Search
-
Celebrating Resilience: Raquel's Remarkable Journey Through Breast Cancer Treatment
Raquel was 33 when she was diagnosed with breast cancer. It was April 2023, when she found a lump in her breast and was referred to the William N. Pennington Cancer Institute. After comprehensive imaging, she was diagnosed with invasive lobular carcinoma, which is a type of breast cancer that begins in the milk-producing glands of the breast. Between June 2023 and January 2024, she received a total mastectomy, chemotherapy and radiation at Renown Health. “Breast cancer is uncommon in women under 40, but any woman with a mass or lump in her breast should have an exam by a physician and imaging at any age,” said Dr. Lee Schwartzberg. In fact, according to the Centers for Disease Control and Prevention (CDC), only 9% of all new cases of breast cancer in the U.S. are found in women younger than 45. “It was a pretty scary diagnosis, but I’ve been led by great people through the process,” she said. “They were so helpful and there for me throughout the chemo and radiation.” Raquel's journey through breast cancer treatment at the William N. Pennington Cancer Institute was marked by the exceptional care provided by the Renown Health team, including nurses, nurse navigators, therapists, support teams and providers. Among the dedicated professionals, Dr. Michelle Chu and Dr. Lee Schwartzberg played pivotal roles in Raquel's diagnosis and subsequent treatment plan. Their expertise, compassion and commitment to patient care left an indelible impact on Raquel's experience. Their thorough examination and comprehensive approach ensured that Racquel received the best possible care for her invasive lobular carcinoma. In addition to the care provided at Renown, Raquel greatly benefitted from being connected with a mentor by Dr. Chu. This mentor, Kayla, had undergone a similar diagnosis and treatment plan, and at the same age Raquel. They texted and called each other throughout Raquel’s treatment, providing additional support through a challenging time. As of January 2024, Raquel is done with her treatment and continues to see her care team for follow-up appointments. “I’m through the worst and ready to rebuild my life,” Raquel said. To help celebrate this milestone, Nevada Athletics invited Raquel to receive the game ball at a Nevada Men’s Basketball game. She was joined on the basketball court for this special recognition by her husband, Raul; mother, Arlene; and two daughters, Ryleigh and Rhiannon. Racquel's journey is not only a testament to her resilience but also a tribute to the invaluable contributions of Dr. Chu and Dr. Schwartzberg in guiding her towards triumph over breast cancer.
Read More About Celebrating Resilience: Raquel's Remarkable Journey Through Breast Cancer Treatment
-
How Regular Cervical Cancer Screenings Can Save Lives
According to the American Cancer Society, approximately 13,820 new cases of invasive cervical cancer will be diagnosed, and 4,360 women will die from cervical cancer. However, cervical cancer is preventable with regular screening tests and the HPV vaccine. It’s important to note that medical advances have allowed progress in diagnosing and treating cervical cancer. While it used to be one of the most common causes of cancer death for American women, the incidence of death has significantly declined. What to Know About the HPV Vaccine HPV vaccination is the best way to prevent cervical cancer and is recommended for all youth starting as early as age 9, or for teens and adults up to age 45 who didn’t start or finish the series. In Nevada, only 50.1% of teens ages 13-17 have been vaccinated for HPV. There are 13 types of HPV, and the vaccine Gardasil 9 protects against 9 of those HPV strains, greatly reducing the incidence of cervical cancer among vaccinated individuals. What to Know About Cervical Cancer Screenings The CDC says the most important thing you can do to help prevent cervical cancer is to have regular screening tests starting at age 21. And there are two common tests that can detect early stages of cervical cancer (or precancer) and improve health outcomes. The pap test (or pap smear). This screening looks for precancers. Women should begin getting pap smears when they’re 21. The human papillomavirus (HPV) test looks for the virus that can cause these cell changes. Cervical Cancer Screening Schedule The American Cancer Society offers the following guidelines for screenings: All women should begin cervical cancer screening at 21. Women between 21 and 29 should have a pap test every three years. Beginning at 30, the preferred way to screen is with a pap test combined with an HPV test every five years. This is called co-testing and should continue until age 65. A pap test (or pap smear) is performed during a regular screening appointment to look for precancers, cell changes on the cervix that might become cervical cancer if they are not evaluated or appropriately treated. Typically outpatient procedures can reduce the risk of long-term health impacts that prevent pre-cancerous cells from becoming cancer cells. Women over 65 who have had regular screenings in the previous ten years should stop cervical cancer screening as long as they haven’t had any severe precancers found in the last 20 years. How to Get Screened Request an appointment with your primary care physician or OBGYN to schedule a screening.
Read More About How Regular Cervical Cancer Screenings Can Save Lives
-
6 Signs of Heart Failure
Heart failure is a serious medical condition that occurs when the heart is unable to pump blood effectively, leading to a variety of symptoms and potential complications. Although there has been progress made in the treatment of many forms of heart disease, heart failure continues to be a prevalent and life-threatening condition – nearly 6.2. million adults in the U.S. have heart failure. Recognizing the signs of heart failure is crucial for early detection and timely intervention. We talked to Ruth Skinner, APRN at the Renown Institute for Heart & Vascular Health, about recognizing common signs and symptoms of heart failure. Heart Failure Signs and Symptoms The symptoms of heart failure may be subtle and can be mistaken for normal signs of aging. Common symptoms of heart failure are due to extra fluid or congestion – typically starting with congestion of the lungs, then moving to different parts of the body. Common heart failure symptoms include: Breathing Difficulties (Dyspnea): One of the hallmark symptoms of heart failure is shortness of breath during daily activities and having trouble breathing when lying down. Fatigue and Weakness: Because heart failure can lead to reduced blood flow to the body’s tissue, patients may find themselves becoming tired and weak even during routine activities. Swelling (Edema): Fluid retention in the body can cause noticeable swelling. Weight gain along with swelling of the feet, legs, ankles or stomach is often a key sign of worsening heart failure. Rapid or Irregular Heartbeat: Heart failure can disrupt the heart's electrical signals, causing irregular heartbeats (arrhythmias) or a rapid heartbeat (tachycardia). These can be felt as palpitations or fluttering sensations in the chest. Persistent Cough or Wheezing: Fluid buildup in the lungs triggers a persistent cough, sometimes accompanied by pink or white mucus. Loss of Appetite or Nausea: Heart failure can affect blood flow to the digestive system, leading to symptoms like loss of appetite and nausea. If you or a loved one experiences any of the above signs and symptoms, it’s important to seek medical attention promptly.
-
What Is an Echo-Tech?
When it comes to our heart, keeping this vital source of life in tip-top shape is of utmost importance. Echo technologists or echocardiographers, otherwise known as "echo-techs," are charged with that mission, providing critical information that leads to life-saving interventions to keep our hearts beating strong. Adrianne Little, echocardiographer at Renown Health, breaks down the echo-tech's role in the health system, the educational path it takes to get there and the unique perks that come with the profession. What does an echo tech do? “Echo techs play a key role in the diagnosis and treatment of patients,” said Adrianne. “We are members of the cardiovascular imaging team that perform ‘heart ultrasounds’ or echocardiograms. Although we are most commonly known as echo techs, our official title is either ‘cardiac sonographer’ or ‘echocardiographer.’” Echo techs use imaging technology and sophisticated ultrasound equipment to produce images of the heart. These images show how well the heart functions, as well as the valves, chambers and blood flow. Echocardiograms are used to diagnosis and treat a variety of heart conditions such as murmurs, arrhythmias and heart failure. At the end of the day, the main goal of echo techs is to help our cardiovascular team provide the quickest and most accurate diagnoses to help with patient management and help them receive the highest standard of care. “When it comes to looking at the heart, we are part of the front-line team," said Adrianne. “We provide real time critical information that leads to life saving interventions down the road.”
-
Staying Heart-Healthy with Genetic Screening
February is American Heart Month. While cardiac care is crucial every time of year – especially as heart disease stays the number one killer in the United States – American Heart Month serves as a great reminder to stay on top of your heart health. We spoke with Malina Ruiz, a cardiology nurse practitioner at Renown Health, on three key ways to embrace heart-healthy living and how genetic screening can help inform you of certain genetic risks that can play a role on the cardiac life stage. 1. Invest in a heart-healthy diet. Eating a diet that is rich in fruits, vegetables, whole grains and healthy fats (including monounsaturated fats such as avocados and polyunsaturated fats such as sunflower oil) is a key defense in protecting your cardiac health, according to Malina. While you are filling your plate with these nutritious foods, remember to keep an eye on your saturated and trans-fat intake, and try limiting foods that are high in those fats. “No matter what age we are, maintaining a heart-healthy diet will always be important,” said Malina. Need help finding cardiac-friendly meals? The National Heart, Lung and Blood Institute makes it easy with heart-healthy recipes and tips from experts. 2. Do an exercise audit. “Keeping an active lifestyle during our younger years is one of the most important factors that affect heart health in future years,” said Malina. Maintaining a regular exercise regimen that allows you to raise your heart rate and break a sweat can help prevent future cardiac events. A good rule of thumb is to aim for 150 minutes a week of moderate-intensity exercise, which averages out to 30 minutes a day on 5 days out of the week. It’s never too late to start a regular exercise routine! Exercise doesn’t have to be something you dread – leverage American Heart Month to find activities that you enjoy. The American Heart Association can help you discover new ways to move your body. At the end of the day, as Malina emphasizes, “any movement is better than nothing!” 3. Don't skip those check-ups. Regular preventative visits with your primary care provider can help you identify possible risk factors for heart conditions before they start actively affecting your life. “Check-ups become even more important as we age, along with being aware of the signs and symptoms of heart disease, heart attack and stroke,” added Malina. There’s no time better than the present – call our expert scheduling team today at 775-982-5000 to request a preventative check-up with your primary care provider.
Read More About Staying Heart-Healthy with Genetic Screening
-
8 Reasons to See a Cardiologist
While February is recognized as American Heart Month, it’s important to prioritize your heart health 365 days a year. Cardiologists play an integral role in our overall health and wellbeing – they are the experts when it comes to preventing and treating heart and vascular diseases. Dr. Jad Al Danaf of Renown Institute for Heart & Vascular Health shares eight reasons to visit a cardiologist. 1. Abnormal EKG The American Heart Association states an electrocardiogram, abbreviated as EKG or ECG, is a recording of the heart’s electrical activity to measure the rate and rhythm of the contractions in the upper and lower chambers of the heart. An EKG detects heart problems or abnormalities. If you have an EKG that shows abnormal results, you’ll want to see a cardiologist. An abnormal EKG can mean many things, such as irregular heart rate, heart rhythm abnormalities in the shape or size of the heart, medication side effects, and more. A cardiologist is most qualified to evaluate an abnormal EKG and determine the cause. 2. Immediate family history of heart disease or sudden cardiac death Knowing your family health history is essential to identify if you’re at risk for certain health conditions such as heart disease. For example, if you’re aware of anyone in your immediate family who had or has had heart problems or passed away from sudden cardiac death. In that case, you’ll want to discuss it with a cardiologist so they can determine if screenings, medications, or lifestyle changes are needed to help lower your risk. 3. Chest pain or shortness of breath with exertion If you have chest pain or shortness of breath that starts or worsens with activity, it may indicate a heart problem, and you should schedule a visit with a cardiologist immediately. Severe chest pain might be a sign of a heart attack or other serious medical emergency. If you’re experiencing severe chest pain, shortness of breath, or any other signs of a heart attack, call 911 immediately. 4. High blood pressure Have you had a high blood pressure reading? If so, it’s recommended to consult with a cardiologist for further evaluation. High blood pressure puts you at risk for heart disease and stroke, as uncontrolled high blood pressure can damage arteries, reducing blood flow and oxygen to your heart and brain.
-
Heart Failure Risks and Expecting the Unexpected
For the average person, detecting the signs of heart failure can be tricky, especially since people can look fairly healthy and have few symptoms. We asked Christopher Rowan, M.D., of the Renown Institute for Heart & Vascular Health, to answer our most pressing questions about heart failure. Even with more technology in medicine and a greater awareness about health today, the Centers for Disease Control and Prevention still reports that one in every four U.S. deaths is caused by heart disease. The real tragedy of heart-related deaths is that they are both common and preventable. “Heart failure can have many forms that are seen in anyone at any age," says Christopher Rowan, MD, with Renown Institute for Heart & Vascular Health. "As many forms as it has, it can also have as many causes. Although the symptoms of heart failure are numerous, people can look mostly healthy and have relatively few symptoms.” We sat down with Dr. Rowan to ask some common questions about heart failure. How can I tell if I have heart failure? What are some sure signs? "The signs and symptoms of heart failure are numerous, but the most common ones are shortness of breath when trying to walk (which differs from somebody’s normal pattern); progressive swelling in the feet, legs and ankles that does not disappear overnight; and waking up at night due to shortness of breath or waking up more than normal to urinate," Dr. Rowan says. Can heart failure be cured? "The treatment of heart failure depends on its primary cause," Dr. Rowan says. "Various forms of heart failure can be cured; however, the person is always at risk for recurrence. Some forms of heart failure have no cure but can be managed and stabilized and people can live a relatively normal life for years." What can I do to prevent heart failure? "To prevent the onset of heart failure, know your risk factors, including high blood pressure, diabetes, smoking and an unhealthy lifestyle," Dr. Rowan says. "If you have any of these risk factors, work to get them under good control and stop smoking. If you are overweight, start a daily routine where you walk at least 45 minutes per day, 5 days per week. Walking is the best exercise for your cardiovascular health." To learn more, visit the Heart Failure Program at the Renown Institute for Heart & Vascular Health. We want to hear your story! If you or a friend have been treated for a heart condition at Renown Health and are interested in chatting with us about your experience, please email your contact information to support@renown.org so we can follow up.
Read More About Heart Failure Risks and Expecting the Unexpected
-
The Salty Six: Are High-Sodium Foods Increasing Your Stroke Risk?
Excess amounts of sodium doesn’t just increase your risk of a heart attack, it can also increase your risk of a stroke. Unfortunately, avoiding that saltshaker may not be enough. Did you know that the average American consumes 3,400 milligrams of sodium each day? That’s a dangerous number considering that the American Heart Association recommends limiting daily sodium intake to 1,500 milligrams (about half the weight of a penny) to reduce the risk of heart disease and stroke. The problem is not necessarily that you’re putting too much salt on your food, it’s that salt is already in the foods you’re regularly eating. To help keep your sodium intake at a healthy level, make sure you’re aware of “The Salty Six,” six sneaky foods that are surprisingly high in sodium. Breads, Rolls and Tortillas: Although breads and tortillas may not initially appear to be high in sodium, we often consume several servings. Make sure to keep track of your total servings to see how they add up. Deli Meat, Cured Meats and Poultry: It may surprise you that six thin slices of deli meat can add up to more than half of your daily limit, so be mindful when building those sandwiches. Also, do your best to avoid cured meats, which often means the meat has been salted. Substitute uncured, skinless meats instead. Cheese: Salt is an important addition in the cheese-making process, as it prevents bacterial growth. Unfortunately, that added salt can increase your health risks. Limit the amount of cheese you add to meals to keep your sodium content down. Pizza: Take a quick look at the first three items above and it should be no surprise as to why pizza made the list. One slice and you’ve met at least half of your daily limit. Go easy on the cheese and try adding more veggies instead of meat. Canned Soup: One cup of canned soup can be as high as nearly 1,000 milligrams of sodium. When shopping for canned soup it’s important to check the label – not just on sodium content but serving size as well. Always select low-sodium options when possible or cook your own soup at home. Sandwiches and Burgers: A sandwich or burger from your favorite restaurant can contain more than 100 percent of your daily sodium limit. When dining out, it is best to select low-sodium options or eat a half portion to limit the amount of salt. If some of your favorite foods are on this Salty Six list, don’t panic. Although these foods can be high in sodium, it isn’t necessary to cut these foods out of your diet completely. It’s just important to eat them in moderation and be mindful of your daily sodium intake. Look for low-sodium options, use herbs and spices instead of table salt and do your best to stay under the recommended daily limit of 1,500 milligrams.”
Read More About The Salty Six: Are High-Sodium Foods Increasing Your Stroke Risk?
-
Women and Heart Attacks: Subtle Signs to Know
Heart disease is the number one killer of women – claiming one life every minute – yet many women don’t know that the signs of heart attack may not be the same symptoms they’ve learned about all their lives. In women, nearly 71% experienced unusual exhaustion in the weeks before, 50% had trouble sleeping and 42% suffered shortness of breath. Most importantly, about 43% had no chest pain. Women and Heart Attacks: The Subtle Symptoms In both men and women, the most common symptom is pressure or pain in the mid chest, but there are also more subtle signs. “Women can experience a heart attack without chest pain,” explains Letitia Anderson, M.D., cardiologist with Renown Institute for Heart & Vascular Health. “It is not uncommon for women to experience extreme fatigue, shortness of breath, dizziness, lightheadedness, nausea, vomiting and pain in the abdomen or back as their primary symptom.” Other symptoms can include: Neck or jaw pain Fullness or pressure that goes away and comes back The feeling of a rope being tied around your body and squeezed Some doctors have reported seeing patients who just didn’t "feel right." One woman simply felt more tired than usual while cleaning, while another woman reported feeling winded carrying boxes to the basement. Admittedly these are symptoms many of us would shrug or sleep off versus going to the hospital for immediate care, which is why it’s important to pay close attention to the warning signs. “Women are good at being the caregiver for the rest of the family and writing off their own symptoms as something minor, like indigestion or a muscle pull,” says Dr. Anderson. “Remember that heart attacks have early warning signs, and if they are recognized and treated in time, a heart attack can be prevented and heart damage avoided.” When You Need to Call 911 Paying attention to your body is key. If you’ve experienced any unusual or flu-like symptoms, struggled to breathe or just don’t feel right – give yourself a gut check and ask if you’ve honestly felt this way before. If you’re worried at all, you need to seek emergency care. Do not wait – call 911 immediately Take an ambulance to the hospital if at all possible Try to stay calm and take deep, slow breaths until medical help arrives.
Read More About Women and Heart Attacks: Subtle Signs to Know
-
A Blood Test: What Valuable Clues It Tells Your Doctor
Blood. It can make you squeamish to think about it, yet every drop is vital to your health. In fact, a tiny vial of it can tell your doctor a wealth of information. We asked Benjamin Hansen, M.D., to explain what providers can learn from a blood test and why it’s important to get one as part of your annual checkup. CBC, the initials, sound innocent enough, right? In fact, when your favorite TV doctor orders a CBC, or complete blood count, it’s often the first step in getting an overall picture of your health. "It primarily measures white blood cells, red blood cells and platelets," explains Hansen. Although a blood test is one test you don’t have to study for, the measurements it takes can point to a host of information. What a Blood Test Says About Your Health White Blood Cell Count "The white blood cell count in your CBC helps us to determine the strength of your immune system," says Hansen. "It also helps us to determine the likelihood of infection because white blood cells fight off infection. Knowing the white blood cell count can also be helpful in patients with compromised immune systems, such as those on certain medicines or with conditions that impair immunity," he adds. White blood cells are made in your bone marrow and are alive only one to three days. Therefore, your body is constantly making them. Red Blood Cell Count "The red blood cells carry oxygen from your lungs throughout your body, while also carrying away waste. The hemoglobin (red blood cell protein) count is important because it helps us determine how well you're able to deliver oxygen from your lungs to the rest of your body," states Hansen. If these counts are low, you may have trouble breathing or experience fatigue. Red blood cells also grow in bone marrow, but they have a long lifespan – generally 100 to 120 days. Why Get a Blood Test? Although the CBC is just one type of blood test, according to the National Institutes of Health (NIH) there are a number of blood tests available that can help check for diseases and conditions such as: Heart disease Cancer Anemia (low iron) Diabetes High cholesterol Alcohol or Drug use disorder HIV/AIDS Additionally some tests show how well your kidneys, liver, heart and other organs are working. If you are taking a medication, a blood test can also let your provider know if it is helping you. What to Expect From a CBC Blood Test When you are not feeling well, it may take some detective work to figure out what is wrong and sometimes a CBC can be helpful. With this in mind, a lab order from your provider is needed to order a CBC blood test. Some blood tests require you to not eat food (fast) eight to 12 hours before the blood draw. Your provider will let you know the type of blood test(s) they are ordering for you. Usually it's important to drink plenty of water before your blood test, to make it easier to locate your veins. Generally a small sample of blood is taken from your arm vein and then sent to a lab for analysis. Discussing Your Results "A CBC can help your provider determine if there is an infection, your level of immunity, if you are anemic or if you are prone to bleeding," says Hansen. When to Get a Blood Test "A CBC is usually ordered for a specified purpose. If you think you might need a CBC, please call your provider. It's also important to see your provider regularly to keep an eye on your health. Many patients should see their provider at lease yearly," Hansen clarifies.
Read More About A Blood Test: What Valuable Clues It Tells Your Doctor
-
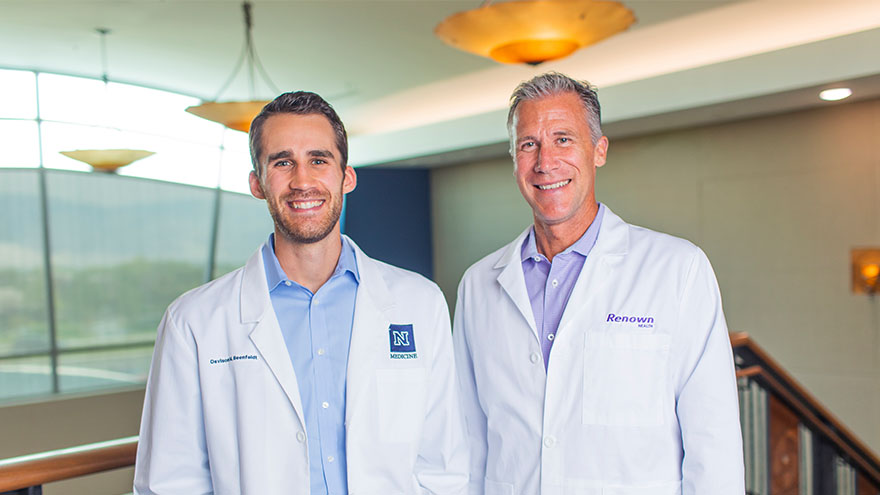
A Family's Legacy
Dr. Derek Beenfeldt first joined the Renown family in 2014 as a family medicine physician after graduating from University of Nevada, Reno, School of Medicine (UNR Med) in 2011. His son Davis was only 10 years old when Dr. Beenfeldt decided to change careers and attend medical school. Ten years later, Davis is following in his dad’s footsteps as a third year student at UNR Med. “I am proud of Davis for taking on the challenges and the commitment that I know goes along with attending medical school,” Dr. Beenfeldt said. “I also feel lucky that we have a medical school with such a great reputation and resources close to home.” The affiliation is a great source of pride for Dr. Beenfeldt. Not just because two important organizations in his life are joining forces, but he also sees it as both entities taking on an immense responsibility – the challenge to be better for incoming students, and subsequently to improve healthcare in Nevada. Davis is currently going through his rotations and spending countless hours a week at Renown Regional. His dad is right there by his side supporting him along the way. “It has been really interesting to have discussions about the UNR medical school with Davis, I recognize the names of many of the professors and courses from when I was a student,” Dr. Beenfeldt said. “I tried to be empathetic, as I can relate to how difficult and stressful this time is for him. Dr. Beenfeldt currently works as chief medical officer for Renown’s insurance arm Hometown Health, and Davis is still browsing specialties. “I don’t know what kind of medicine I want to focus on yet, but I feel lucky that I can attend medical school so close to home and have the option to continue helping my fellow Nevadans after I graduate.” UNR Med at a Glance UNR’s Medical School was established in 1969 Over the last 50 years, UNR Med has educated 3,900+ physicians More than 30% of UNR Med physician graduates continue to practice in Nevada UNR Med is the state’s oldest medical school
-
Bladder Control Treatment for Women – What’s Right for You?
Although going to the bathroom is not a typical conversation among women and their doctors, it’s an important one. It is a topic you may want to discuss with a urogynecologist, a physician who diagnoses, manages and treats pelvic health conditions in women. Kerac Falk, MD, a urogynecologist and assistant professor at the University of Nevada, Reno and Renown Health discusses overactive bladder in women and how to treat it. According to the National Institutes of Health, about 1 in 4 women struggle with pelvic health conditions, with over 40 percent of women over age 60 experiencing problems. While these conditions may be common, they shouldn’t just be accepted as a normal part of getting older. In fact, many women don’t think of urine leakage as a medical problem, and only 1 in 3 women with incontinence seek care. So, while these conditions may be common, they shouldn’t just be accepted as a normal part of getting older. There are excellent treatment options that can significantly improve the quality of life. Overactive Bladder Symptoms in Women: As your body changes and ages, so does your pelvic health. Whether you just had a baby, are experiencing urgency issues or find you cannot go about your daily routine, sneeze or laugh without leaking urine – you’re not alone. An overactive bladder, also known as OAB, is more than feeling an urgent need to go to the bathroom. It can also include the following: Incontinence or lack of control over urination Waking up in the middle of the night to empty your bladder Going to the bathroom often, even every 30 to 60 minutes Symptoms of OAB can lead to a decreased quality of life, feeling as if you cannot go about your normal daily routine, or even become hazardous, increasing the risk of trips, falls, and bone fractures. Various Treatments are Available: Behavioral management (eliminating coffee, soda and alcohol which irritate your bladder) Pelvic floor physical therapy to optimize nerve and muscular function and coordination to prevent leakage Medications including tablets and local estrogen replacement Pelvic nerve stimulation and reprogramming treatments Botox to relax the bladder muscle Solutions for an Overactive Bladder: Simply put, OAB is a nerve and muscle problem, so the bladder needs to calm down. Although there is no underlying reason for OAB, some underlying conditions may exist, such as: High blood pressure Recent trauma Neurological conditions (such as stroke and multiple sclerosis) Lifestyle and non-invasive measures can usually reduce symptoms by as much as 50%, significantly improving quality of life. However, if these measures do not help your OAB, further bladder testing may be needed. Dr. Falk notes that “every patient has a unique situation and set of symptoms. My job as a urogynecologist and pelvic floor subspecialist is to work as a team with each individual to figure out what’s going on and design the best treatment approach that fits your needs and goals, whether that is conservative or with more advanced procedures. The outcome we are working towards is improved quality of life.” If you are bothered by your bladder, the best thing you can do is bring this up with your primary care doctor or gynecologist to begin to discuss solutions
Read More About Bladder Control Treatment for Women – What’s Right for You?