others in need.” Laurie had been taking care of an elderly woman who was a patient at the old Renown Skilled Nursing Facility and decided to enroll in payroll deductions to donate to this facility. When that facility closed, she received a letter asking which area she wanted to transfer her donations to, and she decided to begin donating to Renown Children’s Hospital to give back to kids in the community. “I’m fortunate for not only my employment at Renown, but my husband’s and daughter’s employment as well. As employees of Renown, we have such great jobs, benefits and opportunities, and I think we should all strive to give back to express our gratitude and appreciation.” At his employee orientation in 2012, Troy Fernandez heard about Renown’s Employee Giving Program and learned that funds were needed for individuals who needed financial support to pay for healthcare services at Renown. He knew his donations would go to a good cause and signed up for recurring payroll deductions to donate to the Greatest Need Fund. “It feels good to be able to give back to those who are less fortunate than us,” said Troy. “It was very easy to enroll in this program, and I’ve been donating to the same support area ever since.”
Read More About A Token of Appreciation: Renown’s Employee Giving Program
-
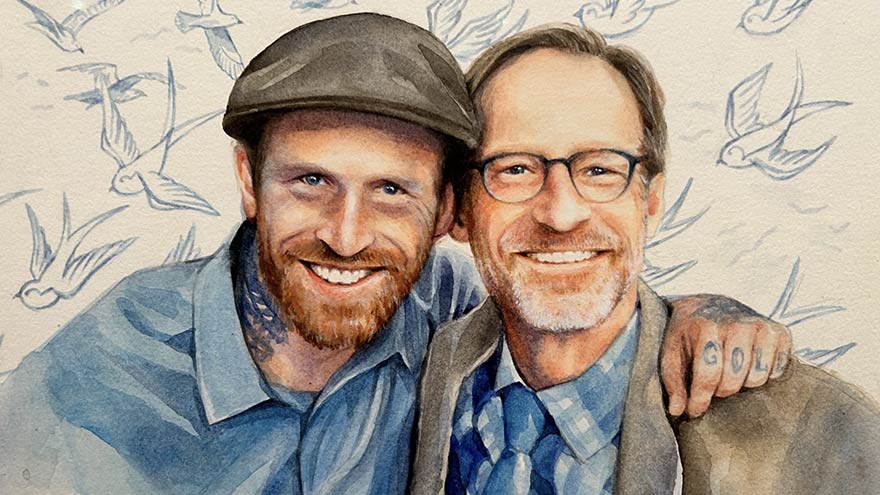
Why I Give: Dan’s Story
In the fall of 2020, Dan's world was suddenly shaken when he received a distressing call: his son, Jeremy, was admitted to Renown with complications from spinal meningitis. Without a second thought, Dan rushed from Southern California to be by Jeremy's side. For an agonizing 10 days, Dan remained in the ICU. He was overwhelmed with worry and helplessness as Jeremy fought for his life on a ventilator. During this time, Dan, an esteemed artist and professor, found comfort in the collection of artworks adorning the walls at Renown. With more than 2,000 pieces of original art, Renown has meticulously curated hospital rooms, hallways and various spaces to support those in need. Dan, who talks about art's magic every day as a professor, experienced its power in a new light.
-
Department Spotlight: Respiratory Care
This Department Spotlight is dedicated to Jason Simpson, Manager of Respiratory Services at Renown Children’s Hospital. Take a moment to breathe deeply. Inhale in, exhale out. We rely on our lungs to provide us with the air we need to live a healthy life – and this essential bodily function is something that many of us don’t think twice about since it comes easily for us. Now, imagine yourself as someone who is living with severe asthma, chronic obstructive pulmonary disease (COPD) or someone who was recently diagnosed with a frightening respiratory condition like COVID-19 or pneumonia. The simple act of breathing can prove to be an intimidating venture requiring the care of a professional. Who are the people that take on the challenge? Meet Renown Health’s Respiratory Care Services department. Serving patients across 13 service lines, three acute facilities, outpatient locations and telehealth, our respiratory specialists – including respiratory therapists, respiratory care aides, inpatient COPD respiratory therapy navigators and educators and more – use their expertise to help restore the vitality of all their patients with every inhale and exhale, shaping a healthier livelihood one lung at a time. The Guardians of Respiratory Wellness Whether they are managing lifelong respiratory conditions or offering crucial support in emergencies, the Respiratory Care team strives to enhance the quality of life for every patient. As an indispensable member of the clinical team at Renown, our respiratory therapists work collaboratively with doctors and nurses to tackle a wide range of tasks, tailoring care for each patient’s unique needs. “Respiratory care is involved with all stages of life, from beginning to end,” said Sarah Kurtz, Respiratory Therapist. “We work closely with nurses and doctors and perform arterial punctures, breathing treatments, weaning maneuvers for patients on life support, intubations and much more. We assess patients constantly to see if their care needs to be upgraded or if they can be weaned to get them back home with their families.” “You start your morning researching your assigned patients,” added Tim Start, Respiratory Specialist. “We go over lab values and chest radiographs and decide the best plan of care for each patient. Our objective is to improve their respiratory status by giving them medications and doing breathing exercises. We participate in other forms of care with nurses, such as activities of daily living (ADLs) and mobilization. We work as a team, and that enables us to provide great patient care.” For patients living with COPD, enjoying all that life has to offer comes with a separate set of obstacles. According to the Centers for Disease Control and Prevention (CDC), over 200,000 people across the Silver State are living with this chronic condition. Luckily for them, Renown has a specialized team to help these patients optimize their life and manage their condition with individualized treatment and education. “We run a report every morning to identify all the patients currently admitted who have a history of COPD, take respiratory medications or smoke,” said Amber Beck, Inpatient COPD RT Navigator. “After looking through their charts, we visit with the patient (and possibly their family) at the bedside to help them better understand how to manage their breathing issues.” As a vital part of the Respiratory Care team, Renown’s respiratory care aides help ensure the seamless operation of our respiratory care services. These dedicated professionals provide essential support to respiratory therapists not only during intricate procedures but also outside of face-to-face patient care by transporting equipment, restocking supplies, assisting in the mobilization of patients and more. “We are responsible for the maintenance of unit supplies and making decisions regarding levels of stock to be maintained,” said Dia Ramos, Respiratory Care Aide. “We also transport equipment, refill the oxygen tanks on the floors and intensive care units (ICUs), order and stock respiratory care supplies, mobilize patients and assist the respiratory therapists during bronchoscopies in the ICUs. In addition, we clean respiratory equipment like mechanical ventilators, continuous positive airway pressure (CPAP) and bilateral positive airway pressure (BiPAP) machines, high flows and aerosol poles.” Once the COVID-19 pandemic hit, a special spotlight shined upon respiratory care teams across the country for the heroic care they provided patients in respiratory distress. While their roles in health systems have gained a better understanding nationwide, this team understands it is vital for them to educate the community about the important jobs they hold for our patients. “Respiratory care can be under the radar,” said Pam Umek, Respiratory Specialist. “Once, when I told someone that I am a Respiratory Therapist, they said, ‘Oh, like a yoga breathing instructor?’ I then explained all the things we do: intubation, extubation, bronchoscopies, transports, traumas, codes, rapid responses, pediatrics/NICU, breathing medications/therapies, open heart rapid ventilator weaning … needless to say, that individual walked away with a better understanding of not just Respiratory Care Services but also the enormous effort it takes to care for our community.” The accolades and achievements continue to pour in, from national awards and certifications to implementing different jobs in care units to optimize the patient care experience. “We have earned and continue to maintain the Joint Commission Disease-Specific Certification for COPD,” said Amber Beck. “We are well below national averages for 30-day readmissions, lengths of stay and mortality due to COPD. Sandy, one of our COPD Coordinators, was a recipient of a patient advocacy award from the American Association of Respiratory Care and FACES Foundation.” “We have started implementing Respiratory Care Aides in the critical units, starting with the Cardiac ICU,” added Dia Ramos. “We work as one team and are always helping each other with their tasks.” Education and mentorship are at the core of Renown’s mission to make a genuine difference in the health and well-being of every patient. Nurturing the next generation of medical professionals – including respiratory care professionals – is a task that the Respiratory Care team takes seriously. “It has been great being able to help educate students in different disciplines,” added Pam Umek. “We have been able to offer shadow shifts to students in emergency medical services (EMS), nursing and medical school. These opportunities help students entering the medical field have a better understanding of the many ways we can help care for our respiratory patients.” From the moment of birth to the final stages of life, Renown is fortunate to have a Respiratory Care team that tirelessly ensures every breath counts, safeguarding their role as a trusted partner within our health system. A Tribute to Jason Simpson, Healthcare Hero
-
Living with COPD? How to Maximize Your Summer Experience
June offers an official welcome to summer and the height of outdoor activities in northern Nevada such as hiking, camping, days spent at the lake and embracing long days and warm evenings with friends and family. Enjoying all that the summer season has to offer may not be as easy for those living with chronic obstructive pulmonary disease, or COPD, which effects more than 15 million Americans. What is COPD? COPD is a group of lung diseases including emphysema and chronic bronchitis that result in airflow blockages from the lungs. People may experience frequent coughing and shortness of breath among other symptoms. COPD typically impacts adults ages 65 and older and is becoming increasingly more common among women. Although smoking plays a key role in the development of COPD, air pollution and indoor air quality, and respiratory infection also contribute to disease development. While there is no cure for COPD, limiting progression of disease and managing symptoms can be achieved through lifestyle changes, therapy, and medications. Tips for Living with COPD This Summer, and Always Stay Hydrated: Staying hydrated is extremely important for people with COPD, especially during the summer. Not drinking enough water can make breathing more difficult because it increases respiratory symptoms. Make sure to always keep a water bottle with you and aim to drink 8-10 glasses of water daily. Be Mindful of Temperature: COPD symptoms can be exacerbated by hot weather. It is best to participate in outdoor activities during the cooler times of day, like the morning or evening. Check Air Quality Before You Go: Before engaging in outdoor activities, be sure to check the air quality index and plan your activities accordingly. Pace Yourself: Exercising can be difficult for people who have COPD. To make the most of your summer, try not to push yourself too hard and take breaks when you need them. If you start to feel out of breath or tired, take a break in a cool, shaded area until you feel better. Take Matters Into Your Own Hands To address the needs of community members living with COPD, the Renown Health Research Office has teamed up with Pulmonary Medicine to provide patients who are former or current smokers and have a history of frequent exacerbations with an option to participate in the ARNASA study. "COPD exacerbations have a huge negative impact on patient’s lung function” states Dr. Farah Madhani-Lovely, Chief of Pulmonary Medicine at Renown Health and Assistant Dean of Clinical Research at the University of Nevada, Reno School of Medicine. “We have had inhalers and prednisone for decades but patients are still having exacerbations. Now we have a new pathway we think will prevent exacerbations which is what this clinical trial is designed to prove.” This study will evaluate the efficacy and safety of astegolimab compared with placebo in participants 40-80 years of age with COPD. “This study in particular is so exciting because of the enthusiasm from the sponsor’s end” says Katie Buckley, Lead Clinical Research Coordinator working on pulmonology studies at Renown’s Clinical Research Office. “Often times sites aren’t assigned particularly passionate or engaged personnel who aid in carrying out these studies, but you can tell Roche Genentech’s team truly cares about the success of the study, the safety of their participants, and proving the efficacy of the investigational agent. Working on a study like this takes a village, and when the individuals on all ends share similar mindsets and work towards success as a collective unit instead of as individual moving parts, it’s amazing to see everything we’re able to accomplish.” Renown’s team of expert pulmonologists and researchers are available to join patients with COPD in support of their healthcare journey. If you are interested in learning more about this clinical trial option at Renown Health, talk to your pulmonologist at your next appointment or contact us at 775-982-3646. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
Read More About Living with COPD? How to Maximize Your Summer Experience
-
Department Spotlight Clinical Research
May 20 is National Clinical Trials Day. Celebrate with us by recognizing the Clinical Research team at Renown Health! The root of every medication, treatment and procedure in healthcare can be traced back to research. From the beginning of the history of medicine, research has always played a crucial role in improving the lives of patients around the world, leaving a permanent mark on how we expand our medical capabilities to this day. Renown Health’s Clinical Research team, in partnership with the University of Nevada, Reno School of Medicine (UNR Med), are leading that effort in our very own community. As our in-house leaders of clinical trials, this team is dedicated to advancing the science of medicine to help further our bottom line of making a genuine difference in the health and well-being of the patients they serve. Trial by (Medical) Jury Every day looks different for the Clinical Research team, especially when it comes to interacting with patients, providers and “sponsors,” which are the organizations providing the treatment for the study. One fact always remains true: communication and collaboration are key, especially among the team who act as the face of this process. Meet Lisa English (pictured above on the far right in a blue shirt), a Lead Clinical Research Coordinator at Renown who serves as the study "project manager." One aspect of Lisa’s day-to-day is seeing patients through their clinical trials from start to finish. It all begins with the setup. “Before we can launch a study, there is a lot of back-and-forth dialogue between everyone involved to ensure the best fit,” said Lisa. “Sponsors will come to us with novel treatments, such as medications or devices, and the inclusion criteria that patients need to meet in order to qualify for the study. We then immediately jump into working with the providers, looking closely at the science and comparing the treatments to what is on the market already.” From there, Lisa coordinates conversations between the providers, sponsors and study teams to gauge everyone’s capacity based on the length of the study, ensuring everyone involved has the time to dedicate to the process. Next, the providers identify patients that meet the criteria for the study, and together, the team decides where the patient visits will happen and discusses any potential barriers that may affect patient retention. The budget is clearly defined at this stage, set up to make sure no patient is ever billed for medical costs incurred as a result of the study. Often, research participants are seen within the specialty clinics throughout the health system, while other times the Clinical Research Coordinators see patients at the recently centralized Clinical Research Office at Renown Regional Medical Center. This location provides an essential public-facing space for the community to learn more about clinical trials and demonstrates the breadth of resources available at Renown to sponsors to strengthen external partnerships and research funding opportunities. Once the study officially begins, team members like Lisa will set patients up for a “screening/qualifying visit.” During this appointment, she makes sure patients get scheduled for their lab work, imaging scans and anything else the provider may need to make an executive decision on whether or not the patient is a good candidate for the study. “I build it all in Epic,” said Lisa. “The study information, directions, requirements and next steps are all loaded in Epic for easy tracking. We are also required to input any notes in the sponsor’s electronic data capture website. All the information I track is inputted without protected health information (PHI), so every patient is completely anonymous.” After the patient officially qualifies, the study goes full steam ahead. Team members like Lisa and the providers receive continual updates from sponsors on the status of the study. “Throughout the entire process, I make sure patients get scheduled for everything that meets the requirements for the study,” said Lisa. “I meet with patients one-on-one to discuss their needs and concerns and ask questions about the study, organize their appointments and charts and deal with any issues or pivots that may arise. It’s very important that every patient fully understands what is going to happen with their care.” The Clinical Research department strives to serve as a care partner to patients, providers and clinics they work with. The majority of our Clinical Research Coordinators are trained phlebotomists and medical assistants, performing their own assessments such as lab draws and electrocardiograms (ECGs) to streamline the research visit process and reduce resource constraints on the clinics and health system. Lisa typically sees a couple of patients per week, depending on the study and where patients are in the cycle. Depending on the complexity of the trial, patients may see the research team only one time or several times over many years. Typically, clinical trial patients are seen in clinic every 2-4 weeks. There are many tasks required before, during and after a research visit to ensure everything runs smoothly, so Clinical Research Coordinators dedicate an average of 5-11 hours of work per patient, per visit. Regardless of patient load, each employee in the Clinical Research department – as well as participating teams across Renown and UNR Med – always step in to help each other out. According to Lisa, the environment is immensely supportive. “We have a program here at Renown to train employees who have never done clinical trials,” said Lisa. “We love seeing people get more engaged with the important work we do, and every department has been great at collaborating with us. Everyone brings a different perspective.” At the end of the study, Lisa gathers all the information and collects notes into a zip drive or paper binder for archiving. The sponsor lets the Clinical Research team, providers and patients know whether they are on the trial drug or on the placebo. The teams use the data gathered during the study to publish a report or present at conferences, promoting the critical research done to better the lives of patients in our community, and potentially, the world. “I appreciate the time everyone gives us to make sure our research is successful,” said Lisa. “It feels great to work together to make a difference, improve healthcare quality and save lives.” Behind-the-Scenes, Yet on the Frontlines The impact of research studies transcends hospital walls, and this can all be attributed to the dedication of our Clinical Research department. The constant collaboration between this team, lab science, medical assistants and providers, cardiology technologists, sonographers, finance teams and our partners at UNR Med is crucial to safeguarding the success of the studies. Devoted to keeping research close to home, Renown and UNR Med teamed up to form the Clinical Research Office (CRO) in 2021. With the strength of northern Nevada's largest not-for-profit health system and Nevada’s first medical school, this team is dedicated to giving our community access to the latest care innovations. “At UNR Med, we are working with students, residents and academic faculty; on the Renown side, we are working with clinicians and community participants,” said Amber Emerson, Manager for Community Outreach and Research Engagement for UNR Med. “Everything we do is data-driven,” added Kristen Gurnea, Manager of Clinical Research for Renown. “Our main goal is to optimize our impact and provide a community benefit for our patients. The scope of our roles in the Clinical Research office is very diverse.” To help meet the growing need locally for healthcare and cutting-edge treatment solutions, the CRO has continued to grow, expanding its research capabilities and helping bring new medications, medical devices and more to patients across northern Nevada and northeastern California. “Once upon a time, our team had only six members; today we have grown to a team of 25,” added Diana Torres, Research Resource Analyst for Renown. “We used to be considered one department, including Medical Education, and we have since branched off into our own cost center. We branched off even further and created a separate Genetics department that runs the Healthy Nevada Project. Throughout this process, the Clinical Research department was always the main point of the umbrella.” “We participate in hospital-wide outreach and marketing, and we feel this has really helped us get the word out about our department,” added Raul Arellano, Research Resource Analyst for Renown. “In fact, we doubled our clinical trial portfolio from last year.” The CRO currently operates over 100 clinical trials locally in cardiology, endocrinology, infectious disease, neurology, pediatric and adult oncology, pediatric sub-specialties and pulmonology. Behind the curtains of in-person research, the CRO is home to several experts who help turn our research studies into a reality, from budgeting and billing to barrier-breaking and building relationships. “I help with barriers patients and Clinical Research Coordinators are facing, building connections and relationships inside and outside of our health system,” said Kristen Gurnea. “I enjoy handling all the supporting pieces that are required for studies to happen.” “My role changes every day,” added Jenna Berger, Administrative Assistant for the CRO at Renown. “Some days, I’ll be helping coordinate patient stipends and going through document management to ensure we have all necessary signatures. Other days, I will be planning events – like Clinical Trials Week – for our department and creating marketing materials and fliers.” “Our day-to-day involves going over anything related to research financials,” added Diana Torres. “We handle sponsor billings, process efficiency and collecting revenue for research contracts, and we collaborate closely with our Finance department and Revenue Integrity in order to accomplish this. It’s important for us to make sure all billing on both the sponsor and patient side is taken care of, especially because patients should never receive a bill for medical services they receive for the trial. A year and a half ago, we started doing budget negotiations for research contracts,” said Diana Torres. “We are proud to help clinical teams with any training they may need on these negotiations as well as billing reviews and allocations.” Seeing patients progress during a study and transform before their eyes inspires the CRO team to continue doing what they do every day. “I’ve been here for many years, first working on the floor as an oncology nurse and transitioning to oncology research in 2005,” said Anna Winchell, Cancer Protocol Nurse for Renown. “I love getting to know the patients and seeing them progress into a healthy lifestyle.” Medical students and residents at UNR Med also play a significant role in the research process, advancing medicine by exploring causes and novel treatments for a wide range of conditions, including HIV, muscular dystrophy, gastrointestinal disorders, infectious diseases and more. Medical research at UNR Med is headed by committed research coordinators, community outreach managers, grants managers, pharmacists and physicians. “I oversee scientific review and help the physicians that come to us for those resources,” said Amil Trujillo-King, Medical Research Coordinator at UNR Med. “I guide medical students in their research protocols and help with different projects to improve research activities for both students and medical residents.” It takes a village to make clinical research happen. Because of that, the ACRO cannot thank the following teams enough for moving mountains for the future of medicine: Renown Health and UNR Med leadership for demonstrating the integrated health system’s commitment to expanding access to clinical research in our community within both the Renown / UNR Med affiliation and Renown active strategic plans. Renown Pharmacy especially Research Clinical Pharmacist Tim Morton, who supports all clinical trial medication dispensing and patient education across all clinical trials at Renown. Accounts Payable for having a huge impact on patient and employee reimbursement. Renown Medical Group for their participating providers, especially in oncology, cardiology, pulmonology, pediatrics, endocrinology and neurology, who are involved in research year after year. Marketing and Communications for helping with printed materials and raising awareness for clinical research at Renown and UNR Med. An Affiliation to Last Through the Ages A collective, shared vision of exploring community health – that is the impetus behind the affiliation between Renown and UNR Med. By leveraging resources across both institutions, the CRO has maximized their impact, giving the people of northern Nevada greater access to new interventions and treatments and promoting an impassioned culture with patients, providers, residents and medical students. “Community-based research always sat well with me,” said Amber Emerson. “As Renown and UNR Med, we have this unique opportunity to shape clinical research here in northern Nevada. We always make sure we present research in a meaningful way that speaks to the work we produce and demonstrates the opportunities we offer. After all, participating in clinical research doesn’t mean our patients are ‘guinea pigs’ – quite the opposite! They are partners in their health care, and we support them through providing access to novel treatments.” “Research is my passion, and my career has spanned broadly from grants administration to study coordination,” added Valerie Smith, Clinical Research Center Administrative Manager at UNR Med. “I am excited to be at the forefront of research frontiers in northern Nevada.” Through robust engagement and collaboration with healthcare providers, department administrators, internal research team members and leadership, the strength of this affiliation is unmeasurable. The CRO’s ultimate goal is to have clinical trials be the standard of care for every condition that Renown and UNR Med treats. Clinical research participation is all about patient autonomy, shared decision-making between patients and their providers and advancing medicine to save lives. From their beginnings as a small group of passionate researchers to their present reality as a leader in the research space in northern Nevada, their efforts do not go unnoticed. “The success of our department is inspiring,” said Amil Trujillo-King. “Renown and UNR Med supports the wellbeing of all employees and contributes directly to the growth of the department.” “When I first joined Renown in Patient Access, I didn’t realize that we had a research department; with a strong healthcare background in my family, I knew I wanted to grow in my career, and our expanding Clinical Research office was that next step,” said Raul Arellano. “With our affiliation with UNR Med, it’s especially inspiring to be able to apply what I learned as a Patient Access Representative to help further outcomes for our patients through managing our finances.” Through their unwavering commitment to research excellence and patient-centered care, the CRO will continue to pave the way for groundbreaking medical discoveries and improved outcomes for patients for years to come. “Fundamentally, we’re working to build a culture of research in our community because we believe it is the right thing to do. Our community deserves to have access to clinical trials and novel care close to home with a dedicated team to support them every step of the way,” closes Kristen Gurnea.
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Your Ultimate Cold and Flu Survival Guide
While viruses can attack year-round, colds, flus and other respiratory illnesses are typically more prevalent during fall and winter. People spend more time indoors, which allows viruses to pass more easily from one person to another. The cold, dry air can also affect the respiratory system, making it more susceptible to germs. According to the CDC, flu activity in the U.S. often begins to increase in October and peaks between December and February. “Flu season” can last as late as May. When it comes to the cold and flu, prevention and preparation are key. Getting the flu shot and a COVID-19 vaccine is the first and most crucial step in protecting against these two respiratory illnesses. Preventative actions, such as washing your hands, covering your mouth and nose when coughing or sneezing and getting enough sleep can also help you avoid getting sick. However, despite your best prevention efforts, the time may come this winter when you start to feel a little scratch in your throat or a fever coming on. By taking steps ahead of time to assemble a cold and flu survival kit, you’ll be more prepared for whenever illness strikes, allowing you to stay home, rest and avoid spreading germs. Tips for Managing Symptoms Keep these tips in mind to ease your cold or flu symptoms: Stay home and rest Drink plenty of fluids Treat aches and fever with over-the-counter medication such as ibuprofen or acetaminophen Manage a cough with over-the-counter expectorants or suppressants Run a humidifier or sit in a steamy bathroom to ease congestion What to Stock in Your Flu Survival Kit Be ready when a cold or the flu strikes by having a flu survival kit filled with these get-well essentials stocked in your pantry, fridge and medicine cabinet: Over-the-Counter Medications: Take advantage of over-the-counter medications to make yourself feel better and ease most common flu symptoms of fever, headache, cough, muscle aches, sore throat, and runny or stuffy nose Pain relievers - Ibuprofen (Motrin and Advil) or Acetaminophen (Tylenol): for fever and aches Decongestants: for sniffles and congestion Cough expectorant (guaifenesin): for a “wet” cough to help clear secretions from the lungs Cough suppressant (dextromethorphan/DM): for a severe “dry” cough to block the cough reflex Cough syrups and drops Drinks: Water Herbal tea Low-sugar sports drinks Pedialyte Foods: Chicken soup Broth Vitamin C-containing fruits and vegetables Oatmeal Toast (add some avocado, honey or egg) Miscellaneous items: Tissues Lozenges Protective mask Thermometer Humidifier When to Seek Care and Where to Go Most healthy adults who have a cold, the flu, or other mild respiratory illnesses don’t need to see a care provider and will recover at home with self-care measures. Because these are viral illnesses, antibiotics won’t work against treating them. Your care provider may be able to prescribe an antiviral medication that can relieve your symptoms and shorten the duration and severity of your illness; however, this needs to be started within 48 hours of symptom onset and is often only prescribed to individuals at high risk for developing complications from the flu or those experience severe symptoms. Primary Care or Urgent Care Contact your primary care provider or visit an Urgent Care if you are at an increased risk, including those who: Are 65 years of age or older Have chronic medical conditions Are pregnant or recently gave birth Have a weakened immune system Find a primary care provider If you are otherwise healthy and not at increased risk of complications, seek medical advice if your flu symptoms are unusually severe, such as mild difficulty breathing, a severe sore throat, coughing that produces a lot of green or yellow mucus, or feeling faint. Emergency Care Go to the Emergency Department if you are experiencing emergency warning signs such as severe pain (chest, abdomen), concern for heart attack or stroke (slurred speech, new localized weakness), severe dehydration (needing IV fluids) or severe shortness of breath.
-
Plan Early: Completing Your Advance Directive
We plan for the birth of a child, weddings and retirement, but rarely do we discuss how we want to be cared for at the end of our lives. Getting through this challenging conversation and completing an Advance Directive can give you peace of mind that your loved ones will not have to make difficult choices on your behalf. The best time to complete an Advance Directive is now – don’t wait until a life-limiting illness or crisis occurs to discuss your views about end-of-life care and to learn what choices are available. By preparing in advance, you can help reduce the doubt and anxiety related to decision-making for your family if you cannot speak for yourself. What are Advance Directives? An Advance Directive is a document that states your choices about medical treatment and names another person to make medical decisions on your behalf if you are unable to. This document allows you to make legally valid decisions about future medical care. “Completing your Advance Directive is a gift you give your family,” says Director of Palliative Care, Mary-Ann Brown RN, MSN. “The stress associated with these difficult decisions is decreased if everyone knows what is important to you and what you want at the end of life.”
Read More About Plan Early: Completing Your Advance Directive
-
Estate Planning Mistakes to Avoid
August is National Make-a-Will month. We talked to Renown Health Foundation Planned Giving Officer, Abbey Stephenson, to learn more about wills, trusts, and estate plans and why you should feel motivated this month to get started. Did you know that 2/3 of Americans don't have a will or trust? If this is you, don’t worry, you’re not alone. Although there are laws in place to determine who inherits your assets if you die without a will or trust, having a will or trust ensures your assets go where you want them to go after you are gone. They can also help minimize disputes between family members and heirs about who gets what. In Nevada, the laws that govern who gets what if you die without a will or trust can be found in Chapter 134 of the Nevada Revised Statutes. There are other documents that people often prepare at the same time as their will or trust – like an advance health care directive and durable power of attorney for assets. These documents all together are called an estate plan. Although they have other purposes too (like nominating a guardian for a child, planning for disability or avoiding probate, which is a court process), wills and trusts are documents that say who will receive your assets after you are gone. The most common type of trust is often called a revocable living trust or a family trust. People who have a trust usually still have a will, although it is a shorter form of will called a pour-over will. It’s a good idea to talk to an estate planning attorney about whether or not a trust makes sense for your family or circumstances. Now that you’re ready to get started, here are some mistakes to avoid: 1. Failing to plan Not setting aside the time to plan may be the biggest mistake. Failing to prioritize preparing or updating your estate plan means your last wishes and desires may not be fulfilled. The right documents memorialize what you would like to happen upon your disability and death so that other people can know and follow your wishes with respect to your care and your assets. 2. Failing to coordinate beneficiary designations Certain types of assets like life insurance and retirement accounts are not covered by your will or trust and need to be addressed separately. These types of assets are referred to as non-probate assets because they transfer under contract principles and don’t require court supervision or probate to be distributed to the named beneficiaries. By completing beneficiary designation forms provided by the retirement account custodian, insurance company or financial institution, you can direct your assets to one or more beneficiaries. 3. Failing to title your assets properly Asset titling refers to how you own your asset – such as in your individual name, jointly with someone else, or in a trust or entity. For example, assets titled for two people with a “right of survivorship” will automatically go to the surviving owner. Review your asset titling and make changes, if needed, to ensure your property and assets are passed down the way you intend. 4. Failing to include charities meaningful to you In addition to providing for family members and other important people in your life, you many also choose to give to charities meaningful to you in your estate plan. When you include a charity in your estate plan, that gift is called a planned gift and many charitable organizations, including Renown, recognize such donations through their legacy giving societies. As you prepare to make your own will or a more comprehensive estate plan, we recommend you consult with a lawyer. Here are some free resources that may be helpful too: Renown Health Foundation is proud to sponsor the Family Estate Planning Series put on by PBS Reno and the Community Foundation of Northern Nevada. The free, 8-week course of 90-minute, in-depth workshops is a great place to learn much more and to help you get started in the planning process. The next course begins on September 7, 2022. More information can be found here. Renown Health offers periodic advance health care directive workshops where attendees can learn about, complete, and sign their directive. The next workshop is scheduled for September 14th. More information can be found here. The American College of Trust and Estate Counsel provides information on a number of commonly asked estate planning questions here. If you are interested in including a charitable gift to Renown in your estate plan, we would be happy to talk to you about how your gift will make a difference for our mission. Please contact Abbey Stephenson at abbey.stephenson@renown.org or visit renown.org/LegacyGiving to learn about Renown Health Foundation’s Legacy Giving Society and ways to give.