Search
-
Know when to visit an ER: Top 5 concerns
When a sudden illness or injury occurs, the emergency room (ER) provides immediate medical attention to those in need. Understanding the top reasons for visiting the ER can help people make informed decisions about seeking emergency care. Here are the five most common reasons people in Nevada visited an ER in 2023. 1. Abdominal pain One of the top reasons people visit the ER is abdominal pain. The abdomen has many organs, including the stomach, liver, small and large intestines, gallbladder and pancreas. Significant pain in this area can be a cause of concern. Warning signs of a serious problem include abdominal pain with fever, vomiting, and not being able to move or perform everyday tasks due to pain. Seeking medical attention when experiencing these symptoms is essential. Emergency physicians can perform abdominal exams, assess the condition and rule out significant threats. 2. Fever High fevers that do not get better with medicine and are accompanied by other symptoms can cause concern. This can indicate that the body is fighting off an infection or illness. Fever with symptoms like vomiting, pain, altered mental status, shortness of breath or inability to perform daily functions are warning signs to watch out for. Adults and children should visit an ER, where the team can assess the causes of the fever. 3. Chest pain and shortness of breath Chest pain and discomfort, or pain in the upper body can suggest warning signs of a heart attack. If a person is experiencing signs of a heart attack, call 911 immediately to ensure timely treatment or assessment by a medical professional. Heart attack symptoms include: Chest pain, including pain that can be described as chest pressure, heaviness or squeezing Discomfort in the chest, arms, back, neck, shoulders and jaw Difficulty breathing Sweating with any of the above symptoms When visiting a Renown ER for chest pain, a trained medical professional will promptly perform an Electrocardiogram (EKG) in an area where preliminary assessments, also known as triage, take place. Individuals experiencing shortness of breath or trouble breathing, whether from a respiratory infection, asthma complications or other pre-existing conditions should not ignore symptoms as these can signify more serious issues. Warning signs of respiratory distress may include: A significant change in breathing rate A significant change in the amount of energy used to inhale or exhale when breathing Changing of the skin color to blue, gray or paleness, which can indicate a lack of oxygen Nasal flaring Chest retractions, which can suggest difficulty bringing air into the lungs What this looks like: the chest sinking in just below the neck, breastbone or rib cage while breathing 4. Neurological symptoms Sudden and severe headaches or seizures may prompt individuals to visit the ER if symptoms are extremely disorientating or debilitating. These symptoms could be indicative of various conditions, including strokes or neurological disorders that require prompt evaluation. If a person is experiencing signs of stroke, call 911 immediately to ensure timely treatment. Stroke symptoms include: Numbness, weakness or loss of movement in the face, leg or arm, especially on one side Confusion, including trouble speaking or understanding Trouble with vision or loss of balance When choosing emergency care for signs and symptoms of stroke, a Comprehensive Stroke Center can provide patients with immediate intervention, including evaluation, treatment and education. 5. Cough/flu-like symptoms Emergency departments are staffed by medical professionals trained to prioritize and treat emergency and trauma situations. Receiving care at an ER should be reserved for severe symptoms and life-threatening conditions. It’s best to schedule a visit with a primary care physician for mild cold and flu symptoms. Most urgent care locations are equipped with rapid testing options, including RSV, COVID-19, influenza, mononucleosis, urinary issues and strep throat. It is critical to distinguish between common respiratory infections and more severe cases, such as pneumonia or complications from the flu. Symptoms that may warrant a visit to the ER include: Rapid decline in the ability to perform regular daily activities Coughing or throwing up blood Severe dehydration and inability to drink fluids High fever not responsive to medication Understanding top ER visits in Nevada While these ER complaints are common reasons for emergency room visits in Nevada, it's important to remember that emergency care is available for all immediate medical needs. Do not hesitate to seek help at an emergency room if someone experiences a sudden or severe health concern. Quick and appropriate action can make a significant difference in keeping you and your loved ones healthy. Renown Health is the largest locally governed, not-for-profit healthcare network in northern Nevada, providing leading emergency and trauma care by board-certified emergency physicians 24/7 at three locations, including the region’s only pediatric emergency department. Renown Health emergency rooms prioritize swift assessments, advanced diagnostic tools and compassionate care, providing leading emergency and trauma care. Trust Renown ER for not just emergency care but exceptional care. Learn more at renown.org/ER.
-
Most Common Reasons Women Visit the ER
If you or someone you know is experiencing a medical emergency, it's essential to seek immediate attention by calling 9-1-1 or visiting the ER for a thorough evaluation by a trained medical professional and timely intervention. Access to a convenient and trusted emergency room (ER) is critical to any person’s healthcare needs, including medical emergencies related to women’s health. We explored some common scenarios and warning signs prompting women to seek immediate medical attention with Aiden Gould, Board-Certified Emergency Physician at Renown Health. When your medical emergency can’t wait, Renown ER is here to provide you with the region’s leading emergency care to diagnose and treat your condition or illness. Understanding Common Reasons Women Visit the Emergency Room Gynecological Emergencies: One of the most common reasons women may seek emergency care is due to gynecological emergencies such as severe pelvic pain, abnormal bleeding or complications related to pregnancy. These issues can be alarming and warrant immediate medical attention if the issue persists or is out of the ordinary for you. Emotional and Physical Well-Being: For those facing diverse medical or mental health emergencies, seeking prompt assistance is crucial for a thorough assessment and safe, timely intervention. Renown ER teams are equipped with trained professionals who provide compassionate care for individuals seeking help in the following situations: Suicide risk assessment and intervention Substance abuse assessment Assault and trauma care Crisis support and intervention Resources for ongoing care and well-being support Severe Abdominal Pain: Unexplained and severe abdominal pain that is substantially different than what is normal for you is a symptom you should never ignore as it can indicate underlying issues. Warning signs of an acute medical situation include fever, vomiting or a rapid change in motor function and inability to move due to pain. Respiratory Distress: Difficulty breathing, persistent coughing and other respiratory issues can be especially concerning. Women with pre-existing respiratory conditions like asthma or those experiencing sudden respiratory distress should seek immediate care from a medical professional. Warning signs of respiratory distress may include a significant change in one’s breathing rate, changing of the skin color to blue, gray or paleness due to lack of oxygen, nose flaring and chest retractions. Cardiovascular Emergencies: Heart-related issues are not exclusive to men. Women can also experience cardiovascular emergencies that often go undiagnosed because symptoms differ from men. Symptoms like chest pain, extreme fatigue, vomiting or pain in the abdomen, shortness of breath or palpitations should be evaluated by an emergency medical professional as timely intervention is critical in such cases. Renown leads the region in cardiology care with our technological expertise and patient-centered approach. Our comprehensive team diagnoses heart disease and other cardiac conditions, offering personalized treatment plans. Neurological Symptoms: Sudden and severe headaches, seizures or other neurological symptoms may prompt women to visit the ER if symptoms are extremely disorientating or debilitating. These symptoms could be indicative of various conditions from mild to severe, including strokes or neurological disorders that require prompt evaluation. Renown Regional Medical Center is a Comprehensive Stroke Center, providing primary stroke care including evaluation, treatment and education to patients who arrive at a Renown facility with the signs and symptoms of a stroke. Compassionate Care in Times of Need At Renown Health, we understand that your time is valuable, especially in emergency situations. That's why we strive to provide patients with exceptional care, compassion and respect. Plan ahead and make informed decisions about seeking medical care by viewing your estimated triage wait time at a Renown ER.
-
What to Expect at a Renown Health ER
Access to a trusted and efficient emergency room (ER) in times of unexpected medical emergencies is crucial. Renown Health’s emergency and trauma care is available at three ER locations, including the region’s only level II trauma center and ER designed for pediatric patients to provide you and your family with prompt, high-quality and specialized care by board-certified emergency physicians when you need it. Dr. John Hardwick, board-certified emergency physician at Renown Health, describes a guide to emergency care at Renown Health below. Timely and Compassionate Care: Renown ER is committed to delivering timely and compassionate care. Experienced medical professionals at Renown will communicate openly with you, involving you in the decision-making process and addressing any concerns you may have. Upon arrival, you can expect to be promptly assessed by a team of skilled medical professionals who will prioritize your needs based on the severity of your illness or condition. Click here to learn more about the emergency care process, from check-in to discharge. Expert Medical Team: With advanced technology and experienced specialists from Northern Nevada Emergency Physicians, all patients are in good hands for emergency care at Renown Health. Our pediatric and adult emergency physicians have completed fellowship training in specialty areas such as sports medicine, ultrasound and emergency medical services. Team members in the emergency department will ensure you are informed and as comfortable as possible during your visit to minimize any pain or discomfort you may feel. Efficient Triage Process: Renown ER utilizes an efficient triage process to prioritize patients based on the urgency of their medical condition. This ensures that those with more critical conditions receive immediate attention, while still providing timely care for others. Tests such as labs or diagnostic services will often be completed while you wait to see a physician to expedite the process. Comprehensive Diagnostic Services: The ERs at Renown offer comprehensive diagnostic services to quickly identify your symptoms. This may include X-rays, laboratory tests, CT scans and other imaging studies, helping emergency physicians make informed decisions about your treatment plan. Specialty Care and Collaboration with the Renown Health Network: We offer the area's largest network of specialized providers and services to help ensure you receive industry-leading, personalized care during and after your emergency room visit. This collaboration means you’ll have access to more specialists and a wide range of expertise to continue your care without leaving the Renown Health network. State-of-the-Art Facilities: Renown Health invests in state-of-the-art facilities and equipment to ensure that patients receive the best possible care. Renown ERs are equipped with modern medical technology, allowing board-certified emergency physicians to diagnose and treat a wide range of medical conditions. Post-ER Visit Support and Resources: Your experience with Renown Health doesn't end when you leave the ER. Our team will address your questions and provide you with post-visit instructions, medications and follow-up recommendations to continue your care. With a commitment to timely and compassionate care and a team of expert healthcare professionals, you can trust Renown ER to provide the highest standard of emergency medical services when you need it most.
-
Strategies for Lasting Weight Loss
Managing weight is a complicated and often difficult journey for many individuals, and obesity stands as a common and serious chronic health condition. In fact, the Center for Disease Control and Prevention reports that the prevalence of obesity in the US is greater than 40% in adults and 20% in children, and those numbers are continuing to climb. In Nevada, according to the 2020 Behavioral Risk Factor Surveillance System, 28.7% of adults reported being obese. By 2030, almost 80% of American adults may be overweight and half of them will be obese. But obesity isn't just about the numbers on the scale; it's a multifaceted, lifelong, neurobehavioral disease triggered by a combination of factors. These include abnormal eating patterns, reduced physical activity levels, environmental stressors, genetics and various other contributors. Obesity extends far beyond appearance, often leading to the development of numerous medical conditions such as diabetes, heart disease, elevated blood pressure, stroke, sleep apnea, liver disease, various cancers and infertility. Join us as we delve into the complexities of obesity and explore strategies for effective weight management available right here in northern Nevada. Why Can Losing Weight be so Difficult? The challenge behind weight loss finds its roots in the Set-Point Theory of Obesity, a concept that says our bodies have a predetermined weight, or fat mass, within a defined set-point range. In other words, when an individual's weight deviates from this set point, the body initiates mechanisms to bring it back to the established range. So, if someone loses weight below their set point, the body may respond by increasing hunger and reducing metabolism, making it challenging to sustain weight loss. There Isn’t One Right Answer, But Renown is Here to Help Various weight management strategies can be utilized by patients struggling with obesity, which may lead to substantial weight loss, resolution of associated medical conditions and improved psychosocial health. In fact, the most successful strategy involves a multidisciplinary approach under the guidance of trained specialists that includes a combination of tactics, including: Behavioral adaptations Dietary modifications Physical exercise Anti-obesity medications Weight loss surgery
-
Sepsis: Causes & Symptoms
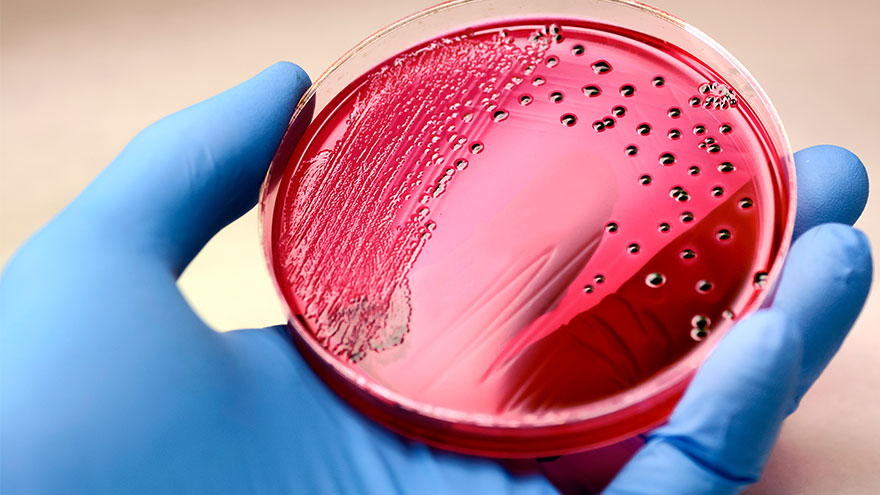
According to the Global Sepsis Alliance, 1 in 5 deaths worldwide are associated with sepsis. If not recognized early and treated promptly, sepsis is the final common pathway to death from most infectious diseases worldwide, including viruses such as COVID-19. We spoke with Jeremy Gonda, MD, a critical care physician from Renown Health’s Sepsis Committee to increase public awareness of this preventable medical emergency. What is sepsis? Sepsis is a response to infection—bacterial, viral or fungal—and can start anywhere in the body and spread into the bloodstream. The body is trying so hard to fight an infection that it begins releasing chemicals into the bloodstream that cause inflammation and the shutdown of multiple organ systems. “It carries a very poor prognosis in general unless you catch and treat it very early,” said Dr. Gonda. “Any infection can lead to sepsis. Typically your immune system takes care of the infection. It doesn’t progress, but in cases where the infection becomes severe, or the immune system doesn’t function properly, people can certainly die. So there’s, unfortunately, a very high mortality rate associated with sepsis.” According to the Centers for Disease Control and Prevention, each year at least 1.7 million adults in America develop sepsis. While you can recover from sepsis if caught early, many sepsis survivors suffer from long-term physical and psychological effects. What are the signs of sepsis? One way to spot sepsis is to use the acronym SEPSIS: S – Slurred speech and confusion E – Extreme shivering or muscle pain/fever P – Passing no urine all day S – Severe breathlessness I – “I feel like I might die” S – Skin mottled or discolored Keep in mind that sepsis symptoms can vary depending on where the infection starts. “Patients may experience urinary burning if they have a urinary tract infection or a cough and shortness of breath if they have pneumonia first,” said Dr. Gonda. “However, often symptoms are more generalized or subtle such as fevers, confusion and malaise.” How do you develop sepsis? When germs enter your body, they can cause an infection. If you don’t stop that infection, it can cause sepsis. Areas of infection that more commonly result in sepsis include: Lungs, such as pneumonia Kidney, bladder and other parts of the urinary system Digestive system Bloodstream (bacteremia) Catheter sites Wounds or burns Who is most at risk? People with compromised immune systems are at greater risk for sepsis, such as “The very young, the elderly and any people who may have conditions that suppress your immune system,” said Dr. Gonda. “For instance, if you have diabetes or if you’re an organ transplant patient who is on immunosuppressant therapy, you’re at somewhat higher risk.” Sepsis is often considered a hospital-acquired infection, but a study in The Journal of American Medical Association found that 80% of sepsis cases occur outside of a hospital. That’s why it’s especially important to remember any infection can lead to sepsis, and anyone can develop sepsis from an infection. What do I do? Timing is critical in the case of sepsis and septic shock. According to a study on septic shock patients, there is a 7.6 percent decrease in survival for each hour treatment is delayed. On the other end, if treatment is given within an hour of the first drop in blood pressure, the survival rate is 80 percent. Because sepsis can be so deadly, it’s important to seek medical attention as soon as possible. “If you’re not getting any better, if you think symptoms are progressively worsening – you should definitely be evaluated by a doctor,” said Dr. Gonda. You can help #StopSepsis by getting involved at worldsepsisday.org.
-
Head Injuries, Sprains and Broken Bones
Participating in sports and physical activities is enjoyable and beneficial for our health. However, the risk of injuries comes with the fun and excitement of sports. Sports-related injuries, including sprains, traumatic brain injuries and broken bones, are more common than we realize and can land you in the emergency room. Dr. Scott Shepherd, Emergency Medicine Physician, provides a wealth of information. Traumatic Brain Injuries: The Invisible Threat Traumatic brain injuries come in many forms. From “mild” brain injuries, concussions, to major brain injuries and bleeds. Sometimes it is very difficult to tell the difference between a major injury and a minor injury because many of the symptoms are the same. Concussions Concussions are a type of “mild” traumatic brain injury resulting from a blow to the head or a violent shaking of the body that causes a transient alteration in mental function. They are particularly prevalent in contact sports such as football, soccer and boxing. A concussion can affect memory, judgment, reflexes, speech, balance and muscle coordination. Typically, concussions are not life threatening and usually short lived. However, multiple concussions can lead to permanent disabilities. So, remember there is nothing “mild” about injuring your brain. Contusions The more serious brain injuries from brain contusions (actual bleeding in the brain material) and bleeding that presses on the brain are life threatening. These injuries are caused by the same blow to the head as a concussion and the symptoms are the same from memory deficits, loss of coordination to coma. Because of this, anyone who has a blow to the head and is not acting normal should be evaluated by a medical professional. Anyone suspected of having a severe head injury should seek immediate medical attention and follow a strict protocol for rest and a gradual return to play. It is important to note a person may not lose consciousness if they suffer a concussion; however, major consequences can occur if not properly managed. If you suspect you have an emergency that needs immediate medical attention, please call 911 or visit an emergency room near you. While it is impossible to prevent traumatic brain injuries altogether, the severity of the injury can be mitigated through proper helmet usage and knowing your skill level when participating in high-risk activities. The guidelines for picking a helmet for summer activities such as mountain biking, dirt biking and riding off highway vehicles are similar to those of picking a helmet for winter sports. Learn more about choosing the right helmet. Any blow to your head, neck or upper body can result in a major head injury Signs to watch for include the following: Headache Dizziness Blurred vision Difficulty with thinking, attention or memory Sensitivity to noise or light Ringing in the ears Changes in hearing Double vision Changes in behavior Balance issues Nausea/vomiting Sprains: The Annoying Twist One of the most common sports injuries is a sprain, which occurs when ligaments that connect bones are stretched or torn. Sprains typically occur in joints, such as the ankle, knee or wrist, and are often caused by sudden twists or impacts. Symptoms may include: Pain Swelling Bruising Limited range of motion Rest, ice, compression and elevation (RICE) are the initial recommended treatment, followed by physical therapy to regain strength and mobility.
-
What it Means to be a Level II Trauma Center
When the sudden need for emergency or critical care arises, the level of a trauma center is an important designation that helps explain the types of resources available. Renown Regional Medical Center is proud to be the only Level II Trauma Center in our region, which is a critical service to provide. We spoke with Bret Frey, MD, an emergency care physician, to discuss what this means for our community. Requirements for Designation as a Level II Trauma Center To be a designated Level II Trauma Center, a hospital must have 24-hour immediate coverage by general surgeons and multiple specialties, such as orthopedic surgery, neurosurgery, emergency medicine and more. In addition, this hospital must provide trauma prevention and ongoing education for its teams and incorporate a comprehensive quality assessment program. “What it means for this community is nothing short of amazing,” said Dr. Frey, who explained that Renown has over 20 specialty physicians on-call and ready to provide trauma care. According to Dr. Frey, many communities of the same or larger size have fewer specialists ready and available to provide this level of care. Renown Regional Medical Center is located near downtown Reno. The Emergency Department has several helipads and ambulance banks to intake patients requiring emergency care. Patients can also receive emergency walk-in care. On the same campus is Renown Children’s Hospital, which is home to the only pediatric Emergency Room dedicated solely to pediatric patients. Emergency and trauma care is just one area in which Renown Health is the regional leader. When patients or families choose Renown during an emergency, they will have access to all the resources provided through the entire health network. This means access to the many specialists available to consult on different conditions or care situations, inpatient care if needed, referrals to other areas of the network and medications to go. “I’m very happy and proud to be a part of building something very special in this community,” said Frey.
Read More About What it Means to be a Level II Trauma Center
-
What to do if you Experience a Summer Burn
As families spend more time outdoors to enjoy the summer temperatures, it's important to be aware of potential hazards that can lead to burns – be it sunburns, burns sustained while grilling or navigating the hot surfaces often found around pool decks and parks. All these burn types are not only painful but can also cause severe damage to the skin and require immediate medical attention. Ross Albright, MD, an emergency care physician, explores effective preventive measures to avoid burns during the summer and discusses when it's essential to seek medical care. Stay Sun Safe While soaking up the sun is a favorite summer pastime for many, it's important to protect your skin from harmful ultraviolet (UV) rays. Sunburns not only damage the skin but also increase the risk of more severe burns. Follow these tips for staying safe in the sun: Apply broad-spectrum sunscreen with a minimum SPF of 30 before heading outdoors and reapply every two hours. Seek shade during peak hours of sun intensity, typically between 10 a.m. and 4 p.m. Wear protective clothing, such as wide-brimmed hats, sunglasses and lightweight, long-sleeved garments. Fire and Hot Object Safety Summer is full of fun outdoor activities like BBQs, campfires and fireworks, all of which can pose a fire hazard if not handled carefully. To prevent burns caused by fires: Maintain a safe distance from open flames and grills and always use oven mitts or potholders when handling hot objects. Keep a fire extinguisher and a first aid kit readily available. Keep children away from hot objects and fireworks and educate them about the dangers of touching or playing with them. Hot Surface Safety Asphalt, metal slides and surfaces around the pool retain heat and are likely to be significantly hotter than other materials such as a wooden picnic table to grassy pathway (these can still be hot too!). So, it's crucial to be cautious around these materials to prevent burns: Use caution when near hot surfaces surrounding water sources, such as pool decks or metal slides. Always wear shoes when walking on hot surfaces such as asphalt, concrete and even sand. Ensure that playground equipment such as slides and swings are cool to the touch before your kiddos start climbing around. Recognizing Severity of Burns and Seeking Care Despite our best efforts, burns can still occur. It's essential to know when a burn requires medical attention: First-degree burns, characterized by redness, pain and minor swelling, can typically be treated at home with cool water and over-the-counter pain relievers such as ibuprofen (Advil or Motrin) or acetaminophen (Tylenol). Second-degree burns, which may cause blistering and more intense pain, should be evaluated by a healthcare professional. Third-degree burns, indicated by charring or blackened skin, deep tissue damage or burns that cover a large area, require immediate emergency care. Preventing burns during the summer is paramount to enjoying a safe and enjoyable season. By following these tips, you can significantly reduce the risk of burns and ensure prompt medical attention when necessary. Stay informed, stay safe and have a burn-free summer! If you or someone you know experiences a burn, it's important to seek immediate medical care.
-
When to Seek Care for Abdominal Pain
Abdominal pain is one of the most common complaints that brings individuals to the emergency room. We spoke with emergency physician Bret Frey, MD, to ask about when and where to seek care for abdominal pain. Dr. Frey advises that any time you feel something is developing inside your body that is substantially different from what is normal for you, understand that something is wrong. He further explains that warning signs of an acute medical situation include fever, vomiting or a rapid change in function and ability to move due to pain. These symptoms indicate that one needs to be evaluated by a medical professional. This evaluation will include the care team conducting an examination and asking a series of questions to determine if additional diagnostics, such as lab work or imaging, are needed. Be prepared to discuss where the pain is and what it feels like, in addition to how long it’s been bothering you and if it’s constant or intermittent. While appendicitis often comes to mind when thinking about abdominal pain, Dr. Frey says that this is not the bulk of cases that the Emergency Department sees. In fact, often the pain does not have a specific diagnosis, but our team of board-certified emergency physicians are experienced in assessing and caring for those experiencing the acute symptoms he described. “We often don’t come away with an answer about exactly what it is, but we substantially rule out life threats in a very methodical and systematic way,” said Frey. The abdomen includes many organs, including the stomach, liver, small and large intestines, gallbladder and pancreas. In addition, pain stemming from your chest, pelvis or back may be felt in the abdominal area. If you are experiencing abdominal issues that are persistent but not an emergency, talk to your primary care doctor about what you are experiencing, and be prepared to review the history of this pain, medications, allergies and diet. He or she will be a good partner to review conditions such as gas, heartburn, constipation, diarrhea, inflammation or menstrual and ovulation pain. Drinking plenty of water is always an important part of supporting your health.
-
Importance of Safe Sleep
In today's fast-paced society, it is understandable for parents to want to take shortcuts in caring for their little ones. A s a result, It is tempting to leave a sleeping infant in a car seat or swing after a long day of errands or when you need a moment to catch your breath. But, as convenient as these devices may be, they pose a serious risk to your child's safety. Why Car Seats and Swings Pose Risks for Infant Sleep Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The American Academy of Pediatrics (AAP) states that “infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical.” If a parent must use a car seat or other sitting device, they should only do so for a short period of time and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The American Academy of Pediatrics (AAP) warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. This is because infants can easily slump over or become entangled in the straps, blocking their airway, and causing suffocation. Car seats, swings, and bouncers are quick and convenient ways to feed, hold, and sleep an infant. Not out of malice or discontent, but again from the need for quick and easy access to baby care in an already busy lifestyle. However, the risks outweigh the benefits. The AAP states: Infants should be moved to a crib, bassinet, or play yard for sleeping as soon as is practical. If a parent must use a car seat or other sitting device, they should only do so for a short period and never as a substitute for a proper sleeping environment. Leaving a sleeping infant in a sitting device, such as a car seat or swing, can create unsafe sleeping conditions. The AAP warns that doing so increases the risk of sudden infant death syndrome (SIDS) and positional asphyxia. In addition, infants can easily slump over or become entangled in the straps, blocking their airways and causing suffocation.
-
What to Expect at a Well Child Checkup
A well-child checkup is a great opportunity to monitor your child’s growth and development, and it's also a chance to establish a trusting relationship with your child’s pediatrician and have your questions answered. What to Expect at Each Checkup At every checkup, a comprehensive physical examination will be conducted to assess your child's growth parameters, including height, weight and head circumference. A developmental assessment will evaluate the progress of your infant or young child in achieving age-appropriate milestones, encompassing language skills, motor development, problem-solving abilities and psycho-social skills. In addition, your pediatrician will address common concerns such as feeding, sleep patterns, oral health and general infant care. Unless there are specific needs or concerns for your baby, routine laboratory tests are typically unnecessary. Your pediatrician will provide guidance on immunization schedules, post-vaccination expectations and when to seek medical attention. Furthermore, during each visit, you will receive age-specific guidance to help you anticipate your child's expected growth and development, along with essential safety precautions and illness prevention measures. Your pediatrician will discuss various topics, such as placing your baby to sleep on their back, utilizing rear-facing infant car seats until around age two, maintaining home water thermostats below 120 degrees Fahrenheit, ensuring dangerous objects and poisonous substances are out of sight and reach, emphasizing dental health and promoting the use of bike helmets, among other things. Preparing for Your Visit It is recommended that, as a parent, you write down any questions beforehand, so you don’t forget them in the moment. Most importantly, feel comfortable asking your pediatrician about anything that might seem unusual, as you are the parent, and you know best! Before leaving the pediatrician’s office, be sure that you fully understand any instructions given to you and ask for clarification if needed. From your child’s birth through young adulthood, you will be visiting your pediatrician regularly. The American Academy of Pediatrics provides what a regular schedule might look like. Well-Child Checkup Schedule Two to three days after birth and at one month Two months Four months Six months Nine months One year 15 months 18 months 24 months 30 months Three years, and yearly after
-
10 Essential Questions to Ask at Your Child's Pediatrician Visit
Taking a few minutes to prepare for your child's pediatrician visit helps ensure that all your child's medical needs are met. Knowing the right questions to ask your provider can help you get the most out of your visit and ensure you and your child feel comfortable and informed. It is essential to base your questions on your child's specific health needs, but the ten options below are a great place to start. How is my child's overall health and development progressing? Is my child meeting their developmental milestones, and are there any areas where they may need extra support? What vaccinations does my child need, and are they up to date on all required immunizations? Are there any nutritional recommendations or concerns for my child's age and stage of development? What are some strategies for promoting healthy habits and physical activity for my child? Are there any warning signs I should look out for regarding my child's health or behavior? What can I do to help prevent common childhood illnesses like colds, flu strains or ear infections? What should I do if my child gets sick, and when should I seek medical attention? Are there any changes to my child's medication or dosage that I should be aware of? Is there anything else I should know or be aware of regarding my child's health or development?
Read More About 10 Essential Questions to Ask at Your Child's Pediatrician Visit






.jpg?rev=f89fdc95b1824f868e98988928b0a6bb)



